Correlation between liver-controlled attenuation parameters and serum 25-hydroxyvitamin D level in patients with type 2 diabetes
-
摘要:
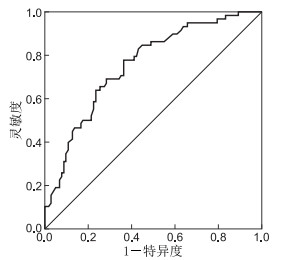
目的 探讨2型糖尿病(type 2 diabetes mellitus, T2DM)患者肝脏受控衰减参数(controlled attenuation parameters, CAP)值与血清25-羟维生素D[25(OH)D]的相关性。 方法 选取2019年5月—2020年7月在蚌埠医学院第一附属医院就诊的T2DM患者160例,依据CAP数值大小分为无NAFLD组(43例)、轻度NAFLD组(35例)、中度NAFLD组(35例)和重度NAFLD组(47例)。分别测定VAT、SAT、25(OH)D和其他生化指标,比较各组间生化指标的差异,采用logistic回归分析,Pearson或Spearman进行相关性分析,ROC曲线分析CAP预测T2DM患者维生素D缺乏的最佳阈值。 结果 无NAFLD组25(OH)D显著高于中度和重度NAFLD组,轻度和中度NAFLD组25(OH)D显著高于重度NAFLD组(均P < 0.05);CAP与25(OH)D、HDL-C呈负相关(r=-0.436、-0.193,均P < 0.05),CAP与WHR、BMI、VAT、SAT、TC、TG、FINS、HOMA-IR、FFA、CRP、γ-GT、ALT呈正相关(r=0.276~0.447,均P < 0.05);25(OH)D与CAP、VAT、FBG、TC、TG、FFA、HOMA-IR、ALT、CRP、γ-GT呈负相关(r=-0.436~-0.156,均P < 0.05)。Logistic回归分析发现FFA和25(OH)D是T2DM发生NAFLD的影响因素,ROC曲线显示以CAP在265 dB/m为诊断界值预测维生素D缺乏的敏感性为0.776,特异性为0.637。 结论 T2DM患者肝脏脂肪含量与血清25(OH)D负相关,25(OH)D是T2DM发生NAFLD的保护因素。 Abstract:Objective This study aimed to investigate the correlation between controlled attenuation parameters (CAP) of the liver and serum 25-hydroxyvitamin D[25(OH)D] in patients with type 2 diabetes mellitus (T2DM). Methods A total of 160 patients with T2DM who were admitted to the First Affiliated Hospital of Bengbu Medical College from May 2019 to July 2020 were selected. On the basis of the CAP value, the patients were divided into the following groups: without NAFLD (43 patients), with mild NAFLD (35 patients), with moderate NAFLD (35 patients) and with severe NAFLD (47 patients). Vat, SAT, 25(OH)D and other biochemical indexes were measured, and differences in biochemical indexes amongst the groups were compared. Logistic regression analysis and Pearson or Spearman correlation analysis were performed, and ROC curve was used to analyse the optimal threshold of CAP for predicting vitamin D deficiency in patients with T2DM. Results 25(OH)D in the non-NAFLD group was significantly higher than that in the moderate and severe NAFLD groups, and 25(OH)D in the mild and moderate NAFLD groups was significantly higher than that in the severe NAFLD group (all P < 0.05). CAP was negatively correlated with 25(OH)D and HDL-C (r=-0.436, -0.193, all P < 0.05), whereas CAP was positively correlated with WHR, BMI, VAT, SAT, TC, TG, FINS, HOMA-IR, FFA, CRP, γ-GT and ALT (r= 0.276-0.447, all P < 0.05). 25(OH)D was negatively correlated with CAP, VAT, FBG, TC, TG, FFA, HOMA-IR, ALT, CRP and γ-GT (r=-0.436--0.156, all P < 0.05). Logistic regression analysis showed that FFA and 25(OH)D were the influencing factors for the development of NAFLD in T2DM. ROC curve showed that CAP265 dB/m as the diagnostic threshold had a sensitivity of 0.776 and a specificity of 0.637 for predicting vitamin D deficiency. Conclusion Liver fat content is negatively correlated with serum 25(OH)D in patients with T2DM, and 25(OH)D is a protective factor for NAFLD in T2DM. -
表 1 4组T2DM患者一般资料和生化指标比较[M(P25, P75)]
组别 例数 性别(男/女,例) 年龄(x±s, 岁) BMI(x±s) WHR VAT(x±s, cm2) SAT(x±s, cm2) 25(OH)D(x±s, ng/mL) 无NAFLD组 43 21/22 52.98±9.86 22.31±3.25 0.90(0.86, 0.92) 57.11±33.25 140.81±54.81 29.54±8.37 轻度NAFLD组 35 20/15 57.63±7.48 24.23±2.59c 0.93(0.90, 0.95)c 75.43±38.06c 182.01±54.85c 26.59±8.85 中度NAFLD组 35 19/16 53.80±13.87 25.48±2.43c 0.94(0.92, 0.96)c 89.05±29.11c 197.34±40.87c 23.65±9.94c 重度NAFLD组 47 26/21 54.83±12.04 25.70±3.28cd 0.93(0.91, 0.96)c 93.67±25.21cd 211.68±53.31cd 19.18±7.65cdf 统计量 0.630a 1.238b 11.765b 27.365e 11.737b 15.304b 11.611b P值 0.889 0.298 < 0.001 < 0.001 < 0.001 < 0.001 < 0.001 组别 例数 FBG(mmol/L) HbA1c(x±s, %) FINS(mIU/L) HOMA-IR TC(x±s, mmol/L) HDL-C(mmol/L) LDL-C(x±s, mmol/L) 无NAFLD组 43 6.80(5.11, 8.40) 10.05±1.96 3.97(2.00, 7.87) 1.30(0.79, 2.39) 3.94±0.93 0.97(0.86, 1.10) 2.67±0.82 轻度NAFLD组 35 7.60(5.75, 8.90) 9.53±2.74 5.84(3.05, 8.50) 1.74(1.06, 3.07) 4.03±1.53 0.99(0.78, 1.15) 2.37±1.15 中度NAFLD组 35 8.34(5.29, 10.59) 10.36±2.32 5.49(2.12, 9.26) 1.92(0.94, 3.30) 4.82±1.47cd 0.88(0.77, 1.03) 2.56±0.81 重度NAFLD组 47 7.01(5.84, 8.22) 9.07±1.80cf 8.54(5.18, 12.40)c 2.79(1.38, 4.11)c 5.05±1.46cd 0.89(0.77, 1.06) 2.63±0.89 统计量 3.749e 2.804b 13.170e 11.340e 7.059b 6.523e 0.775b P值 0.290 0.042 0.004 0.010 < 0.001 0.089 0.509 组别 例数 TG(mmol/L) FFA(mmol/L) ALT(U/L) AST(U/L) γ-GT(U /L) CRP(mg/L) 无NAFLD组 43 1.42(0.92, 2.17) 0.46(0.38, 0.57) 15(12, 19) 19(17, 23) 16(12, 25) 0.90(0.50, 1.30) 轻度NAFLD组 35 1.30(1.01, 2.04) 0.54(0.41, 0.70) 15(11, 18) 20(17, 21) 19(14, 34) 1.20(0.50, 2.57) 中度NAFLD组 35 2.10(1.55, 3.14)cd 0.62(0.47, 0.85)c 19(12, 34) 21(19, 27) 27(18, 55)c 1.50(0.60, 3.03)c 重度NAFLD组 47 2.10(1.48, 3.37)cd 0.65(0.47, 0.92)c 23(16, 36)cd 20(18, 27) 27(19, 40)c 1.70(0.90, 2.78)c 统计量 19.596e 24.165e 20.036e 6.621e 14.189e 17.157e P值 < 0.001 < 0.001 < 0.001 0.085 0.003 0.001 注:a为χ2值,b为F值;与无NAFLD组比较,cP < 0.05;与轻度NAFLD组比较,dP < 0.05;e为H值;与中度NAFLD组比较,fP < 0.05。 表 2 CAP与各指标的相关性分析
统计量 WHR BMI VAT SAT 25(OH)D TC TG FINS HOMA-IR HDL-C FFA CRP γ-GT ALT r值 0.392 0.454 0.447 0.474 -0.436 0.295 0.328 0.276 0.283 -0.193 0.337 0.369 0.281 0.313 P值 < 0.001 < 0.001 < 0.001 < 0.001 < 0.001 < 0.001 < 0.001 < 0.001 < 0.001 0.015 < 0.001 < 0.001 < 0.001 < 0.001 表 3 25(OH)D与各指标的相关性分析
统计量 CAP VAT FBG TC TG FFA HOMA-IR ALT γ-GT CRP r值 -0.436 -0.158 -0.241 -0.223 -0.215 -0.223 -0.168 -0.175 -0.156 -0.208 P值 < 0.001 0.047 0.002 0.005 0.006 0.005 0.034 0.027 0.049 0.008 表 4 T2DM患者发生NAFLD风险的影响因素
变量 B SE Wald χ2 P值 OR值 95% CI 常数项Constant -16.077 7.407 4.711 0.030 < 0.001 25(OH)D -0.103 0.034 9.020 0.003 0.902 0.844~0.965 FFA 6.498 1.836 12.531 < 0.001 663.772 18.176~24 239.753 -
[1] 洪文忠, 李奕萍. 血清γ-GT、CHE、Apelin及内脂素水平在非酒精性脂肪肝病患者中的诊疗价值[J]. 中华全科医学, 2020, 18(3): 463-466. https://www.cnki.com.cn/Article/CJFDTOTAL-SYQY202003034.htm [2] LALLUKKA S, YKI-JÄRVINEN H. Non-alcoholic fatty liver disease and risk of type 2 diabetes[J]. Best Pract Res Clin Endocrinol Metab, 2016, 30(3): 385-395. doi: 10.1016/j.beem.2016.06.006 [3] SAPONARO C, GAGGINI M, GASTALDELLI A. Nonalcoholic fatty liver disease and type 2 diabetes: common pathophysiologic mechanisms[J]. Current Diabetes Reports, 2015, 15(6): 1-13. doi: 10.1007%2Fs11892-015-0607-4.pdf [4] DING Y H, WEI T M, QIAN L Y, et al. Association between serum 25-hydroxyvitamin D and carotid atherosclerotic plaque in Chinese type 2 diabetic patients[J]. Medicine, 2017, 96(13): 6445. doi: 10.1097/MD.0000000000006445 [5] 董智慧. 老年2型糖尿病患者25羟维生素D与糖脂代谢、颈动脉内膜中层厚度的关系[J]. 中国老年学杂志, 2020, 40(9): 1820-1823. doi: 10.3969/j.issn.1005-9202.2020.09.010 [6] ALHEWISHEL MA, BAHGAT M, AL HUWAIYSHIL A, et al. 25(OH)D serum level in non-diabetic and type Ⅱ diabetic patients: a cross-sectional study[J]. Cureus, 2020, 12(6): e8910. http://www.researchgate.net/publication/342545548_25OHD_Serum_Level_in_Non-Diabetic_and_Type_II_Diabetic_Patients_A_Cross-Sectional_Study/download [7] 李静波, 刘姝, 温博, 等. FibroTouch与B超、CT对脂肪肝的诊断价值比较[J]. 临床肝胆病杂志, 2016, 32(3): 459-462. doi: 10.3969/j.issn.1001-5256.2016.03.011 [8] KIM J, LEE H, LIM J, et al. The angiogenesis inhibitor ALS-L1023 from lemon-balm leaves attenuates high-fat diet-induced nonalcoholic fatty liver disease through regulating the visceral adipose-tissue function[J]. Int J Mol Sci, 2017, 18(4): 846-881. doi: 10.3390/ijms18040846 [9] KO Y H, WONG T C, HSU Y Y, et al. The correlation between body fat, visceral fat, and nonalcoholic fatty liver disease[J]. Metab Syndr Relat Disord, 2017, 15(6): 304-311. doi: 10.1089/met.2017.0001 [10] KWOK R, CHOI K C, WONG G L, et al. Screening diabetic patients for non-alcoholic fatty liver disease with controlled attenuation parameter and liver stiffness measurements: a prospective cohort study[J]. Gut, 2016, 65(8): 1359-1368. doi: 10.1136/gutjnl-2015-309265 [11] 杨丽弘, 廖鑫, 张晗, 等. 2型糖尿病合并非酒精性脂肪肝肝纤维化与血清25-羟维生素D水平的关系研究[J]. 中国糖尿病杂志, 2018, 26(2): 117-122. doi: 10.3969/j.issn.1006-6187.2018.02.007 [12] 齐潇雁, 肖新华. 非酒精性脂肪肝与2型糖尿病研究进展[J]. 中国现代医药杂志, 2015, 17(12): 89-92. doi: 10.3969/j.issn.1672-9463.2015.12.032 [13] SILVAGNO F, PESCARMONA G. Spotlight on vitamin D receptor, lipid metabolism and mitochondria: Some preliminary emerging issues[J]. Mol Cell Endocrinol, 2017, 450: 24-31. doi: 10.1016/j.mce.2017.04.013 [14] BORGES C C, SALLES A F, BRINGHENTI I, et al. Vitamin D deficiency increases lipogenesis and reduces beta-oxidation in the liver of diet-induced obese mice[J]. J Nutr Sci Vitaminol (Tokyo), 2018, 64(2): 106-115. doi: 10.3177/jnsv.64.106 [15] 马世瞻, 赵家军. 内分泌与脂代谢[J]. 华西医学, 2018, 33(5): 491-498. https://www.cnki.com.cn/Article/CJFDTOTAL-HXYX201805001.htm -





 下载:
下载: