Analysis of preoperative risk factors of severe neonatal meconium aspiration syndrome
-
摘要:
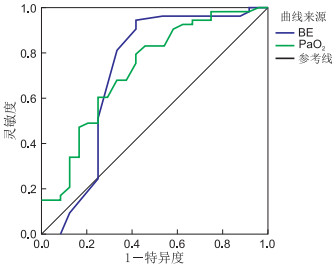
目的 探讨影响重症胎粪吸入综合征(meconium aspiration syndrome,MAS)患儿预后的危险因素,分析这些因素的预测价值,为提高MAS的临床救治水平提供帮助。 方法 回顾性分析蚌埠医学院第一附属医院2014年1月—2019年12月收治的77例行机械通气治疗的重症MAS患儿的临床资料,根据治疗结果分为通气成功组和通气失败组,对2组患儿一般资料、动脉血气分析及其并发症进行比较,再对有统计学意义的观察指标进行受试者特征(ROC)曲线及多因素逐步logistic回归分析。 结果 (1) 通气失败组胎儿宫内窘迫、持续性肺动脉高压(PPHN)及多器官功能障碍(MODS)发生率分别为66.7%、41.7%及66.7%,均高于通气成功组(41.5%、5.7%、22.6%),通气失败组的Apgar评分、pH值、动脉血氧分压(PaO2)及碱剩余(BE)均明显低于成功组,比较差异均有统计学意义(均P < 0.05)。(2)多因素logistic回归分析显示PaO2、BE值、PPHN、MODS是影响机械通气治疗MAS预后的独立危险因素。(3)ROC曲线分析显示BE值为-8.5是预测MAS预后的最佳界值点,敏感性和特异性分别为94.3%和58.3%;PaO2为40.5 mm Hg(1 mm Hg=0.133 kPa)是预测MAS预后的最佳界值点,敏感性和特异性分别为79.2%和58.3%。 结论 PaO2、BE值及并发症PPHN、MODS是影响机械通气治疗重症MAS患儿预后的独立危险因素,PaO2及BE值有助于早期预测重症MAS患儿的预后,早期及时对这些危险因素采取防治措施有助于降低重症MAS的病死率。 Abstract:Objective To explore the risk factors affecting the prognosis of children with severe meconium inhalation syndrome (MAS), analyse the predictive value of these factors, and improve the clinical treatment level of MAS. Methods The clinical data of 77 patients with severe MAS treated by mechanical ventilation from January 2014 to December 2019 were retrospectively analysed. According to the treatment results, the patients were divided into successful ventilation group and failure ventilation group. The general data, arterial blood gas analysis and their complications were compared between the two groups. Receiver characteristic (ROC) curve and stepwise logistic regression were used to analyse the statistically significant observation indexes. Results (1) The incidence of intrauterine distress, persistent pulmonary hypertension (PPHN) and multiple organ dysfunction (MODS) in the failure ventilation group was 66.7%, 41.7% and 66.7%, respectively, which were higher than those in the successful ventilation group (41.5%, 5.7% and 22.6%). The Apgar score, pH value, arterial partial pressure of oxygen (PaO2) and buffer excess (BE) in the failure ventilation group were significantly lower than those in the successful ventilation group. The difference was statistically significant (all P < 0.05). (2) Multivariate logistic regression analysis showed that PaO2, BE value, PPHN and MODS were independent risk factors of mechanical ventilation in the treatment of MAS. (3) ROC curve analysis showed that the BE value of -8.5 was the suitable boundary point to predict MAS prognosis, and the sensitivity and specificity were 94.3% and 58.3%, respectively; its PaO2 was 40.5 mm Hg, which was the best boundary point to predict prognosis, and the sensitivity and specificity were 79.2% and 58.3%, respectively. Conclusion PaO2 BE values and combined PPHN and MODS are the independent risk factors affecting the prognosis of MAS after mechanical ventilation. BE values and PaO2 can predict the prognosis of children with MAS, and early and timely prevention and treatment of these risk factors can reduce the mortality of severe MAS. -
Key words:
- Meconium aspiration syndrome /
- Risk factors /
- Prognosis /
- Neonatus
-
表 1 2组MAS患儿临床资料比较(x±s)
组别 例数 入院日龄[M(P25, P75), h] 胎龄(周) 出生体重(g) 性别[例(%)] 剖宫产[例(%)] 宫内窘迫[例(%)] 男 女 成功组 53 3(1.5,6.0) 39.5±1.4 3 202±609 32(60.4) 21(39.6) 28(52.8) 22(41.5) 失败组 24 4(2.0,10.5) 39.8±1.7 3 307±538 14(58.3) 10(41.7) 12(50.0) 16(66.7) 统计值 -0.924a -0.877b -0.722b 0.029c 0.053c 4.183c P值 0.355 0.383 0.437 0.865 0.818 0.041 组别 例数 pH值 PaCO2(mm Hg) PaO2(mm Hg) BE值 Apgar 1 min评分(分) Apgar 5 min评分(分) 成功组 53 7.2±0.1 51.8±13.3 53.6±19.0 -5.2±2.8 7±1 7±1 失败组 24 7.1±0.2 54.8±15.4 40.0±16.6 -9.7±7.2 5±2 8±1 统计值 2.337b -0.889b 3.012b -2.994b -3.789b -3.935b P值 0.026 0.377 0.004 0.003 < 0.001 < 0.001 注:a为Z值,b为t值,c为χ2值。 表 2 2组MAS患儿并发症比较[例(%)]
组别 例数 HIE NRDS PPHN MODS NPH 成功组 53 45(84.9) 38(71.7) 3(5.7) 12(22.6) 0(0) 失败组 24 23(95.8) 22(91.7) 10(41.7) 16(66.7) 2(8.3) χ2值 0.999 3.829 12.804 13.836 1.839 P值 0.318 0.050 < 0.001 < 0.001 0.175 表 3 多因素logistic回归赋值表
自变量 赋值 治疗结果 0=失败,1=成功 Apgar 1 min 定量 Apgar 5 min 定量 pH值 定量 BE值 定量 PaO2 定量 PPHN 0=有,1=无 MODS 0=有,1=无 表 4 影响MAS预后的多因素逐步logistic回归分析
项目 B SE Wald χ2 P值 OR值 95%CI Apgar 1 min 0.146 0.529 0.077 0.782 1.158 0.411~3.263 Apgar 5 min -1.304 0.742 3.087 0.079 0.271 0.063~1.163 PH值 -6.533 4.892 1.783 0.182 0.001 < 0.001~21.238 BE值 -0.289 0.144 4.045 0.044 0.749 0.565~0.993 PaO2 -0.133 0.058 5.256 0.022 0.875 0.781~0.981 PPHN 3.753 1.673 5.260 0.022 42.670 1.726~1 054.833 MODS 2.951 1.429 4.264 0.039 19.133 1.162~315.052 表 5 患儿BE值及PaO2对MAS预后的预测价值分析
项目 临界值 灵敏度(%) 特异度(%) AUC P值 95% CI BE -8.5 94.3 58.3 0.713 0.003 0.558~0.867 PaO2 40.5 79.2 58.3 0.726 0.002 0.559~0.853 -
[1] KUMAR A, KUMAR P, BASU S, Endotracheal suctioning for prevention of meconium aspiration syndrome: a randomized controlled trial[J]. Eur J Pediatr, 2019, 178(2): 1825-1832. doi: 10.1007/s00431-019-03463-z [2] PANDITA A, MURKI S, OLETI T P, et al. Effect of nasal continuous positive airway pressure on infants with meconium aspiration syndrome: a randomized clinical trial[J]. JAMA Pediatrics, 2018, 172(2): 161-165. doi: 10.1001/jamapediatrics.2017.3873 [3] CALKOVSKA A, MOKRA D, CALKOVSKY V, et al. Clinical considerations when treating neonatal aspiration syndromes[J]. Expert Rev Respir, 2019, 13(2): 193-203. doi: 10.1080/17476348.2019.1562340 [4] 邵肖梅, 叶鸿瑁, 丘小汕. 实用新生儿学[M]. 5版. 北京: 人民卫生出版社, 2019: 412-416, 699-714, 405-408, 568-573, 642-646. [5] 林碧云, 龙莎莎, 王来栓. 新生儿窒息后多器官损害诊断标准研究进展[J]. 中华围产医学杂志, 2016, 19(4): 243-246. doi: 10.3760/cma.j.issn.1007-9408.2016.04.002 [6] MOHAMMAD N, JAMAL T, SOHAILA, A, et al. Meconium stained liquor and its neonatal outcome[J]. Pak J Med Sci, 2018, 34(6): 1392-1396. [7] SHRESTH A, SINGH S D, TAMRAKAR D. Associated factors and outcome of babies born through meconium stained amniotic fluid[J]. Kat J Univ Med, 2018, 16(61): 65-68. http://www.ncbi.nlm.nih.gov/pubmed/30631020 [8] RUSSELL K W, NANCE M L, ADZICK N S, et al. Meconium aspirtion syndrome requiring ECMO in newborns with gastroschisis: incidence and surgical outcomes[J]. Pediatr Surg Int, 2019, 35(4): 469-472. doi: 10.1007/s00383-018-4419-x [9] OLIVEIRA C P L, ROCHA G M D, MACHADO A, et al. Meconium aspiration syndrome: risk factors and predictors severity[J]. J Mater Fetal Neonatal Med, 2019, 32(9): 1492-1498. doi: 10.1080/14767058.2017.1410700 [10] PAUDEL P, SUNNY A K, POUDEL P G, et al. Meconium aspiration syndrome: incidence, associated risk factors and outcome-evidence from a multicentric study in low-resource settings in Nepal[J]. J Paediatr Child Health, 2020, 56(4): 630-635. doi: 10.1111/jpc.14703 [11] 杨健红, 谭艳丽, 唐红, 等. 胎心监护联合脐血血气分析及Apgar评分预测羊水粪染新生儿窒息的临床价值[J]. 广西医学, 2016, 38(1): 35-38. https://www.cnki.com.cn/Article/CJFDTOTAL-GYYX201601013.htm [12] 付迎新, 彭薇, 张王梅. 脐动脉血气分析联合Apgar评分在新生儿窒息并发多器官损伤中的诊断价值[J]. 中国妇幼保健, 2018, 33(7): 1539-1542. https://www.cnki.com.cn/Article/CJFDTOTAL-ZFYB201807033.htm [13] PANTON L, TROTMAN H. Outcome of neonates with meconium aspiration syndrome at the University Hospital of the West Indies, Jamaica: a resource-limited setting[J]. Am J Perinatol, 2017, 34(12): 1250-1254. doi: 10.1055/s-0037-1603330 [14] 帕提曼·吐尔洪. 新生儿胎粪吸入综合征引起肺动脉高压的临床分析[J]. 中国实用医药, 2017, 12(22): 63-64. https://www.cnki.com.cn/Article/CJFDTOTAL-ZSSA201722034.htm [15] CHOUDHARY M, MEENA M K, CHHANGANI N. et al. To study prevalence of persistent pulmonary hypertension in newborn with meconium aspiration syndrome in western Rajasthan, India: a prospective observational study[J]. J Matern Fetal Neonatal Med, 2016;29(2): 324-327. doi: 10.3109/14767058.2014.1000296 [16] QASIM A, JAIN S K. Milrinone use in persistent pulmonary hypertension of the newborn[J]. Neoreviews, 2020, 21(3): 165-178. doi: 10.1542/neo.21-3-e165 [17] 王俊怡, 虞人杰, 刘淑芳, 等. 新生儿窒息多器官损害发生率、高危因素和转归的多中心研究[J]. 中华围产医学杂志, 2016, 19(1): 23-28. doi: 10.3760/cma.j.issn.1007-9408.2016.01.008 [18] WEISS S L, PETERS M J, ALHAZZANI W, et al. Surviving sepsis campaign international guidelines for the management of septic shock and sepsis-associated organ dysfunction in children[J]. Pediatr Crit Care Med, 2020, 21(2): 52-106. doi: 10.1097/PCC.0000000000002198 [19] 杨雨航, 裴亮, 杨妮, 等. 儿科重症监护病房中的新发功能障碍[J]. 中华儿科杂志, 2017, 55(6): 451-456. doi: 10.3760/cma.j.issn.0578-1310.2017.06.011 -





 下载:
下载: