Immunophenotype and clinical characteristics of acute myeloid leukaemia with positive FLT3-ITD
-
摘要:
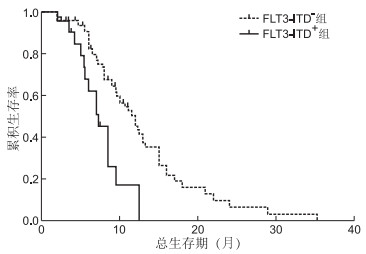
目的 探索伴有FMS样酪氨酸激酶3-内部串联重复(fms-like tyrosine kinase 3, FLT3-ITD)突变的急性髓系白血病(AML)患者的免疫表型及临床特征。 方法 收集2016年12月—2018年12月蚌埠医学院第一附属医院103例初诊AML患者(除外M3型),其中FLT3-ITD+患者24例(阳性组),FLT3-ITD-患者79例(阴性组)。对2组患者的临床特征和免疫表型进行回顾性研究,统计2组患者治疗总反应率(overall reaction,OR)、无进展生存时间(progression free survival,PFS)与总生存时间(overall survival, OS)。 结果 阳性组患者CD33、CD7、CD56及CD38抗原表达率较阴性组明显升高(均P < 0.05),而CD13、CD34表达率则显著降低(均P < 0.05);阳性组患者外周血白细胞计数、血红蛋白计数、骨髓原始细胞比例、合并NPM1(Nucleophosmin)突变率明显高于阴性组(均P < 0.05);阴性组患者治疗总反应率为78.48%,明显优于阳性组的33.33%,差异有统计学意义(P < 0.001)。阳性组患者中位OS为9.5个月,中位PFS为9个月;阴性组患者中位OS为17个月,中位PFS为16个月,阴性组较阳性组明显延长(P < 0.05)。 结论 FLT3-ITD阳性AML患者白血病细胞抗原表达紊乱,外周血白细胞、血红蛋白、骨髓原始细胞高,易合并NPM1突变且治疗总反应率低,PFS和OS明显缩短,治疗效果差,预后不良。 -
关键词:
- 急性髓系白血病 /
- FLT3-ITD突变 /
- 免疫表型 /
- 临床特征
Abstract:Objective To explore the immunophenotype and clinical characteristics of patients with acute myeloid leukaemia (AML) with fms-like tyrosine kinase 3-internal tandem replication (FLT3-ITD) mutation. Methods A total of 103 patients with AML (excluding the M3 type), including 24 patients with FLT3-ITD+ (positive group) and 79 patients with FLT3-ITD- (negative group), who were initially diagnosed in the haematology department of the First Affiliated Hospital of Bengbu Medical College from December 2016 to December 2018 were enrolled in this study. The clinical haematological characteristics and immunophenotypes of the two groups were retrospectively studied. The patients in both groups were followed up, and the overall reaction rate (OR), progress-free survival (PFS) and overall survival (OS) were calculated. Results The expression rates of CD33, CD7, CD56 and CD38 in the FLT3-ITD+group were significantly higher than those in the FLT3-ITD- group (all P < 0.05). By contrast, the expression rates of CD13 and CD34 were low (all P < 0.05). White blood cell count, haemoglobin count, bone marrow leukaemia cells and mutation rate of combined NPM1 in the FLT3-ITD+ group were higher than those in the FLT3-ITD- group (all P < 0.05). after the treatment the Objective response rate in the FLT3-ITD- group (78.5%) was significantly higher than that in the FLT3-ITD+ group (33.3%), and the difference was statistically significant (P < 0.001). The median OS and PFS in the FLT3-ITD+ group were 9.5 and 9 months, respectively, and those in the FLT3-ITD- group were 17 and 16 months, respectively. The OS and PFS of the FLT3-ITD- group were longer than those of the FLT3-ITD+ group (P < 0.05). Conclusion Patients with AML with FLT3-ITD+ have abnormal expression of leukaemia cell antigen, high peripheral blood leukocytes, abundant haemoglobin and bone marrow primordial cells, are prone to NPM1 mutation, have shortened PFS, OS and reduced the response rate. Hence, the treatment effect and prognosis of these patients are poor. -
Key words:
- Acute myeloid leukaemia /
- FLT3-ITD mutation /
- Immunophenotype /
- Clinical characteristics
-
表 1 2组初诊AML患者临床资料对比(x ±s)
组别 例数 年龄(岁) 性别(女/男,例) 白细胞计数(×109个/L) 血小板计数(×109个/L) 血红蛋白(×109个/L) 骨髓原始细胞比例/(%) 分型[例(%)] 合并NPM1突变率[例(%)] M0 M1 M2 M4 M5 M6 M7 FLT3-ITD阳性组 24 52.58±18.63 8/16 73.78±68.54 52.67±42.26 88.50±23.10 75.57±19.72 0(0.0) 4(16.7) 10(41.7) 3(12.5) 6(25.0) 1(4.2) 0(0.0) 15(62.50) FLT3-ITD阴性组 79 52.39±17.58 34/45 30.31±83.89 48.00±48.73 77.59±23.37 63.02±26.37 1(1.3) 7(8.7) 38(48.1) 21(26.6) 10(12.7) 1(1.3) 1(1.3) 16(20.25) 统计量 0.046a 0.797b 2.310a 0.423a 2.008a 2.709a 5.991b 15.294b P值 0.963 0.372 0.023 0.673 0.047 0.009 0.424 < 0.001 注:a为t值,b为χ2值。 表 2 2组AML患者LC抗原表达率比较[例(%)]
组别 例数 CD56 CD13 CD34 CD38 CD7 CD33 FLT3-ITD+组 24 8(33.33) 14(58.33) 12(50.00) 21(87.50) 8(33.33) 22(91.67) FLT3-ITD-组 79 10(12.66) 63(79.75) 60(75.95) 51(64.56) 11(13.92) 57(72.15) χ2值 5.456 4.473 5.892 4.606 4.606 3.923 P值 0.020 0.034 0.015 0.032 0.032 0.048 表 3 2组AML患者首次诱导化疗反应[例(%)]
组别 例数 CR PR NR 阳性组 24 5(20.83) 3(12.50) 16(66.67) 阴性组 79 35(44.30) 27(34.18) 17(21.52) Z值 -3.427 P值 0.001 -
[1] YOUNG A L, TONG R S, BIRMANN B M, et al. Clonal haematopoiesis and risk of acute myeloid leukemia[J]. Haematologica, 2019, 104(12): 175-185. http://www.sciencedirect.com/science/article/pii/S152169261930043X [2] 周文华, 陈国安. t(8;21)急性髓系白血病预后因素研究进展[J]. 中华实用诊断与治疗杂志, 2019, 33(2): 197-200. https://www.cnki.com.cn/Article/CJFDTOTAL-HNZD201902028.htm [3] HE Y, SUN L, XU Y, et al. Combined inhibition of PI3Kδand FLT3 signaling exerts synergistic antitumor activity and overcomes acquired drug resistance in FLT3-activated acute myeloid leukemia[J]. Cancer Lett, 2018, 420(4): 49-59. http://europepmc.org/abstract/MED/29409989 [4] 沈悌, 赵永强. 血液病诊断及疗效标准[M]. 4版. 北京: 科学出版社, 2018: 91-93. [5] INFANTE M S, PIRIS M Á, HERNÁNDEZ-RIVAS J Á. Molecular alterations in acute myeloid leukemia and their clinical and therapeutical implications[J]. Med Clin, 2018, 151(9): 362-367. doi: 10.1016/j.medcli.2018.05.002 [6] PAPAEMMANUIL E, GERSTUNG M, BULLINGER L, et al. Genomic classification and prognosis in acute myeloid leukemia[J]. N Engl J Med, 2016, 374(23): 2209-2221. doi: 10.1056/NEJMoa1516192 [7] SAKAGUCHI M, YAMAGUCHI H, KUBOYAMA M, et al. Significance of FLT3-tyrosine kinase domain mutation as a prognostic factor for acute myeloid leukemia[J]. Int J Hematol, 2019, 110(5): 566-574. doi: 10.1007/s12185-019-02720-z [8] CHOI E J, LEE J H, PARK H S, et al. Comparison of anthracyclines used for induction chemotherapy in patients with FLT3-ITD-mutated acute myeloid leukemia[J]. Leuk Res, 2018, 68(3): 51-56. http://europepmc.org/abstract/MED/29544132 [9] PASIC I, DANA W, LAM W, et al. Influence of FLT3-ITD and NPM1 status on allogeneic hematopoietic cell transplant outcomes in patients with cytogenetically normal AML[J]. Eur J Haematol, 2019, 102(4): 368-374. doi: 10.1111/ejh.13216 [10] DOHNER H, ESTEY E, GRIMWADE D, et al. Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel[J]. Blood, 2017, 129(4): 424-447. doi: 10.1182/blood-2016-08-733196 [11] KUROSAWA S, YAMAGUCHI H, YAMAGUCHI T, et al. The prognostic impact of FLT3-ITD, NPM1 and CEBPA in cytogenetically intermediate-risk AML after first relapse[J]. Int J Hematol, 2020, 102(4): 368-374. doi: 10.1007/s12185-020-02894-x?utm_medium=other&utm_content=null&utm_campaign=BSCN_1_DD01_CN_springer_article_paid_XMOL [12] 罗丽卿, 彭振翼, 刘晓, 等. IDH2基因突变对急性髓系白血病患者的临床特征及预后影响[J]. 中国实验血液学杂志, 2019, 27(4): 1077-1082. https://www.cnki.com.cn/Article/CJFDTOTAL-XYSY201904018.htm [13] ZHI H C, KAI H C, LEI T, et al. clinical and biological implications of mutational spectrum in acute myeloid leukemia of FAB subtypes M4 and M5[J]. Cancer Gene Ther, 2018, 25(4): 77-83. http://www.nature.com/articles/s41417-018-0013-6 [14] 郑源海, 林元峰, 许瑞元, 等. 急性髓系白血病免疫表型特征与预后相关性分析[J]. 现代检验医学杂志, 2018, 33(4): 90-94. doi: 10.3969/j.issn.1671-7414.2018.04.024 [15] BRAS A E, DE H V, VAN S A, et al. CD123 expression levels in 846 acute leukemia patients based on standardized immunophenotyping[J]. Cytometry B Clin Cytom, 2019, 96(2): 134-142. doi: 10.1002/cyto.b.21745 [16] 林婧祎, 张宇晶, 高锦程, 洪珞珈. 急性髓系白血病免疫治疗方式及研究进展[J]. 中华全科医学, 2017, 15(10): 1763-1767. https://www.cnki.com.cn/Article/CJFDTOTAL-SYQY201710039.htm [17] SCHRANZ K, HUBMANN M, HARIN E, et al. Clonal heterogeneity of FLT3-ITD detected by high-throughput amplicon sequencing correlates with adverse prognosis in acute myeloid leukemia[J]. Oncotarget, 2018, 9(53): 30128-30145. doi: 10.18632/oncotarget.25729 [18] ZHANG Q R, WU X, CAO J, et al. Association between increased mutation rates in DNMT3A and FLT3-ITD and poor prognosis of patients with acute myeloid leukemia[J]. Exp Ther Med, 2019, 18(4): 3117-3124. http://www.ncbi.nlm.nih.gov/pubmed/31572552 [19] 刘铁强, 黄珊, 姚波, 等. 伴CD4、CD7表达的AML患者免疫表型特点及其分子生物学和细胞遗传学特征[J]. 中国实验血液学杂志, 2016, 24(6): 1627-1632. https://www.cnki.com.cn/Article/CJFDTOTAL-XYSY201606006.htm [20] TAO S D, WANG C L, CHEN Y, et al. Prognosis and outcome of patients with acute myeloid leukemia based on FLT3-ITD mutation with or without additional abnormal cytogenetics[J]. Oncol Lett, 2019, 18(6): 6766-6774. http://www.ncbi.nlm.nih.gov/pubmed/31807186 -





 下载:
下载: