Comparative analysis of four scoring systems in predicting the short-term prognosis of patients with traumatic brain injury
-
摘要:
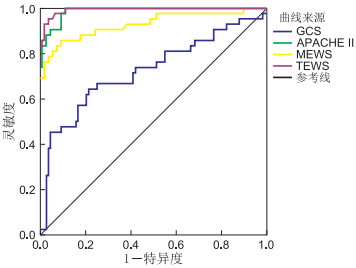
目的 探讨4种常用的评分方式对颅脑外伤(TBI)患者病情预后评估分效能。 方法 选择2017年1月—2018年6月温州医科大学附属第二医院接诊的TBI患者149例,按照患者入院后28 d时预后将所有患者分为预后良好和预后不良2种情况。分析2组患者入院时一般资料并根据格拉斯哥昏迷指数(GCS)、急性生理学及慢性健康状况评分(APACHEⅡ)、改良早期预警评分(MEWS)和分流早期预警评分(TEWS)对患者入院时状态进行评分,而后采用logistic回归分析判断影响患者预后的因素,并使用ROC曲线评价4种评分对患者预后的预测效能。 结果 患者出院时预后不良例数为42例,预后不良率为28.18%。预后良好患者颅内出血率、GCS、APACHEⅡ、MEWS、TEWS均显著低于预后不良患者,伤情显著优于预后不良患者(均P < 0.05)。APACHEⅡ、MEWS及TEWS为影响患者预后的独立危险因素。ROC分析结果显示,APACHEⅡ及TEWS对TBI患者预后的AUC显著大于MEWS(均P < 0.05),APACHEⅡ及TEWS对TBI患者预后的AUC比较差异无统计学意义(P>0.05)。 结论 TWES与APACHEⅡ对于TBI患者预后均有较好的预测效能,但TWES预测阳性可信度较好,可以将之运用于TBI患者入院时评估中。 Abstract:Objective To investigate the efficacy of four scoring methods in evaluating the prognosis of patients with traumatic brain injury (TBI). Methods A total of 149 patients with TBI who were admitted to the Second Affiliated Hospital of Wenzhou Medical University from January 2017 to June 2018 were selected. According to the prognosis at 28 days after admission, all patients were divided into two types: good prognosis and poor prognosis. The general data of the two groups of patients at admission was analyzed and the patients' admission status was scored based on the Glasgow Coma Index (GCS), Acute Physiology and Chronic Health Status Score (APACHEⅡ), Modified Early Warning Score (MEWS), and Triage Early Warning Score (TEWS). Then logistic regression analysis was used to determine the factors affecting the prognosis of the patients, and the ROC curve was used to evaluate the predictive power of the four scores on the prognosis of the patients. Results The number of patients with poor prognosis at the time of discharge was 42, and the poor prognosis rate was 28.18%. The intracranial hemorrhage rate, GCS, APACHEⅡ, MEWS, and TEWS of patients with good prognosis were significantly lower than those with poor prognosis, and the injuries were significantly better than those with poor prognosis (all P < 0.05). The APACHEⅡ, MEWS and TEWS were the independent risk factors that affect the prognosis of patients (all P < 0.05). The results of ROC analysis showed that the prognosis of APACHEⅡ and TEWS for TBI patients were significantly greater than that of MEWS (both P < 0.05), and the prognosis of APACHEⅡ and TEWS for TBI patients were not significantly different (P>0.05). Conclusion Both TWES and APACHEⅡ have better predictive power for the prognosis of TBI patients, but the positive predictive reliability of TWES is good, and they can be used in TBI patients' admission evaluation. -
Key words:
- Warning score /
- Traumatic brain injury /
- Prognosis /
- Predictive analysis
-
表 1 2组TBI患者一般资料中影响预后情况的单因素分析
自变量 例数 年龄(岁) 性别 BMI 吸烟史[例(%)] 颅内出血[例(%)] GCS(分) APACHEⅡ(分) MEWS(分) TEWS(分) 男性 女性 预后良好组 107 38.14±9.51 67 40 22.14±2.94 59(55.14) 11(10.28) 7.32±1.71 15.82±4.35 1.64±0.51 3.79±1.03 预后不良组 42 41.55±10.12 24 18 22.88±3.01 27(64.29) 17(40.48) 8.98±1.99 27.05±5.13 3.04±1.09 6.91±1.79 统计量 -1.881a 0.380b -1.359a 1.033b 18.021b 4.731a -13.463a -11.190a -13.304a P值 0.063 0.537 0.178 0.309 < 0.001 < 0.001 < 0.001 < 0.001 < 0.001 自变量 例数 损伤至入院时间(h) 基础疾病[例(%)] 伤情[例(%)] 损伤原因[例(%)] 高血压 糖尿病 轻 中 重 交通事故 坠落伤 重物砸伤 其他 预后良好组 107 5.63±2.13 34(31.78) 21(19.63) 29(27.10) 59(55.14) 19(17.76) 67(62.62) 20(18.69) 13(12.15) 7(6.54) 预后不良组 42 6.42±3.09 17(40.48) 12(28.57) 5(11.90) 12(28.57) 25(59.52) 20(47.62) 11(26.19) 7(16.67) 4(9.52) 统计量 -1.708a 1.014b 1.399b 19.407c 2.798b P值 0.076 0.313 0.236 < 0.001 0.423 注:a为t值,b为χ2值,c为Z值。 表 2 2组TBI患者实验室指标中影响预后情况的单因素分析(x±s)
组别 例数 AST(U/L) ALT(U/L) Cr(mmol/L) BUN(mmol/L) TC(mmol/L) WBC(×109/L) PLT(×109/L) 预后良好组 107 56.73±18.34 40.67±13.45 99.25±21.47 15.07±4.23 2.44±0.65 9.79±1.42 157.69±34.51 预后不良组 42 61.21±21.13 45.34±19.12 93.74±19.51 16.54±5.02 2.51±0.84 10.02±1.97 147.54±30.17 t值 -1.207 -1.448 1.506 -1.678 -0.458 -0.689 1.772 P值 0.231 0.152 0.135 0.098 0.628 0.493 0.079 表 3 影响患者预后的logistic回归分析
变量 B SE Wald χ2 P值 OR值 95% CI 颅内出血 1.745 2.629 3.259 0.071 5.725 -0.097~6.502 GCS 0.256 0.586 0.191 0.662 1.291 0.147~4.073 APACHEⅡ 1.453 0.249 3.946 0.026 4.275 2.371~7.982 MEWS 1.097 1.799 3.539 0.041 2.955 1.043~9.578 TEWS 1.082 2.595 3.933 0.027 2.951 1.641~6.584 伤情 轻度 -4.547 4.812 0.893 0.345 0.011 0.000~132.180 中度 -2.707 2.196 1.520 0.218 0.067 0.001~4.935 常数 -25.045 17.262 2.105 0.147 -25.045~0.000 表 4 4种评分方式对患者预后的预测价值分析
评分方式 截点值 SE P值 AUC 95% CI GCS 8 0.051 < 0.001 0.722 0.622~0.823 MEWS 2 0.028 < 0.001 0.892a 0.873~0.962 APACHEⅡ 21 0.006 < 0.001 0.987ab 0.975~0.999 TEWS 5 0.004 < 0.001 0.993ab 0.986~1.000 注:与GCS比较,aP < 0.05;与MEWS比较,bP < 0.05。 表 5 4种评分方式灵敏度、特异度、阳性预测及阴性预测值情况(%)
评分方式 灵敏度 特异度 阳性预测值 阴性预测值 GCS 64.29 78.51 54.00 84.85 MEWS 85.71 90.65 78.26 94.17 APACHEⅡ 97.61 88.78 77.36 98.95 TEWS 95.23 96.26 90.90 98.90 -
[1] NORDSTRÖM A, NORDSTRÖM P, et al. Traumatic brain injury and the risk of dementia diagnosis: A nationwide cohort study[J]. PLoS Med, 2018, 15(1): e1002496. doi: 10.1371/journal.pmed.1002496 [2] EDLOW B L, CHATELLE C, SPENCER C A, et al. Early detection of consciousness in patients with acute severe traumatic brain injury[J]. Brain, 2017, 140(9): 2399-2414. doi: 10.1093/brain/awx176 [3] 冯金周, 刘发健, 匡永勤, 等. PCA-Logistic回归模型预测颅脑损伤患者临床预后的应用研究[J]. 中华神经医学杂志, 2018, 17(12): 1234-1240. doi: 10.3760/cma.j.issn.1671-8925.2018.12.008 [4] BRENNAN P, MURRAY G, TEASDALE G M. Simplifying the use of prognostic information in traumatic brain injury. Part 1: The GCS and Pupils Score: An Extended Index of Clinical Severity[J]. J Neurosurg, 2018, 128(6): 1612-1620. doi: 10.3171/2017.12.JNS172780 [5] SERVIÁ L, BADIA M, MONTSERRAT N, et al. Severity scores in trauma patients admitted to ICU. Physiological and anatomic models[J]. Med Intensiva, 2019, 43(1): 26-34. doi: 10.1016/j.medin.2017.11.008 [6] CHURPEK M M, CAREY K A, DELA MERCED N, et al. Validation of early warning scores at two long-term acute care hospitals[J]. Crit Care Med, 2019, 47(12): e962-e965. doi: 10.1097/CCM.0000000000004026 [7] CARNEY N, TOTTEN A M, CINDY O'REILLY, et al. Guidelines for the Management of severe traumatic brain injury, Fourth Edition[J]. Neurosurgery, 2017, 80(1): 6-15. doi: 10.1227/NEU.0000000000001432 [8] WAGNER A K, HAMMOND F M, GRIGSBY J H, et al. The value of trauma scores: predicting discharge after traumatic brain injury[J]. Am J Phys Med Rehabiln, 2000, 79(3): 235-242. doi: 10.1097/00002060-200005000-00004 [9] LEE S B, KIM D H, KIM T, et al. Triage in emergency department early warning score (TREWS) is predicting in-hospital mortality in the emergency department[J]. Am J Emerg Med, 2019, S0735-6757(19): 30082-30088. http://www.onacademic.com/detail/journal_1000041580712299_a5cd.html [10] WANG Y, WEN L, YOU W, et al. Predicting the outcomes of shunt implantation in patients with post-traumatic hydrocephalus and severe conscious disturbance: a scoring system based on clinical characteristics[J]. J Integr Neurosci, 2020, 19(1): 31-37 doi: 10.31083/j.jin.2020.01.1231 [11] KULESZA B, LITAK J, GROCHOWSKI C, et al. The initial factors with strong predictive value in relation to six-month outcome among patients operated due to extra-axial hematomas[J]. Diagnostics (Basel), 2020, 10(3): E174. doi: 10.3390/diagnostics10030174 [12] TUDOR R M, THOMPSON C J. Posterior pituitary dysfunction following traumatic brain injury: review[J]. Pituitary, 2019, 22(3): 296-304. doi: 10.1007/s11102-018-0917-z [13] JOHN A P. Early warning score challenges and opportunities in the care of deteriorating patients[J]. Dan Med J, 2018, 65(2): pii, B5439. http://ugeskriftet.dk/files/b5439_early_warning_score_challenges_and_opportunities_in_the_care_of_deteriorating_patients.pdf [14] FRANCO-JIMÉNEZ J A, CEJA-ESPINOSA A, ÁLVAREZ-VÁZQUEZ L, et al. Associated factors for Tracheostomy in adults with severe traumatic brain injury. Score proposal[J]. Cir Cir, 2020, 88(2): 200-205. http://med.wanfangdata.com.cn/Paper/Detail/PeriodicalPaper_PM32116326 [15] NIK A, SHEIKH ANDALIBI M S, EHSAEI M R, et al. The efficacy of glasgow coma scale (gcs) score and acute physiology and chronic health evaluation (APACHE) Ⅱ for predicting hospital mortality of icu patients with acute traumatic brain injury[J]. Bull Emerg Trauma, 2018, 6(2): 141-145. doi: 10.29252/beat-060208 [16] 李晓燕, 都玉娜, 陈民, 等. 改良早期预警评分临床应用的SWOT分析[J]. 中华危重病急救医学, 2019, 31(4): 509-512. doi: 10.3760/cma.j.issn.2095-4352.2019.04.029 [17] OKONKWO D O, SHUTTER L A, MOORE C, et al. Brain oxygen optimization in severe traumatic brain injury phase-Ⅱ: A phase Ⅱ randomized triala[J]. Crit Care Med, 2017, 45(11): 1907-1914. doi: 10.1097/CCM.0000000000002619 [18] RAGHUPATHI R, HUH J. Age-at-injury effects of microglial activation following traumatic brain injury: implications for treatment strategies[J]. Neural Regen Res, 2017, 12(5): 741-742. doi: 10.4103/1673-5374.206639 [19] EARLY A N, GORMAN A A, Van Eldik L J, et al. Effects of advanced age upon astrocyte-specific responses to acute traumatic brain injury in mice[J]. J Neuroinflammation, 2020, 17(1): 115. doi: 10.1186/s12974-020-01800-w [20] KONDO Y, GIBO K, ABE T, et al. Association of prehospital oxygen administration and mortality in severe trauma patients (PROMIS): A nationwide cohort study[J]. Medicine (Baltimore), 2019, 98(27): e16307. doi: 10.1097/MD.0000000000016307 -





 下载:
下载: