Expressions of TLR9 and STAT3 and their correlation with IL-10 in patients with ulcerative colitis
-
摘要:
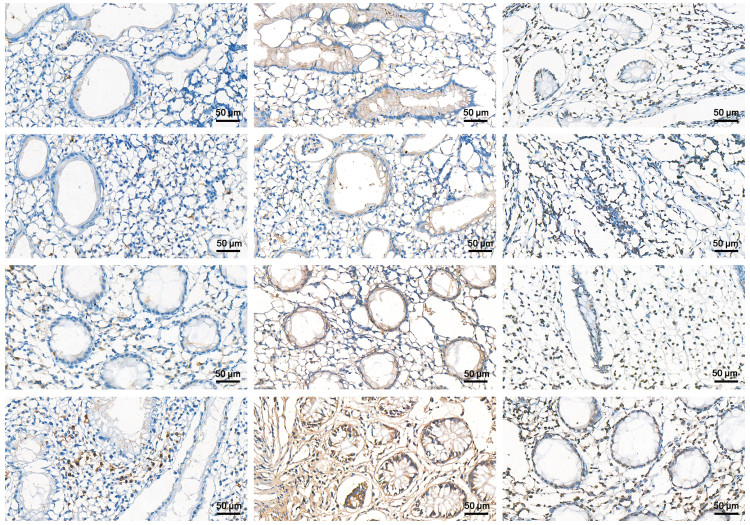
目的 检测Toll样受体9(TLR9)、信号转导与转录活化因子3(STAT3)及白介素10(IL-10)在溃疡性结肠炎(ulcerative colitis,UC)患者外周血及肠黏膜组织中的表达水平, 探讨它们在UC发病中的作用及其相互关系。 方法 选取2019年7月—2020年7月在蚌埠医学院第一附属医院诊治的32例UC患者归为实验组,30例健康体检者纳入正常对照组,其中实验组又分为轻度(10例)、中度(14例)及重度组(8例)。检测外周血单个核细胞中TLR9 mRNA和STAT3 mRNA的表达和血清IL-10水平及肠黏膜组织中TLR9、STAT3及IL-10蛋白表达水平。 结果 实验组UC患者TLR9 mRNA和STAT3 mRNA的表达水平均高于正常对照组(均P < 0.05);血清中IL-10的表达水平明显低于正常对照组(P < 0.05)。肠黏膜组织中TLR9、STAT3的蛋白表达水平均高于正常对照组(均P < 0.05),IL-10蛋白表达水平低于正常对照组(P < 0.05)。TLR9 mRNA和STAT3 mRNA、TLR9和STAT3蛋白表达水平之间均呈正相关,血清IL-10与TLR9 mRNA、STAT3 mRNA表达水平呈负相关,肠黏膜组织IL-10与TLR9、STAT3蛋白表达水平呈负相关。 结论 TLR9、STAT3、IL-10共同参与了UC的发生和发展,在UC的发病机制中TLR9和STAT3可能参与了IL-10的表达与调控。 -
关键词:
- 溃疡性结肠炎 /
- Toll样受体9 /
- 信号转导与转录活化因子3 /
- 白介素10
Abstract:Objective The expression levels of toll-like receptor 9 (TLR9), signal transduction and transcriptional activator factor 3 (STAT3) and interleukin-10 (IL-10) in peripheral blood and intestinal mucosal tissues of patients with ulcerative colitis (UC) were detected to explore their roles in the pathogenesis of UC and their correlation. Methods Thirty-two patients with UC treated in the First Affiliated Hospital of Bengbu Medical College from July 2019 to July 2020 were selected as the experimental group; and 30 healthy subjects according to the results of physical examination were included in the normal control group. The experimental group was further divided into mild group (n=10), moderate group (n=14) and severe (n=8) group. The expressions of TLR9 and STAT3 mRNA in peripheral blood mononuclear cells, serum IL-10 levels and TLR9, as well as levels of STAT3 and IL-10 proteins, in intestinal mucosal tissues were detected. Results The expression levels of TLR9 mRNA and STAT3 mRNA in the experimental group were both higher than those in the control group (all P < 0.05). The expression level of IL-10 in serum in the experimental group was significantly lower than that in the normal control group (P < 0.05). The expression levels of TLR9 and STAT3 in intestinal mucosal tissues were all higher than that in the normal control group (all P < 0.05). By contrast, the expression levels of IL-10 in the experimental group were lower than that in the normal control group (P < 0.05). Expressions of TLR9 mRNA and STAT3 mRNA and TLR9 and STAT3 mRNA were positively correlated. Serum IL-10 was negatively correlated with TLR9 and STAT3 mRNA expression levels. Intestinal mucosal IL-10 was negatively correlated with TLR9 and STAT3 protein expression levels. Conclusion TLR9, STAT3 and IL-10 are jointly involved in the occurrence and development of UC. TLR9 and STAT3 may be involved in the expression and regulation of IL-10 in the pathogenesis of UC. -
Key words:
- Ulcerative colitis /
- Toll like receptors 9 /
- STAT3 /
- interleukin-10
-
表 1 RT-PCR引物系列及产物长度一览表
基因 引物方向 引物序列(5' -3') 扩增产物
长度(bp)TLR9 上游引物 ACTGGCTGTTCCTGAAGTCTGTG 254 下游引物 CAGGTTTAGCTCTTCCAGGGTG STAT3 上游引物 GAGAAGGACATCAGCGGTAAG 138 下游引物 CAGTGGAGACACCAGGATATTG β-actin 上游引物 GGAAGCTTGTCATCAATGGAAATC 168 下游引物 TGATGACCCTTTTGGCTCCC 表 2 各组TLR9 mRNA、STAT3 mRNA水平及IL-10表达
(x ±s,ng/mL) 组别 分级 例数 TLR9 STAT3 IL-10 对照组 30 0.80±0.12 0.83±0.13 56.56±7.11 实验组 轻度 10 0.98±0.05a 1.23±0.06a 44.61±2.53a 中度 14 1.15±0.09ab 1.31±0.13a 35.54±6.09ab 重度 8 1.56±0.28abc 1.82±0.14abc 28.78±3.37abc F值 70.183 145.237 67.395 P值 < 0.001 < 0.001 < 0.001 注:与对照组比较, aP < 0.05;与轻度组比较, bP < 0.05;与中度组比较,cP < 0.05。 表 3 各组TLR9、STAT3及IL-10蛋白表达水平的平均吸光度值
(x ±s,ng/mL) 组别 分级 例数 TLR9 STAT3 IL-10 对照组 30 0.28±0.09 0.23±0.12 1.98±0.19 实验组 轻度 10 0.60±0.10a 0.81±0.22a 1.36±0.05a 中度 14 0.95±0.09ab 1.08±0.09ab 0.88±0.14ab 重度 8 1.73±0.23abc 2.07±0.18abc 0.60±0.11abc F值 351.765 377.283 268.492 P值 < 0.001 < 0.001 < 0.001 注:与对照组比较, aP < 0.05;与轻度组比较, bP < 0.05;与中度组比较,cP < 0.05。 表 4 TLR9 mRNA、STAT3 mRNA及IL-10之间的相关性
指标 r值 P值 TLR9/STAT3 0.809 < 0.001 TLR9/IL-10 -0.749 < 0.001 STAT3/IL-10 -0.838 < 0.001 表 5 TLR9、STAT3及IL-10蛋白表达水平之间的相关性
指标 r值 P值 TLR9/STAT3 0.940 < 0.001 TLR9/IL-10 -0.892 < 0.001 STAT3/IL-10 -0.898 < 0.001 -
[1] PINETON DE CHAMBRUN G, TASSY B, KOLLEN L, et al. The treatment of refractory ulcerative colitis[J]. Best Pract Res Clin Gastroenterol, 2018, 32-33: 49-57. doi: 10.1016/j.bpg.2018.05.009 [2] 刘梦莹, 王启之. TLR9/NF-κBp65信号通路与溃疡性结肠炎[J]. 胃肠病学和肝病学杂志, 2015, 24(9): 1149-1151. https://www.cnki.com.cn/Article/CJFDTOTAL-WCBX201509033.htm [3] ATREYA R, REINISCH W, PEYRIN-BIROULET L, et al. Clinical efficacy of the Toll-like receptor 9 agonist cobitolimod using patient-reported-outcomes defined clinical endpoints in patients with ulcerative colitis[J]. Dig Liver Dis, 2018, 50(10): 1019-1029. doi: 10.1016/j.dld.2018.06.010 [4] BORZUTZKY A, RAUTER I, FRIED A, et al. Defective TLR9-driven STAT3 activation in B cells of patients with CVID[J]. Clin Immunol, 2018, 197: 40-44. doi: 10.1016/j.clim.2018.08.008 [5] 吴开春, 梁洁, 冉志华, 等. 炎症性肠病诊断与治疗的共识意见(2018年·北京)[J]. 中国实用内科杂志, 2018, 38(9): 796-813. https://www.cnki.com.cn/Article/CJFDTOTAL-SYNK201809007.htm [6] RUBIN D T, ANANTHAKRISHNAN A N, SIEGEL C A, et al. ACG Clinical Guideline: Ulcerative Colitis in Adults[J]. Am J Gastroenterol, 2019, 114(3): 384-413. doi: 10.14309/ajg.0000000000000152 [7] UNGARO R, MEHANDRU S, ALLEN P B, et al. Ulcerative colitis[J]. Lancet, 2017, 389(10080): 1756-1770. doi: 10.1016/S0140-6736(16)32126-2 [8] TAKEDA K, AKIRA S. Toll-Like Receptors[J]. Curr Protoc Immunol, 2015. DOI: 10.1002/0471142735.im1412s109. [9] BING X, XUELEI L, WANWEI D, et al. EGCG maintains Th1/Th2 balance and mitigates ulcerative colitis induced by dextran sulfate sodium through TLR4/MyD88/NF-κB signaling pathway in rats[J]. Can J Gastroenterol, 2017, 2017: 3057268. http://europepmc.org/abstract/MED/29404307 [10] ANTHONEY N, FOLDI I, HIDALGO A. Toll and Toll-like receptor signalling in development[J]. Development, 2018, 145(9): dev156018. doi: 10.1242/dev.156018 [11] SCHMITT H, ULMSCHNEIDER J, BILLMEIER U, et al. The TLR9 agonist cobitolimod induces IL10-producing wound healing macrophages and regulatory T cells in ulcerative colitis[J]. J Crohns Colitis, 2020, 14(4): 508-524. doi: 10.1093/ecco-jcc/jjz170 [12] TIAN L, LI Y, ZHANG J, et al. IL-9 promotes the pathogenesis of ulcerative colitis through STAT3/SOCS3 signaling[J]. Biosci Rep, 2018, 38(6): BSR20181521. doi: 10.1042/BSR20181521 [13] CHEN Y Y, MA Z B, XU H Y, et al. IL-6/STAT3/SOCS3 signaling pathway playing a regulatory role in ulcerative colitis carcinogenesis[J]. Int J Clin Exp Med, 2015, 8(8): 12009-12017. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4612798/pdf/ijcem0008-12009.pdf [14] JOFRA T, GALVANI G, COSORICH I, et al. Experimental colitis in IL-10-deficient mice ameliorates in the absence of PTPN22[J]. Clin Exp Immunol, 2019, 197(3): 263-275. doi: 10.1111/cei.13339 [15] BISWAS A, SHOUVAL D S, GRIFFITH A, et al. WASP-mediated regulation of anti-inflammatory macrophages is IL-10 dependent and is critical for intestinal homeostasis[J]. Nat Commun, 2018, 9(1): 1779. doi: 10.1038/s41467-018-03670-6 -





 下载:
下载: