Prognostic value of pretreatment neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio in patients with locally advanced hypopharyngeal cancer treated with radiation
-
摘要:
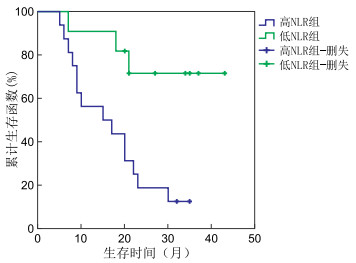
目的 分析放疗前外周血中性粒细胞与淋巴细胞比值(NLR)和血小板与淋巴细胞计数比(PLR)对局部晚期下咽鳞状细胞癌患者的预后评估价值。 方法 回顾性分析2017年2月—2018年12月蚌埠医学院第一附属医院放疗科收治的27例接受单纯放疗、序贯放化疗或同步放化疗下咽癌患者的临床以及随访资料。通过建立受试者工作特征曲线,获得最佳界值,根据界值将患者分为高NLR组、低NLR组以及高PLR组、低PLR组,分析患者放疗前外周血NLR和PLR与临床病理特征及预后的相关性,通过Kaplan-Meier法绘制患者的生存曲线,log rank法比较患者的预后,通过Cox比例风险回归模型进行多因素分析。 结果 27例患者中,有10例患者生存,中位随访时间为34个月,中位生存时间为21个月。放疗前NLR的最佳界值为2.30,PLR的最佳界值为131.46。放疗前高NLR组和低NLR组患者的2年总生存率分别为18.8%和45.5%(P=0.006)。放疗前高PLR组和低PLR组患者的2年总生存率分别为18.8%和45.5%(P=0.040)。Log rank单因素分析显示肿瘤临床分期、治疗方式、放疗前NLR和放疗前PLR与患者的总生存有关(均P < 0.05)。多因素分析结果显示,肿瘤临床分期和治疗方式为影响患者总生存的独立因素。 结论 放疗前NLR、PLR升高对于接受放疗的下咽癌患者可能是预后不良的影响因素,但仍需进一步深入研究。 -
关键词:
- 下咽肿瘤 /
- 预后 /
- 中性粒细胞与淋巴细胞比例 /
- 血小板与淋巴细胞比例
Abstract:Objective To evaluate retrospectively the prognostic value of pretreatment neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR) in patients with locally advanced hypopharyngeal cancer treated with radiotherapy. Methods Twenty-seven patients who received radiotherapy alone, sequential chemoradiotherapy or concurrent chemoradiotherapy for locally advanced hypopharyngeal cancer in our hospital from February 2017 to December 2018 were retrospectively analysed. The patients were divided into two groups: high (NLR group/low NLR group and high PLR group/low PLR groups. Appropriate cut-off points were determined via the receiver operating characteristic curve(ROC) method. The survival curve was established via the Kaplan-Meier method. The survival of the two groups was compared via log-rank test. Multivariate Cox regression analysis was conducted by. Results Among the 27 patients, 10 patients were still alive. The median follow-up time was 34 months, and the median survival time was 21 months. The best cut-off value of NLR and PLR before radiotherapy was 2.30 and 131.46, respectively. The 2-year overall survival rates of patients in the high NLR and the low NLR groups before radiotherapy were 18.8% and 45.5%, respectively (P=0.006). The 2-year overall survival rates of patients in the high PLR and the low PLR groups before radiotherapy were 18.8% and 45.5%, respectively (P=0.040). Log rank single-factor analysis revealed that tumour clinical stage, treatment and NLR/PLR ratio before radiotherapy were related to the overall survival of patients (all P < 0.05). Multivariate analysis showed that tumour clinical stage and treatment were independent factors affecting the overall survival of patients. Conclusion An increase in NLR/PLR ratio before radiotherapy may affect the prognosis of patients with hypopharyngeal cancer. However, the sample size of this study was small. Thus, further research is needed. -
表 1 各组下咽癌患者临床资料比较(例)
项目 类别 高NLR组(16例) 低NLR组(11例) P值 高PLR组(16例) 低PLR组(11例) P值 性别 男性 15 10 0.999 14 11 0.499 女性 1 1 2 0 年龄(岁) ≤65 8 8 0.427 10 6 0.710 >65 8 3 6 5 吸烟 是 9 5 0.704 10 4 0.252 否 7 6 6 7 饮酒 是 9 5 0.704 10 4 0.252 否 7 6 6 7 临床分期 Ⅲ期 3 5 0.144 3 5 0.240 ⅣA期 7 5 9 3 ⅣB期 6 1 4 3 治疗方案 单纯放疗 5 1 0.362 5 1 0.073 同步放化疗 10 9 11 8 序贯放化疗 1 1 0 2 表 2 影响下咽癌患者预后的单因素分析(例)
项目 类别 例数 生存情况 χ2值 P值 存活 死亡 性别 男性 25 9 16 0.384 0.535 女性 2 1 1 年龄(岁) ≤65 16 6 10 0.597 0.440 >65 11 4 7 吸烟 是 14 4 10 1.638 0.201 否 13 6 7 饮酒 是 14 4 10 2.550 0.110 否 13 6 7 临床分期 Ⅲ期 8 1 6 9.434 0.009 ⅣA期 12 4 4 ⅣB期 7 5 7 治疗方案 单纯放疗 6 0 6 9.274 0.010 同步放化疗 19 9 10 序贯放化疗 2 1 1 放疗前NLR 高NLR 16 2 14 7.623 0.006 低NLR 11 8 3 放疗前PLR 高PLR 16 3 13 4.218 0.040 低PLR 11 7 4 表 3 影响下咽癌患者预后的多因素分析
项目 B SE Wald χ2 P值 RR值 95% CI 临床分期 1.182 0.412 8.245 0.004 3.262 1.455~7.311 治疗方案 -1.765 0.542 10.611 0.001 0.171 0.059~0.495 放疗前NLR -0.707 0.742 0.909 0.340 0.493 0.115~2.110 放疗前PLR -0.645 0.629 1.051 0.305 0.525 0.153~1.800 -
[1] 钱洁, 朱江. 下咽癌的临床治疗策略[J]. 临床耳鼻咽喉头颈外科杂志, 2017, 31(21): 1701-1704. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH201721021.htm [2] ECKEL H E, BRADLEY P J. Treatment options for hypopharyngeal cancer[J]. Adv Otorhinolaryngol, 2019, 83: 47-53. http://www.ncbi.nlm.nih.gov/pubmed/30943512 [3] NEWMAN J R, CONNOLLY T M, ILLING E A, et al. Survival trends in hypopharyngeal cancer: a population-based review[J]. Laryngoscope, 2015, 125(3): 624-629. doi: 10.1002/lary.24915 [4] GRIGORIADIS T, VALLA A, ZACHARAKIS D, et al. Vaginal hysterectomy for uterovaginal prolapse: What is the incidence of concurrent gynecological malignancy?[J]. Int Urogynecol J, 2015, 26(3): 421-425. doi: 10.1007/s00192-014-2516-5 [5] GRIVENNIKOV S I, GRETEN F R, KARIN M. Immunity, inflammation, and cancer[J]. Cell, 2010, 140(6): 883-899. doi: 10.1016/j.cell.2010.01.025 [6] PICHLER M, HUTTERER G C, STOECKIGT C, et al. Validation of the pre-treatment neutrophil-lymphocyte ratio as a prognostic factor in a large European cohort of renal cell carcinoma patients[J]. Br J Cancer, 2013, 108(4): 901-907. doi: 10.1038/bjc.2013.28 [7] GUNDOG M, BASARAN H. The prognostic value of neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio in nasopharyngeal cancer[J]. J Buon, 2020, 25(1): 367-375. http://www.researchgate.net/publication/340593736_The_prognostic_value_of_neutrophil-to-lymphocyte_ratio_and_platelet-to-lymphocyte_ratio_in_nasopharyngeal_cancer [8] 董昕, 周宗玫, 毕楠, 等. 局部晚期非小细胞肺癌患者放疗前中性粒细胞与淋巴细胞比值对预后的意义[J]. 中华肿瘤杂志, 2018, 40(6): 446-451. doi: 10.3760/cma.j.issn.0253-3766.2018.06.009 [9] MANDALIYA H, JONES M, OLDMEADOW C, et al. Prognostic biomarkers in stage Ⅳ non-small cell lung cancer (NSCLC): neutrophil to lymphocyte ratio (NLR), lymphocyte to monocyte ratio (LMR), platelet to lymphocyte ratio (PLR) and advanced lung cancer inflammation index (ALI)[J]. Transl Lung Cancer Res, 2019, 8(6): 886-894. doi: 10.21037/tlcr.2019.11.16 [10] LUO H S, XU H Y, DU Z S, et al. Prognostic significance of baseline neutrophil count and lactate dehydrogenase level in patients with esophageal squamous cell cancer treated with radiotherapy[J]. Front Oncol, 2020, 10: 430. doi: 10.3389/fonc.2020.00430 [11] 何梅峰, 姜战武, 郝志伟, 等. 光学成像结合吲哚菁绿引导胃癌前哨淋巴结活检诊断价值的Meta分析[J]. 中华胃肠外科杂志, 2019, 22(12): 1196-1197, 1204. doi: 10.3760/cma.j.issn.1671-0274.2019.12.017 [12] 刘英俊, 高重庆, 王刚成, 等. 中性粒细胞与淋巴细胞比值早期预测直肠癌术后吻合口瘘的价值[J]. 中华肿瘤杂志, 2020, 42(1): 70-71, 73. doi: 10.3760/cma.j.issn.0253-3766.2020.01.011 [13] ARDI V C, KUPRIYANOVA T A, DERYUGINA E I, et al. Human neutrophils uniquely release TIMP-free MMP-9 to provide a potent catalytic stimulator of angiogenesis[J]. Proc Natl Acad Sci USA, 2007, 104(51): 20262-20267. doi: 10.1073/pnas.0706438104 [14] DING P R, AN X, ZHANG R X, et al. Elevated preoperative neutrophil to lymphocyte ratio predicts risk of recurrence following curative resection for stage IIA colon cancer[J]. Int J Colorectal Dis, 2010, 25(12): 1427-1433. doi: 10.1007/s00384-010-1052-0 [15] WILLIAMS K A, LABIDI-GALY S I, TERRY K L, et al. Prognostic significance and predictors of the neutrophil-to-lymphocyte ratio in ovarian cancer[J]. Gynecol Oncol, 2014, 132(3): 542-550. doi: 10.1016/j.ygyno.2014.01.026 [16] 李晓惠, 徐冰清, 高劲, 等. 中性粒细胞与淋巴细胞比值对鼻咽癌放射敏感性及预后影响的研究[J]. 中华放射肿瘤学杂志, 2016, 25(5): 432-436. doi: 10.3760/cma.j.issn.1004-4221.2016.05.002 [17] MOON H, ROH J L, LEE S W, et al. Prognostic value of nutritional and hematologic markers in head and neck squamous cell carcinoma treated by chemoradiotherapy[J]. Radiother Oncol, 2016, 118(2): 330-334. doi: 10.1016/j.radonc.2015.10.029 -





 下载:
下载: