Predictive effect of subjective experience of antipsychotic side effects on medication compliance in schizophrenia
-
摘要:
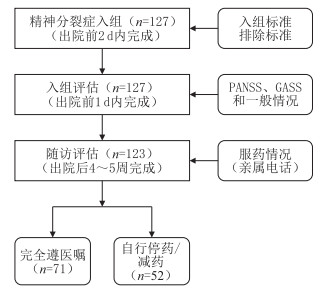
目的 检验抗精神病药物副反应主观体验对精神分裂症患者服药依从性的预测价值。 方法 选择2019年3—6月温州市第七人民医院收治的123例精神分裂症患者,在出院时完成格拉斯哥精神病药物副反应评定量表(Glasgow antipsychotics side-effect scale, GASS)评分。在患者出院后的4~5周,完成药物治疗依从性的电话随访。采用非条件多参数logistic回归分析,探查精神分裂症患者服药依从性的相关危险因素。并采用受试者工作曲线(ROC),以GASS总分为自变量,计算其区分“药物不依从”时的曲线下面积及预测灵敏度和特异度。 结果 52例精神分裂症患者在随访中报告有减少药物剂量或停止使用药物情况,“服药不依从”占42.3%。回归分析结果提示,GASS总分可显著预测“服药不依从”(OR=1.105, 95% CI=1.041~1.173),其中GASS锥体外系副反应因子分与“服药不依从”存在显著的正向关联(P < 0.01,OR=7.965, 95% CI=2.371~26.754)。受试者工作曲线分析结果提示,GASS总分≥20分预测“服药不依从”的灵敏度为92.3%,特异度为66.2%。 结论 患者的药物副反应主观体验可用于预测门诊精神分裂症患者服药依从性。 -
关键词:
- 精神分裂症 /
- 服药依从性 /
- 格拉斯哥精神病药物副反应评定量表
Abstract:Objective To examine the predictive value of subjective experience of antipsychotic side effects on medication compliance in patients with schizophrenia. Methods One hundred and twenty-three patients with schizophrenia completed the Glasgow Antipsychotics Side-effect Scale (GASS) at discharge, and medication compliance follow-up was completed 4-5 weeks after discharge. In the receiver operating curve, the total GASS score was used as the independent variable. The area under the curve was calculated, and the sensitivity and specificity were predicted. Results Fifty-two patients (42.3%) were defined as medication non-compliance. The total score of GASS (OR=1.105, 95% CI=1.041-1.173) and the score of extrapyramidal side effect of GASS (OR=7.965, 95% CI=2.371-26.754) were significantly associated with medication non-compliance (all P < 0.01). Receiver operating characteristic curve analysis indicated that the suitable cut-off points on total score of GASS for identifying medication non-compliance was ≥20 (sensitivity and specificity were 92.3% and 66.2%, respectively). Conclusion The subjective experience of antipsychotic side effects can be used to predict medication non-compliance in patients with schizophrenia. -
表 1 2组精神分裂症患者一般情况比较(x ±s)
项目 例数 性别(例) 年龄(岁) 受教育年数(年) 氯丙嗪当量(mg/d) PANSS(分) GASS总分(分) 药物副反应[例(%)] 女性 男性 阳性症状总分 阴性症状总分 一般症状总分 总分 无/轻度 中度 重度 服药不依从 52 20 32 32.04±7.15 12.63±2.37 617.21±144.92 10.38±2.61 12.29±4.96 22.12±3.54 44.79±7.75 29.88±9.74 11(21.2) 36(69.2) 5(9.6) 服药依从 71 21 50 28.94±6.68 12.73±2.47 437.25±112.90 10.10±2.73 11.39±4.34 22.04±3.80 43.54±7.75 15.82±9.40 53(74.6) 18(25.4) 0(0.0) 统计量 1.066a 2.465b -0.221b 7.740b 0.585b 1.062b 0.109b 0.886b 8.074b 6.007c P值 0.302 0.015 0.826 < 0.001 0.560 0.290 0.914 0.377 < 0.001 < 0.001 注:a为χ2值,b为t值,c为Z值。 表 2 服药不依从的logistic回归分析结果
变量 B SE Wald χ2 P值 OR值 95% CI 服药不依从 常数项 -5.746 1.120 26.317 0.003 < 0.001 氯丙嗪当量 0.006 0.002 7.763 < 0.001 1.006 1.002~1.010 GASS总分 0.100 0.030 10.904 < 0.001 1.105 1.041~1.173 -
[1] WOO J J, POUGET J G, ZAI C C, et al. The complement system in schizophrenia: where are we now and what's next?[J]. Mol Psychiatry, 2020, 25(1): 114-130. doi: 10.1038/s41380-019-0479-0 [2] 陆林. 沈渔邨精神病学[M]. 6版. 北京: 人民卫生出版社, 2018: 300-301. [3] LIEBERMAN J A. Disease modifying effects of antipsychotic drugs in schizophrenia: a clinical and neurobiological perspective[J]. World Psychiatry, 2018, 17(2): 163-165. doi: 10.1002/wps.20543 [4] 唐建良, 金卫东, 江长旺, 等. 齐拉西酮联合奥氮平治疗精神分裂症后单一巩固治疗的疗效研究[J]. 中华全科医学, 2016, 14(7): 1083-1085, 1242. https://www.cnki.com.cn/Article/CJFDTOTAL-SYQY201607008.htm [5] AICHHORN W, WHITWORTH A B, WEISS E M, et al. Second-generation antipsychotics: is there evidence for sex differences in pharmacokinetic and adverse effect profiles?[J]. Drug Saf, 2006, 29(7): 587-598. doi: 10.2165/00002018-200629070-00004 [6] DUFORT A, ZIPURSKY R B. Understanding and managing treatment adherence in Schizophrenia[J]. Clin Schizophr Relat Psychoses, 2019. DOI: 10.3371/CSRP.ADRZ.121218. [7] KADRA G, STEWART R, SHETTY H, et al. Antipsychotic polypharmacy prescribing and risk of hospital readmission[J]. Psychopharmacology(Berl), 2018, 235(1): 281-289. doi: 10.1007/s00213-017-4767-6 [8] HAQUE A A, KAMAL A K M, LAILA Z D, et al. Factors associated with relapse of schizophrenia[J]. Bangl J Psychiatry, 2018, 29(2): 59. doi: 10.3329/bjpsy.v29i2.37851 [9] 陈春棉, 姜德国, 陈策, 等. 格拉斯哥抗精神病药副反应评定量表中文版信效度分析[J]. 中华行为医学与脑科学杂志, 2020, 29(1): 79-80, 83. [10] KITAGAWA K, SO R, NOMURA N, et al. Reliability of the glasgow antipsychotic side-effects scale for Clozapine Japanese version (GASS-C-J)[J]. PLoS One, 2020, 15(6): e0234864. doi: 10.1371/journal.pone.0234864 [11] SULTAN A R, REEM E S H, MOHSEN N M, et al. Studying medication adherence in patients with schizophrenia[J]. Middle East Current Psychiatry, 2016, 23(1): 27-34. doi: 10.1097/01.XME.0000475315.51718.d6 [12] PHAN S V. Medication adherence in patients with schizophrenia[J]. Int J Psychiatry Med, 2016, 51(2): 211-219. doi: 10.1177/0091217416636601 [13] CAQUEO-URÍZAR A, URZŪA A, FOND G, et al. Medication nonadherence among South American patients with schizophrenia[J]. Patient Prefer Adherence, 2017, 11: 1737-1744. doi: 10.2147/PPA.S144961 [14] THAM X C, XIE H, CHNG C M, et al. Factors affecting medication adherence among adults with schizophrenia: a literature review[J]. Arch Psychiatr Nurs, 2016, 30(6): 797-809. doi: 10.1016/j.apnu.2016.07.007 [15] KIKKERT M J, DEKKER J. Medication adherence decisions in patients with schizophrenia[J]. Prim Care Companion CNS Disord, 2017, 19(6): 17n02182. http://europepmc.org/abstract/MED/29216418 -





 下载:
下载: