The clinical significance of heparin-binding protein combined with CRP in the early evaluation of severe acute pancreatitis
-
摘要:
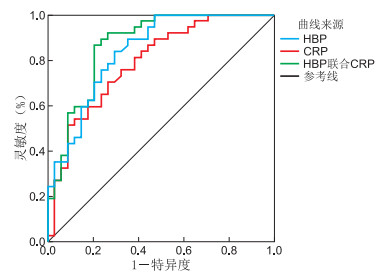
目的 探讨肝素结合蛋白(HBP)联合C反应蛋白(CRP)对重症急性胰腺炎(SAP)患者早期病情轻重程度评估的相关性及临床意义。 方法 收集2018年10月—2020年2月蚌埠医学院第一附属医院急诊外科收治的急性胰腺炎患者71例,根据病情严重程度按照重症急性胰腺炎诊断标准分为SAP患者37例,非SAP患者34例,记录2组患者的一般临床资料,检测入院时HBP、CRP水平,并对其进行APACHEⅡ评分,用Pearson相关分析及工作特征曲线(ROC)评估HBP、CRP以及二者联合在重症急性胰腺炎早期病情评估中的临床价值及意义。 结果 2组患者一般临床资料比较差异无统计学意义。HBP、CRP水平高低与APACHEⅡ评分有关(r=0.759、0.365,均P < 0.05);由ROC曲线可知,HBP、CRP、HBP+CRP的曲线下面积分别为:0.841、0.792、0.869。 结论 HBP、CRP与早期急性胰腺炎的病情程度有正相关性,且HBP的相关性较CRP高,HBP、CRP两者均可很好地预测SAP, 两者联合预测时灵敏度及特异性均高于单个指标预测,HBP联合CRP检测在重症急性胰腺炎早期病情评估中具有较高的临床指导意义。 -
关键词:
- 重症急性胰腺炎 /
- 肝素结合蛋白 /
- C-反应蛋白 /
- 急性生理与慢性健康评分
Abstract:Objective To investigate the correlation study and clinical significance of heparin-binding protein (HBP) combined with C-reactive protein (CRP) in evaluating the severity of the disease in patients with severe acute pancreatitis(SAP). Methods A total of 71 patients with acute pancreatitis admitted to the Emergency Department of the First Affiliated Hospital of Bengbu Medical College from October 2018 to February 2020 were collected. According to the severity of the disease, 37 patients with SAP and 34 patients with non-SAP patients were classified according to the diagnostic criteria of severe acute pancreatitis. The general clinical data of the two groups of patients were recorded, HBP and CRP levels at admission were detected, and APACHEⅡ scores were performed. Pearson correlation analysis and operating characteristic curve (ROC) were used to evaluate HBP, CRP and the combination of the two in evaluating the clinical value and significance of the disease in patients with severe acute pancreatitis. Results The general clinical data of the two groups of patients were not statistically significant. The levels of HBP and CRP were related to ApacheⅡ score (r=0.759, 0.365, all P < 0.05). According to ROC curve, the area under curve of HBP, CRP and HBP+CRP were 0.841, 0.792 and 0.869, respectively. Conclusion HBP and CRP are positively correlated with the severity of early acute pancreatitis, and the correlation between HBP is higher than that of CRP. Both HBP and CRP can predict SAP well, and the sensitivity and specificity of the combined prediction are high. Based on the prediction of a single index, this study shows that HBP combined with CRP detection has a high clinical guiding significance in the early evaluation of severe acute pancreatitis. -
Key words:
- Severe acute pancreatitis /
- Heparin-binding protein /
- C-reactive protein /
- APACHEⅡ score
-
表 1 2组胰腺炎患者APACHEⅡ评分、HBP和CRP水平比较
组别 例数 APACHEⅡ评分[M(P25, P75), 分] HBP [M(P25, P75),ng/mL] CRP (x±s,mg/L) SAP组 37 11(10,15) 88.60(71.56,127.08) 118.81±28.86 非SAP组 34 5(4, 6) 58.33(43.25,72.59) 90.07±28.89 统计量 52.847a 24.440a 4.189b P值 <0.001 <0.001 <0.001 注:a为H值,b为t值。 表 2 HBP值、CRP值及两者联合对SAP预测价值的比较分析
指标 截断值 灵敏度 特异度 AUC P值 95% CI HBP 68.95 0.838 0.706 0.841 <0.001 0.750~0.932 CRP 101.98 0.703 0.735 0.792 <0.001 0.688~0.897 HBP+CRP 60.333 0.865 0.794 0.869 <0.001 0.783~0.954 -
[1] PORTELLI M, JONES C D. Severe acute pancreatitis: pathogenesis, diagnosis and surgical management[J]. Hepatobiliary Pancreat Dis Int, 2017, 16(2): 155-159. doi: 10.1016/S1499-3872(16)60163-7 [2] MACHICADO J, GOUGOL A, PARAGOMI P, et al. 750 differences in the risk of persistent organ failure(POF) in acute pancreatitis(AP) based on onset, duration, and score of systemic inflammatory response syndrome(SIRS)[J]. Gastroenterology, 2020, 158(6): S152-S153. http://www.sciencedirect.com/science/article/pii/S0016508520310684 [3] VALVERDE-LÓPEZ F, MATAS-COBOS A M, ALEGRÍA-MOTTE C, et al. BISAP, RANSON, lactate and others biomarkers in prediction of severe acute pancreatitis in a European cohort[J]. J Gastronterol Hepatol, 2017, 32(9): 1649-1656. doi: 10.1111/jgh.13763 [4] 张映媛, 黄华, 路明亮, 等. 不同评分系统对判断急性胰腺炎病情及预后的比较研究[J]. 胃肠病学和肝病学杂志, 2018, 27(1): 25-29. doi: 10.3969/j.issn.1006-5709.2018.01.005 [5] 陈敏, 袁佳辉, 杨舟鑫, 等. 肝素结合蛋白对成人脓毒症诊断价值的Meta分析[J]. 中华危重病急救医学, 2019, 31(10): 1224-1225, 1230. doi: 10.3760/cma.j.issn.2095-4352.2019.10.009 [6] LIANG Y, ZHAO X, MENG F. Procalcitonin, C-reactive protein, and neutrophil ratio contribute to the diagnosis and prognosis of severe acute pancreatitis[J]. Iran J Public Health, 2019, 48(12): 2177-2186. http://www.ncbi.nlm.nih.gov/pubmed/31993385 [7] 杜奕奇, 陈其奎, 李宏宇, 等. 中国急性胰腺炎诊治指南(2019年, 沈阳)[J]. 临床肝胆病杂志, 2019, 35(12): 2706-2711. https://www.cnki.com.cn/Article/CJFDTOTAL-LCGD201912016.htm [8] HAJ-MIRZAIAN A, PATEL B N, FISHMAN E K, et al. Value of multidisciplinary collaboration in acute and chronic pancreatitis[J]. Abdom Radiol(NY), 2020, 45(5): 1458-1467. doi: 10.1007/s00261-019-02320-9 [9] 邱兆磊, 王振杰, 程峰, 等. 超早期肠内营养联合微生态制剂治疗重症急性胰腺炎患者的临床价值[J]. 中华急诊医学杂志, 2018, 27(9): 967-971. doi: 10.3760/cma.j.issn.1671-0282.2018.09.003 [10] 叶远玲, 王瑞明, 胡芳玉. 早期肠内营养联合急腹症Ⅲ号对重症胰腺炎患者临床症状及胃肠道功能指标的影响[J]. 中华全科医学, 2019, 17(6): 977-980. https://www.cnki.com.cn/Article/CJFDTOTAL-SYQY201906025.htm [11] 谢佩佩, 杨富国, 潘新亭, 等. 血浆置换联合连续性肾脏替代疗法在重症急性胰腺炎患者中的应用研究[J]. 中华危重症医学杂志(电子版), 2019, 12(5): 301-305. doi: 10.3877/cma.j.issn.1674-6880.2019.05.003 [12] 丘自挺, 唐玮欣, 段雯, 等. 脓毒症患者血浆PCT、NT-pro-BNP水平与APACHEⅡ评分的相关性[J]. 中国临床研究, 2017, 30(9): 1189-1191. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGCK201709010.htm [13] 周奋, 金雨虹, 王广芬, 等. 重症监护病房耐碳青霉烯类肠杆菌科细菌感染的危险因素分析[J]. 中华全科医学, 2019, 17(4): 580-582, 648. https://www.cnki.com.cn/Article/CJFDTOTAL-SYQY201904018.htm [14] 邱兆磊, 王振杰, 程峰, 等. microRNA-155对重症急性胰腺炎大鼠急性肺损伤作用的研究[J]. 右江民族医学院学报, 2020, 42(2): 151-154. doi: 10.3969/j.issn.1001-5817.2020.02.004 [15] MO X J, YE X Z, LI Y P. Effects of euphorbia kansui on the serum levels of IL-6, TNF-α, NF-κB, sTNFR and IL-8 in patients with severe acute pancreatitis[J]. J Biol Regul Homeost Agents, 2019, 33(2): 469-475. http://www.ncbi.nlm.nih.gov/pubmed/30945511 [16] HUANG L, ZHU H, GU J. Octreotide and Continuous hemofiltration versus continuous hemofiltration alone in severe acute pancreatitis complicated with acute respiratory distress syndrome[J]. J Coll Physicians Surg Pak, 2019, 29(8): 785-787. doi: 10.29271/jcpsp.2019.08.785 [17] 张悦. 联合检验血清淀粉酶、脂肪酶及C反应蛋白在急性胰腺炎诊断中的价值研究[J]. 中国医药指南, 2020, 18(7): 75. https://www.cnki.com.cn/Article/CJFDTOTAL-YYXK202007052.htm [18] KAHN F, TVERRING J, MELLHAMMAR L, et al. Heparin-binding protein as a prognostic biomarker of sepsis and disease severity at the emergency department[J]. Shock, 2019, 52(6): 135-145. doi: 10.1097/SHK.0000000000001332 [19] 中华医学会重症医学分会. 中国严重脓毒症/脓毒性休克治疗指南(2014)[J]. 全科医学临床与教育, 2015, 13(4): 365-367. https://www.cnki.com.cn/Article/CJFDTOTAL-QKYL201504002.htm [20] 郑博坤, 宋光太, 杨凯, 等. 创伤性应激反应与炎症指标相关性[J]. 浙江创伤外科, 2018, 23(6): 1217-1218. doi: 10.3969/j.issn.1009-7147.2018.06.071 [21] RODRÍGUEZ-ROJAS C, PÉREZ-CAÑADAS P, RAMOS-ARENAS V, et al. CRP levels as predictor of admission to ICU in patients with pancreatitis acute[J]. Clinica Chimica Acta, 2019, 493: S373-S374. http://www.researchgate.net/publication/333540934_CRP_levels_as_predictor_of_admission_to_ICU_in_patients_with_pancreatitis_acute [22] 曹红导. 血清降钙素原和C-反应蛋白在急性胰腺炎治疗中的检测价值分析[J]. 国际感染病学(电子版), 2020, 9(2): 72-73. https://www.cnki.com.cn/Article/CJFDTOTAL-GJGR202002053.htm [23] YIN X, JING X, QI Z, et al. Quantification analysis of lactate dehydrogenase and C-reactive protein in evaluation of the severity and prognosis of the acute pancreatitis[J]. Cell Mol Biol(Noisy-le-qrand), 2020, 66(1): 122-125. http://www.researchgate.net/publication/341116936_Quantification_analysis_of_lactate_dehydrogenase_and_C-reactive_protein_in_evaluation_of_the_severity_and_prognosis_of_the_acute_pancreatitis -





 下载:
下载: