Clinical characteristics of primary biliary cholangitis and RPR value in diagnosing cirrhosis
-
摘要:
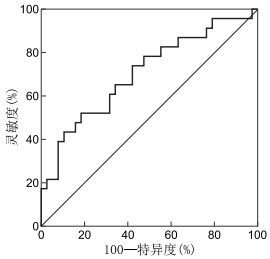
目的 探究原发性胆汁性胆管炎(primary biliary cholangitis,PBC)的临床特征及红细胞分布宽度与血小板计数比值(RDW-to-platelet ratio, RPR)对PBC肝硬化期的诊断价值,提高临床医生对该病的诊疗水平。 方法 收集2014年1月—2019年12月蚌埠医学院第一附属医院感染科门诊及住院部初次确诊为PBC的患者61例,对入组患者的临床资料进行回顾性分析。依据肝硬化诊断标准分为肝硬化组和非肝硬化组,比较2组的血常规、生化指标、RPR值、免疫球蛋白及补体水平。通过受试者工作特征曲线下面积(AUC)判断RPR对PBC肝硬化期的诊断价值。 结果 本组61例PBC患者中女性47例(77.05%);临床主要表现为黄疸(44.26%)和腹胀(24.59%);干燥综合征是最常合并的肝外自身免疫疾病;56例(91.80%)出现肝功能异常,以谷氨酰转肽酶(GGT)升高为主;抗线粒体抗体(anti-mitochondrial antibody, AMA)和(或)AMA-M2阳性率为93.44%;肝硬化组和非肝硬化组红细胞分布宽度(RDW)、血小板计数(PLT)、RPR及补体C3、C4比较差异均有统计学意义(均P < 0.05)。RPR诊断肝硬化的AUC值为0.705(95% CI:0.567~0.843;P=0.008), 最佳界值0.471, 灵敏度和特异度分别为52.20%和81.60%。 结论 PBC好发于中年女性,黄疸是最常见的临床表现。碱性磷酸酶(ALP)和GGT的升高以及AMA阳性是该病的主要特点。干燥综合征是最常合并的肝外自身免疫疾病。RPR对PBC肝硬化诊断有较高的特异度,可结合其他无创血清学指标协助评估疾病进程。 -
关键词:
- 原发性胆汁性胆管炎 /
- 肝硬化 /
- 红细胞分布宽度与血小板计数比值 /
- 抗线粒体抗体
Abstract:Objective To investigate the clinical features of primary biliary cholangitis (PBC) and the value of red blood cell distribution width-to-platelet ratio (RPR) in diagnosing PBC progression to cirrhosis, as well as to improve the level of diagnosis and treatment of the disease by clinicians. Methods From January 2014 to December 2019, 61 patients were diagnosed as PBC in the Outpatient and Inpatient Department of the First Affiliated Hospital of Bengbu Medical College. The clinical data of the patients were retrospectively analysed. According to the diagnostic criteria of cirrhosis, it was divided into cirrhosis and non-cirrhosis groups. Blood routine, biochemical indices, RPR values, immunoglobulin, and complement levels were compared between the two groups. The diagnostic value of RPR for PBC cirrhosis was judged by the area under the working characteristic curve (AUC). Results Amongst the 61 patients with PBC, 47 were female (77.05%). The main clinical manifestations were jaundice (44.26%) and abdominal distension (24.59%). Sjogren's syndrome was the most common extrahepatic autoimmune disease. A total of 56 cases (91.80%) had abnormal liver function, primarily GGT increase. The positive rate of anti-mitochondrial antibody (AMA) and/or AMA-M2 was 93.44%. Significant differences were observed in RDW, PLT, RPR, and complement C3 and C4 between cirrhotic and non-cirrhotic groups. The AUC value of RPR in diagnosing liver cirrhosis was 0.705 (95% CI: 0.567-0.843; P=0.008). The best value was 0.471, and the sensitivity and specificity were 52.20% and 81.60%, respectively. Conclusion PBC usually occurs in middle-aged women, and jaundice is the most common clinical manifestation. The increase in ALP and GGT and the positive AMA are the main characteristics of the disease. Sjogren's syndrome is the most commonly associated extrahepatic autoimmune disease. RPR has a high specificity in diagnosing PBC progression to cirrhosis and can be combined with other non-invasive serological indicators to help evaluate the disease progress. -
表 1 肝硬化组和非肝硬化组PBC患者临床资料比较[例(%)]
组别 例数 性别 年龄(x±s,岁) 黄疸 腹胀 乏力 脾大 腹水 女性 男性 非肝硬化组 38 29(76.32) 9(23.68) 53.76±11.43 18(47.37) 5(13.16) 8(21.05) 4(10.53) 2(5.26) 肝硬化组 23 18(78.26) 5(21.74) 58.43±12.18 9(39.13) 10(43.48) 4(17.39) 16(69.57) 12(52.17) 统计值 0.031a -1.510b 0.394a 7.103a <0.001a 22.662a 17.830a P值 0.861 0.137 0.530 0.008 0.987 <0.001 <0.001 组别 例数 上消化道出血 肝性脑病 AIH 干燥综合征 类风湿性关节炎 2型糖尿病 非肝硬化组 38 0(0.00) 1(2.63) 1(2.63) 7(18.42) 1(2.63) 3(7.89) 肝硬化组 23 2(8.70) 1(4.35) 2(8.70) 4(17.39) 0(0.00) 2(8.70) 统计值 0.203a <0.001a P值 0.138c 0.999c 0.652 0.999 0.999c 0.999 注:a为χ2值; b为t值; c为采用Fisher精确检验。 表 2 肝硬化组和非肝硬化组PBC患者生化指标比较[M(P25, P75)]
组别 例数 ALT(U/L) AST(U/L) ALP(U/L) GGT(U/L) TBil(μmol/L) 非肝硬化组 38 80.50(33.25,420.75) 109.00(52.50,295.25) 184.50(126.00,252.50) 201.50(83.00,384.75) 41.15(11.33,116.18) 肝硬化组 23 43.00(26.00,88.00) 74.00(32.00,184.00) 176.00(106.00,301.00) 128.00(41.00,286.00) 40.60(20.80,160.40) Z值 -1.845 -1.310 -0.327 -1.213 -0.699 P值 0.065 0.190 0.743 0.225 0.484 表 3 肝硬化组和非肝硬化组PBC患者免疫球蛋白及补体水平比较[M(P25, P75)]
组别 例数 IgG(g/L) IgA(g/L) IgM(g/L) C3(x±s,g/L) C4(x±s,g/L) 非肝硬化组 25 15.10(11.45,20.75) 2.90(1.76,4.82) 1.35(0.75,2.24) 0.87±0.35 0.18±0.07 肝硬化组 17 15.60(13.60, 17.80) 3.26(2.56, 4.63) 2.57(1.16,4.31) 0.60±0.23 0.12±0.06 统计值 -0.730a -0.974a -1.602a 2.703b 3.081b P值 0.465 0.330 0.109 0.010 0.004 注:a为Z值,b为t值。 表 4 肝硬化组和非肝硬化组PBC患者血常规指标及RPR值比较[M(P25, P75)]
组别 例数 RDW(%) PLT(x±s,109/L) RET% RPR 非肝硬化组 38 47.15(44.75,54.38) 173.05±75.80 1.12(0.88,1.51) 0.28(0.20,0.45) 肝硬化组 23 52.60(47.20,57.20) 126.57±87.33 1.22(0.91,1.87) 0.48(0.29,0.70) 统计值 -2.426a 2.192b -0.275a -2.664a P值 0.015 0.032 0.783 0.008 注:a为Z值,b为t值。 -
[1] WANG L, GERSHWIN E M, WANG F S. Primary biliary cholangitis in China[J]. Curr Opin Gastroenterol, 2016, 32(3): 195-203. http://www.ncbi.nlm.nih.gov/pubmed/26885951 [2] WANG H, XU H Q, WANG X M, et al. Red blood cell distribution width to platelet ratio is related to histologic severity of primary biliary cirrhosis[J]. Medicine(Baltimore), 2016, 95(11): e3114. http://www.scienceopen.com/document_file/5c0e919c-1c82-4eb7-bf2d-19764668cdd5/PubMedCentral/5c0e919c-1c82-4eb7-bf2d-19764668cdd5.pdf [3] HIRSCHFIELD G M, BEUERS U, CORPECHOT C, et al. EASL Clinical Practice Guidelines: The diagnosis and management of patients with primary biliary cholangitis[J]. J Hepatol, 2017, 67(1): 145-172. doi: 10.1016/j.jhep.2017.03.022 [4] 徐小元, 丁惠国, 李文刚, 等. 肝硬化诊治指南[J]. 临床肝胆病杂志, 2019, 35(11): 2408-2425. doi: 10.3969/j.issn.1001-5256.2019.11.006 [5] ABDULKARIM M, ZENOUZI R, SEBODE M, et al. Sex differences in clinical presentation and prognosis in patients with primary biliary cholangitis[J]. Scand J Gastroenterol, 2019, 54(11): 1391-1396. doi: 10.1080/00365521.2019.1683226 [6] GATSELIS N K, GOET J C, ZACHOU K, et al. Factors associated with progression and outcomes of early stage primary biliary cholangitis[J]. Clin Gastroenterol Hepatol, 2020, 18(3): 684-692, 696. doi: 10.1016/j.cgh.2019.08.013 [7] LOAEZA-DEL C A, GAYTAN-SANTILLAN A, LOPEZ-TELLO A, et al. Patterns of serum lipids derangements and cardiovascular risk assessment in patients with primary biliary cholangitis[J]. Ann Hepatol, 2019, 18(6): 879-882. doi: 10.1016/j.aohep.2019.07.006 [8] 鲁丹, 万彦彬, 杨小金, 等. 原发性胆汁性肝硬化合并自身免疫性疾病患者免疫学指标及补体水平研究[J]. 检验医学与临床, 2016, 13(13): 1829-1831. doi: 10.3969/j.issn.1672-9455.2016.13.032 [9] TANG L, ZHONG R, HE X, et al. Evidence for the association between IgG-antimitochondrial antibody and biochemical response to ursodeoxycholic acid treatment in primary biliary cholangitis[J]. J Gastroenterol Hepatol, 2017, 32(3): 659-666. doi: 10.1111/jgh.13534 [10] 李京华, 赵伟, 童晶晶, 等. 原发性胆汁性肝硬化发生失代偿的危险因素研究[J]. 检验医学, 2018, 33(5): 399-403. https://www.cnki.com.cn/Article/CJFDTOTAL-SHYY201805006.htm [11] 张帅, 郭冠亚, 周霞, 等. 原发性胆汁性胆管炎家系筛查及其低频突变的全外显子组测序研究[J]. 中华肝脏病杂志, 2018, 26(5): 388-392. doi: 10.3760/cma.j.issn.1007-3418.2018.05.014 [12] CELIK D, TATAR B, KOSE S, et al. Evaluation of the diagnostic validity of noninvasive tests for predicting liver fibrosis stage in chronic hepatitis B patients[J]. Acta Gastroenterol Belg, 2020, 83(3): 419-425. http://www.researchgate.net/publication/345145444_Evaluation_of_the_diagnostic_validity_of_noninvasive_tests_for_predicting_liver_fibrosis_stage_in_chronic_hepatitis_B_patients [13] WANG H L, WANG J, XIA J, et al. Red cell distribution width to platelet ratio predicts liver fibrosis in patients with autoimmune hepatitis[J]. Medicine(Baltimore), 2020, 99(34): e21408. http://journals.lww.com/md-journal/Fulltext/2020/08210/Red_cell_distribution_width_to_platelet_ratio.12.aspx [14] 申波, 蒋廷旺. RDW与RPR在原发性胆汁性胆管炎病理分期严重程度判定中的价值[J]. 国际检验医学杂志, 2020, 41(6): 751-754. doi: 10.3969/j.issn.1673-4130.2020.06.030 [15] HUANG C Y, HAN W J, WANG C M, et al. Early prognostic utility of gp210 antibody-positive rate in primary biliary cholangitis: A meta-analysis[J]. Dis Markers, 2019, 2019: 9121207. http://www.ncbi.nlm.nih.gov/pubmed/31737133 [16] YANG F, YANG Y, WANG Q, et al. The risk predictive values of UK-PBC and GLOBE scoring system in Chinese patients with primary biliary cholangitis: the additional effect of anti-gp210[J]. Aliment Pharmacol Ther, 2017, 45(5): 733-743. doi: 10.1111/apt.13927 [17] 卢慧, 张文. 抗着丝点抗体在多种疾病的临床意义[J]. 中华临床免疫和变态反应杂志, 2018, 12(6): 650-654. https://www.cnki.com.cn/Article/CJFDTOTAL-OZHL201806032.htm [18] CHEN C T, TSENG Y C, YANG C W, et al. Increased risks of spontaneous bacterial peritonitis and interstitial lung disease in primary biliary cirrhosis patients with concomitant sjogren syndrome[J]. Medicine(Baltimore), 2016, 95(2): e2537. http://www.onacademic.com/detail/journal_1000038709880210_2355.html [19] 涂荣芳, 杨雪, 唐映梅. 原发性胆汁性胆管炎合并肝外自身免疫性疾病的研究进展[J]. 临床肝胆病杂志, 2020, 36(6): 1398-1401. doi: 10.3969/j.issn.1001-5256.2020.06.046 [20] FAN X, MEN R, NI P, et al. Concomitant systemic lupus erythematosus might have a negative impact on the biochemical responses to treatment in patients with primary biliary cholangitis[J]. Clin Rheumatol, 2020, 39(3): 795-803. doi: 10.1007/s10067-019-04853-2 [21] HARMS M H, VAN BUUREN H R, CORPECHOT C, et al. Ursodeoxycholic acid therapy and liver transplant-free survival in patients with primary biliary cholangitis[J]. J Hepatol, 2019, 71(2): 357-365. doi: 10.1016/j.jhep.2019.04.001 -





 下载:
下载: