Relationship between the quantitative parameters of diffusion kurtosis imaging and the Ki-67 expression level in rectal adenocarcinoma
-
摘要:
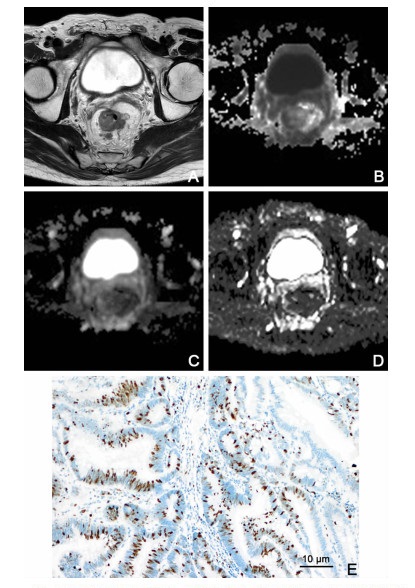
目的 探讨直肠腺癌扩散峰度成像(DKI)定量参数与Ki-67表达的相关性。 方法 选取广东省中医院2019年1月—2020年6月收治的术前未接受新辅助化疗行高分辨率MRI、扩散加权成像(DWI, b=0、1 000 s/mm2)及DKI(b=0、600、1 000、2 000 s/mm2)检查的43例直肠腺癌患者, 测量病灶相应的平均扩散峰度(MK)、平均扩散系数(MD)及表观扩散系数(ADC), 按Ki-67表达将其分为低表达组(Ki-67指数≤25%)和高表达组(Ki-67指数>25%), 比较2组间MK、MD及ADC有无差异, 用Spearman相关法评价各定量参数与Ki-67表达的相关性, 并通过受试者工作特征曲线(ROC)来确定各参数鉴别诊断直肠腺癌Ki-67低表达与高表达的效能。 结果 直肠腺癌Ki-67低表达组与高表达组的MK、ADC分别为[0.88(0.81, 0.94) vs. 1.22(1.06, 1.34);1.20(1.12, 1.30)×10-3 mm2/s vs. 1.10(0.94, 1.15)×10-3 mm2/s], 差异有统计学意义(均P<0.01), 2组间MD[1.20(1.12, 1.30)×10-3 mm2/s vs.1.20(1.10, 1.30)×10-3 mm2/s]比较差异无统计学意义(P>0.05)。MK与Ki-67表达呈正相关(r=0.523, P<0.001), ADC与Ki-67表达呈负相关(r=-0.467, P<0.01)。MK的曲线下面积(AUC=0.906)较ADC、MD的更大, 以MK=0.96为诊断阈值时, 敏感性为96.77%, 特异性为75.00%。 结论 MK、ADC与Ki-67表达相关, 均可间接评估直肠腺癌肿瘤细胞的增殖情况, 但MK在诊断效能方面优于ADC, 能更好地反映直肠腺癌的侵袭性和分子生物学特性。 Abstract:Objective To explore the relationship between quantitative parameters of diffusion kurtosis imaging (DKI) and the molecular markers Ki-67 in patients with rectal adenocarcinoma. Methods A total of 43 patients with rectal adenocarcinoma who underwent surgery and did not receive chemoradiotherapy were selected in this retrospective study. The image data included high-resolution MRI, conventional diffusion-weighted imaging and DKI, Mean kurtosis (MK), mean diffusivity (MD) and apparent diffusion coefficient (ADC) were calculated. The patients were divided into the low-Ki-67 group (Ki-67 ≤ 25%) and high-Ki-67 group (Ki-67>25%) on the basis of the Ki-67 level. The difference of each parameter between the two groups was compared. Spearman correlation analysis was applied to confirm the correlation between each parameter value and Ki-67 expression level. The receiver operating characteristic (ROC) curve was used to evaluate the diagnostic efficacy of each parameter. Results In the high-Ki-67 group, MK and MD were significantly different compared with those in the low-Ki-67 group [0.88(0.81, 0.94) vs. 1.22(1.06, 1.34), P < 0.01; 1.20(1.12, 1.30)×10-3 mm2/s vs. 1.10(0.94, 1.15)×10-3 mm2/s, P < 0.01]. However, MD showed no difference between the two groups [1.20(1.12, 1.30)×10-3 mm2/s vs. 1.20(1.10, 1.30)×10-3 mm2/s, P>0.05]. MK showed a positive association with the Ki-67 expression level (r=0.523, P < 0.001), whereas ADC showed a negative association with the Ki-67 expression level (r=-0.467, P < 0.01). Compared with MD and ADC, MK showed relatively higher area under the ROC curve of 0.906, sensitivity of 0.97 and specificity of 0.75. Conclusion MK and ADC are related to Ki-67 expression, which can indirectly evaluate the proliferation of rectal adenocarcinoma cells. However, MK is superior to ADC in diagnosis efficiency, and can better reflect the invasion and molecular biological characteristics of rectal adenocarcinoma. -
表 1 2组直肠癌患者MK、MD及ADC比较(x ±s)
组别 例数 MK MD (×10-3 mm2/s) ADC (×10-3 mm2/s) 低表达组 12 0.88(0.81, 0.94) 1.20(1.12, 1.30) 1.20(1.12, 1.30) 高表达组 31 1.22(1.06, 1.34) 1.20(1.10, 1.30) 1.10(0.94, 1.15) Z值 -4.090 -0.109 -3.035 P值 < 0.001 0.083 0.004 表 2 Ki-67表达与MK、MD及ADC的相关性
参数 MK MD ADC r值 0.523 0.053 -0.467 P值 < 0.001 0.735 0.002 表 3 MK、MD及ADC的受试者工作曲线
参数 曲线下面积 阈值 敏感性(%) 特异性(%) P值 MK 0.906 0.96 96.77 75.00 0.012 MD(×10-3 mm2/s) 0.511 1.11 83.87 33.33 0.924 ADC(×10-3 mm2/s) 0.800 1.04 61.29 91.67 0.010 -
[1] 赵岩, 孙健, 吴影, 等. 结直肠癌中Survivin、Caspase 9和Ki-67表达的相关性及临床意义[J]. 临床与实验病理学杂志, 2017, 33(4): 435-438. https://www.cnki.com.cn/Article/CJFDTOTAL-LSBL201704019.htm [2] GRANATA V, FUSCO R, REGINELLI A, et al. Diffusion kurtosis imaging in patients with locally advanced rectal cancer: current status and future perspectives[J]. J Int Med Res, 2019, 47(6): 2351-2360. doi: 10.1177/0300060519827168 [3] TONG G, ZHANG G, LIU J, et al. Cutoff of 25% for Ki67 expression is a good classification tool for prognosis in colorectal cancer in the AJCC-8 stratification[J]. Oncol Rep, 2020, 43(4): 1187-1198. http://www.ingentaconnect.com/content/sp/or/2020/00000043/00000004/art00014 [4] TONG G, XU W, ZHANG G, et al. The role of tissue and serum carcinoembryonic antigen in stages Ⅰ to Ⅲ of colorectal cancer-A retrospective cohort study[J]. Cancer Med, 2018, 7(11): 5327-5338. doi: 10.1002/cam4.1814 [5] BERLIN A, CASTRO-MESTA J F, RODRIGUEZ-ROMO L, et al. Prognostic role of Ki-67 score in localized prostate cancer: A systematic review and meta-analysis[J]. Urol Oncol, 2017, 35(8): 499-506. doi: 10.1016/j.urolonc.2017.05.004 [6] CLAY V, PAPAXOINIS G, SANDERSON B, et al. Evaluation of diagnostic and prognostic significance of Ki-67 index in pulmonary carcinoid tumours[J]. Clin Transl Oncol, 2017, 19(5): 579-586. doi: 10.1007/s12094-016-1568-z [7] ARIHIRO K, ODA M, OHARA M, et al. Comparison of visual assessment and image analysis in the evaluation of Ki-67 expression and their prognostic significance in immunohistochemically defined luminal breast carcinoma[J]. Jpn J Clin Oncol, 2016, 46(12): 1081-1087. doi: 10.1093/jjco/hyw107 [8] LUO Z W, ZHU M G, ZHANG Z Q, et al. Increased expression of Ki-67 is a poor prognostic marker for colorectal cancer patients: a meta analysis[J]. BMC Cancer, 2019, 19(1): 123. doi: 10.1186/s12885-019-5324-y [9] ZHU H, LI X, LIU Y, et al. Relationship between parameters of intravoxel incoherent motion imaging with Ki-67 expression level in rectal adenocarcinoma[J]. Chin J Med Imag Technol, 2017, 33(2): 237-241. http://www.researchgate.net/publication/318090590_Relationship_between_parameters_of_intravoxel_incoherent_motion_imaging_with_Ki-67_expression_level_in_rectal_adenocarcinoma [10] 钟华, 刘迪群. 结直肠癌组织中Ki-67和COX-2的表达及其临床意义[J]. 吉林大学学报(医学版), 2016, 42(6): 1168-1172. https://www.cnki.com.cn/Article/CJFDTOTAL-BQEB201606023.htm [11] 张蔚桐, 姚宏亮, 雷三林, 等. 细胞增殖核抗原Ki-67、血管内皮生长因子与缺氧诱导因子-1a在结直肠腺癌组织中表达的临床意义[J]. 中国临床药理学杂志, 2016, 32(19): 1759-1762. https://www.cnki.com.cn/Article/CJFDTOTAL-GLYZ201619008.htm [12] 周洋, 徐鹏举. 扩散峰度成像(DKI)在体部应用的研究进展[J]. 复旦学报(医学版), 2018, 45(6): 911-915, 920. doi: 10.3969/j.issn.1672-8467.2018.06.027 [13] 周舒畅, 王玉锦, 黄璐, 等. 扩散峰度成像与扩散加权成像在难鉴别孤立性肺结节良恶性判定价值的比较研究[J]. 中华放射学杂志, 2019, 53(3): 200-204. doi: 10.3760/cma.j.issn.1005-1201.2019.03.008 [14] 张忠伟, 李杨飞, 潘璟琍, 等. 扩散峰度成像参数在帕金森病诊断中的价值研究[J]. 中华全科医学, 2020, 18(2): 273-276. https://www.cnki.com.cn/Article/CJFDTOTAL-SYQY202002030.htm [15] XING F, TU N, KOH T S, et al. MR diffusion kurtosis imaging predicts malignant potential and the histological type of meningioma[J]. Eur J Radiol, 2017, 95: 286-292. doi: 10.1016/j.ejrad.2017.08.019 [16] SUN K, CHEN X, CHAI W, et al. Breast cancer: diffusion kurtosis MR imaging-diagnostic accuracy and correlation with clinical-pathologic factors[J]. Radiology, 2015, 277(1): 46-55. doi: 10.1148/radiol.15141625 [17] WEN Z Q, CHEN Y, YANG X Y, et al. Application of magnetic resonance diffusion kurtosis imaging for distinguishing histopathologic subtypes and grades of rectal carcinoma[J]. Cancer Imaging, 2019, 19(1): 8. doi: 10.1186/s40644-019-0192-x [18] CUI Y, YANG X, DU X, et al. Whole-tumour diffusion kurtosis MR imaging histogram analysis of rectal adenocarcinoma: Correlation with clinical pathologic prognostic factors[J]. Eur Radiol, 2018, 28(4): 1485-1494. doi: 10.1007/s00330-017-5094-3 [19] YAMADA I, HIKISHIMA K, YOSHINO N, et al. Colorectal carcinoma: Ex vivo evaluation using q-space imaging; Correlation with histopathologic findings[J]. J Magn Reson Imaging, 2018, 48(4): 1059-1068. doi: 10.1002/jmri.26018 [20] ZHU L, PAN Z, MA Q, et al. Diffusion kurtosis imaging study of rectal adenocarcinoma associated with histopathologic prognostic factors: preliminary findings[J]. Radiology, 2017, 284(1): 66-76. doi: 10.1148/radiol.2016160094 -





 下载:
下载: