Analysis of pathological characteristics and prognosis of stages ⅠB1 and ⅡA2 cervical squamous cell carcinoma and adenocarcinoma
-
摘要:
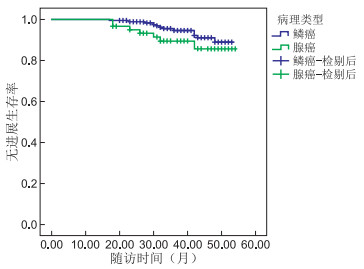
目的 探究ⅠB1~ⅡA2期宫颈鳞癌(squamous cell carcinoma, SCC)与腺癌(adenocarcinoma, AC)患者的病理特征、预后影响因素及其差异。 方法 回顾性分析2016年1月—2019年1月在蚌埠医学院第一附属医院接受宫颈癌根治术治疗的ⅠB1~ⅡA2期宫颈SCC和AC患者的260例临床资料,比较两者的病理特征、预后影响因素及差异。 结果 (1) SCC以外生菜花型为主,AC以内生浸润型为主(均P < 0.05);两者的年龄、肿瘤大小、浸润深度、细胞分化差异无统计学意义(均P>0.05);(2)ⅠB1~ⅡA2期宫颈SCC与AC 3年PFS(无进展生存期)分别为:94.6%、89.4%,差异无统计学意义(P>0.05),单因素log-rank分析示:临床分期、肿瘤大小、浸润深度均是ⅠB1~ⅡA2期宫颈SCC和AC预后影响因素,根据预后影响因素进一步分析,ⅠB1~ⅡA2期宫颈SCC与AC患者3年PFS在肿瘤大小、浸润深度、临床分期上差异均无统计学意义;将临床分期、肿瘤大小、浸润深度纳入多因素Cox回归模型分析示:临床分期是ⅠB1~ⅡA2期宫颈SCC与AC患者预后的独立危险因素(均P < 0.05)。 结论 ⅠB1~ⅡA2期宫颈SCC与AC的病理特征大致相似,AC以内生浸润型为主,易漏诊,宫颈管搔刮术(endocervical curettage, ECC)可明显降低AC漏诊率;根据术后的中危因素,采取合适的术后辅助治疗,ⅠB1~ⅡA2期宫颈SCC与AC患者可获得相同的预后。 Abstract:Objective To explore the pathological characteristics, prognostic factors and differences among patients with ⅠB1 and ⅡA2 cervical squamous cell carcinoma (SCC) and cervical adenocarcinoma (AC). Methods To retrospectively analyse the clinical data of 260 patients with stages ⅠB1 and ⅡA2 cervical SCC or AC who underwent radical resection of cervical cancer in the First Affiliated Hospital of Bengbu Medical College from January 2016 to January 2019. The differences in pathological characteristics, prognostic factors and between the two pathological types were compared. Results SCC was mainly the lettuce flower type, whereas AC was primarily the endogenous infiltrating type (all P < 0.05). Differences in age, tumour size, depth of invasion and cell differentiation between the two pathological types were not statistically significant. The 3-year progression-free survival (PFS) of stages ⅠB1 and ⅡA2 cervical SCC and AC was 94.6% and 89.4%, respectively, and the difference was not statistically significant. Log-rank analysis revealed that the clinical stage, tumour size and depth of invasion were all influencing factors on the prognosis of these two pathological types. Further analysis of the prognostic factors found no statistically significant difference in tumour size, depth of invasion and clinical stage among patients with stages ⅠB1 and ⅡA2 cervical SCC and AC at 3 years. Incorporating multiple predictors of survival such as clinical stage, tumour size and depth of invasion into Multivariable Cox regression analysis the result demonstrated that clinical stage was an independent risk factor for the prognosis of patients with stages ⅠB1 and ⅡA2 SCC and AC (all P < 0.05). Conclusion The pathological characteristics of stages ⅠB1 and ⅡA2 cervical SCC and AC are roughly similar. AC is mainly of endogenous infiltration type, and thus it can be easily missed. Endocervical curettage can substantially reduce the missed diagnosis rate of AC. In the presence of intermediate risk factors and with the conduct of appropriate a adjuvant therapy, after surgery the patients with stages ⅠB1 and ⅡA2 SCC and AC can achieve the same prognosis. -
表 1 ⅠB1~ⅡA2期宫颈SCC与AC的病理特征
病理特征 SCC AC 统计量 P值 临床分期 0.649a 0.516 ⅠB1 8 7 ⅠB2 59 15 ⅠB3 57 17 ⅡA1 30 15 ⅡA2 43 9 肿瘤大小(cm) 1.715b 0.190 < 4 97 37 ≥4 100 26 浸润深度 3.197b 0.074 < 1/2 72 31 ≥1/2 125 32 细胞分化 0.368a 0.713 Ⅰ级 11 4 Ⅱ级 119 39 Ⅲ级 67 20 生长类型 15.478b 0.002 外生菜花型 100 15 内生浸润型 85 44 溃疡型 6 3 糜烂型 6 1 注:a为Z值,b为χ2值。 表 2 ⅠB1~ⅡA2期宫颈SCC与AC预后影响因素的单因素分析
病理特征 例数 终点事件人数 3年PFS率(%) χ2值 P值 年龄(岁) 0.500 0.823 < 50 129 11 94.1 ≥50 124 11 92.6 临床分期 11.277 0.024 ⅠB1 15 0 100.0 ⅠB2 74 2 98.6 ⅠB3 74 7 95.5 ⅡA1 40 4 88.4 ⅡA2 50 9 84.5 肿瘤大小(cm) 5.581 0.018 < 4 129 6 95.6 ≥4 124 16 91.0 病理类型 0.729 0.393 SCC 192 15 94.6 AC 61 7 89.4 浸润深度 4.446 0.035 < 1/2 95 4 95.5 ≥1/2 158 18 91.9 细胞分化 3.893 0.143 Ⅰ级 15 0 100.0 Ⅱ级 154 11 92.6 Ⅲ级 84 11 93.6 生长类型 2.217 0.529 外生菜花型 110 10 91.3 内生浸润型 128 12 94.1 溃疡型 9 0 100.0 糜烂型 6 0 100.0 表 3 ⅠB1~ⅡA2期宫颈SCC与AC的3年PFS率比较(%)
组别 例数 肿瘤大小(cm) 浸润深度 临床分期 < 4 ≥4 < 1/2 ≥1/2 ⅠB ⅡA SCC 192 93.5(87/93) 90.9 (90/99) 97.1(66/68) 89.5 (111/124) 94.4(117/124) 88.2(60/68) AC 61 94.4(34/36) 80.0(20/25) 93.3(28/30) 83.9(26/31) 94.9(37/39) 77.3(17/22) χ2值 2.353 0.765 1.598 P值 0.672a 0.125 0.584a 0.382 0.999a 0.206 注:a为采用Fisher精确检验。 表 4 ⅠB1~ⅡA2期宫颈SCC与AC预后影响因素的多因素分析
病理特征 B SE Wald χ2 P值 OR值 95% CI 临床分期 0.882 0.441 3.998 0.04 2.416 1.018~5.731 肿瘤大小 0.807 0.493 2.681 0.102 2.242 0.853~5.891 浸润深度 0.706 0.573 1.518 0.218 2.025 0.659~6.223 -
[1] 刘萍. 中国大陆13年宫颈癌临床流行病学大数据评价[J]. 中国实用妇科与产科杂志, 2018, 34(1): 41-45. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGSF201801014.htm [2] YOKOI E, MABUCHI S, TAKAHASHI R, et al. Impact of histological subtype on survival in patients with locally advanced cervical cancer that were treated with definitive radiotherapy: adenocarcinoma/adenosquamous carcinoma versus squamous cell carcinoma[J]. J Gynecol Oncol, 2017, 28(2): e19. doi: 10.3802/jgo.2017.28.e19 [3] CAO L, WEN H, FENG Z, et al. Distinctive clinicopathologic characteristics and prognosis for different histologic subtypes of early cervical cancer[J]. Int J Gynecol Cancer, 2019, 29(8): 1244-1251. doi: 10.1136/ijgc-2019-000556 [4] XIE X, SONG K, CUI B, et al. A comparison of the prognosis between adenocarcinoma and squamous cell carcinoma in stage IB-IIA cervical cancer[J]. Int J Clin Oncol, 2018, 23(3): 522-531. doi: 10.1007/s10147-017-1225-8 [5] 胡君, 郑佩孜, 朱丽荣. ⅠB1期宫颈腺癌和鳞癌患者保留卵巢的临床病理特征比较[J]. 北京大学学报(医学版), 2016, 48(5): 783-787. doi: 10.3969/j.issn.1671-167X.2016.05.006 [6] WINER I, ALVARADO-CABRERO I, HASSAN O, et al. The prognostic significance of histologic type in early stage cervical cancer-A multi-institutional study [J]. Gynecol Oncol, 2015, 137(3): 474-478. doi: 10.1016/j.ygyno.2015.02.005 [7] 王一琳, 吴霞, 狄文. 宫颈腺癌与宫颈鳞癌的临床特征分析[J]. 实用妇产科杂志, 2015, 31(2): 150-152. https://www.cnki.com.cn/Article/CJFDTOTAL-SFCZ201502028.htm [8] 陈倩莹, 刘立峰, 金仙玉. 阴道镜诊断CIN的准确性及漏诊宫颈癌的相关因素分析[J]. 大连医科大学学报, 2019, 41(4): 325-328. https://www.cnki.com.cn/Article/CJFDTOTAL-DLYK201904013.htm [9] 米兰, 颛佳, 张岱, 等. 阴道镜下宫颈管搔刮术对宫颈高级别病变检出的作用[J]. 中国妇产科临床杂志, 2019, 20(2): 128-131. https://www.cnki.com.cn/Article/CJFDTOTAL-FKLC201902013.htm [10] 郭艳会, 强金伟. 磁共振扩散相关成像技术在宫颈癌诊治中的研究进展[J]. 中国医学计算机成像杂志, 2020, 26(1): 93-96. doi: 10.3969/j.issn.1006-5741.2020.01.021 [11] 朱林林, 王海燕, 颜宪书, 等. 超声造影与核磁共振成像对宫颈癌病灶和侵犯程度评估的一致性[J]. 中华全科医学, 2019, 17(11): 1889-1892. https://www.cnki.com.cn/Article/CJFDTOTAL-SYQY201911027.htm [12] SAIDA T, SAKATA A, TANAKA Y O, et al. Clinical and MRI characteristics of uterine cervical adenocarcinoma: Its variants and mimics [J]. Korean J Radiol, 2019, 20(3): 364-377. doi: 10.3348/kjr.2018.0458 [13] WU S G, SUN J Y, HE Z Y, et al. Early-stage node negative cervical adenocarcinoma and squamous cell carcinoma show similar survival outcomes after hysterectomy: a population-based study[J]. J Gynecol Oncol, 2017, 28(6): e81. doi: 10.3802/jgo.2017.28.e81 [14] ZHOU J, ZHANG W W, WU S G, et al. The prognostic value of histologic subtype in node-positive early-stage cervical cancer after hysterectomy and adjuvant radiotherapy[J]. Int J Surg, 2017, 44: 1-6. doi: 10.1016/j.ijsu.2017.05.074 [15] CHEN J, WANG R, ZHANG B, et al. Safety of ovarian preservation in women with stage I and II cervical adenocarcinoma: a retrospective study and meta-analysis [J]. Am J Obstet Gynecol, 2016, 215(4): 460. e1-e13. doi: 10.1016/j.ajog.2016.04.023 [16] KATO T, WATARI H, TAKEDA M, et al. Multivariate prognostic analysis of adenocarcinoma of the uterine cervix treated with radical hysterectomy and systematic lymphadenectomy[J]. J Gynecol Oncol, 2013, 24(3): 222-228. doi: 10.3802/jgo.2013.24.3.222 [17] 乌守恒, 曾晓峰, 王萍, 等. 宫颈癌组织中c-myc、bcat1的表达及其临床意义[J]. 四川大学学报(医学版), 2018, 49(5): 725-730. https://www.cnki.com.cn/Article/CJFDTOTAL-HXYK201805008.htm [18] 葛莉莉, 叶春萍, 余宁珠. 宫颈鳞癌及腺癌手术患者淋巴结分布及转移的特点差异分析[J]. 中国妇产科临床杂志, 2017, 18(5): 395-397. https://www.cnki.com.cn/Article/CJFDTOTAL-FKLC201705004.htm [19] 贾海清, 王安娜, 龙再秋. 早期子宫颈腺癌预后影响因素分析[J]. 中国实用妇科与产科杂志, 2019, 35(12): 1374-1378. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGSF201912023.htm [20] BHATLA N, DENNY L. FIGO Cancer Report 2018[J]. Int J Gynaecol Obstet, 2018, 143(Suppl 2): 2-3. [21] HU K, WANG W, LIU X, et al. Comparison of treatment outcomes between squamous cell carcinoma and adenocarcinoma of cervix after definitive radiotherapy or concurrent chemoradiotherapy[J]. Radiat Oncol, 2018, 13(1): 249. doi: 10.1186/s13014-018-1197-5 [22] HOU Y, GUO S, LYU J, et al. Prognostic factors in Asian and white American patients with cervical cancer, considering competing risks[J]. Curr Oncol, 2019, 26(3): 277-285. doi: 10.3747/co.26.4473 [23] 黄裕, 雷海科, 陈文娟, 等. 老年宫颈癌患者治疗结局及预后分析[J]. 中华肿瘤防治杂志, 2018, 25(6): 428-432. https://www.cnki.com.cn/Article/CJFDTOTAL-QLZL201806010.htm [24] MABUCHI Y, YAHATA T, KOBAYASHI A, et al. Clinicopathologic factors of cervical adenocarcinoma stages IB to IIB[J]. Int J Gynecol Cancer, 2015, 25(9): 1677-1682. doi: 10.1097/IGC.0000000000000542 -





 下载:
下载: