Relationship between preoperative NLR and PLR and clinicopathological characteristics and T stage after laparoscopic radical resection of hilar cholangiocarcinoma
-
摘要:
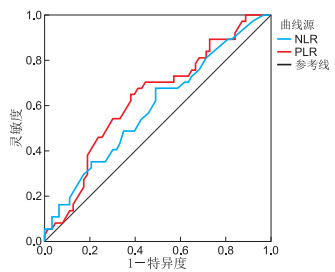
目的 收集近10年本科室肝门胆管癌(HC)患者的病例资料。研究术前中性粒细胞与淋巴细胞比(NLR)和血小板与淋巴细胞比(PLR)与HC临床病理特征及T分期的关系。 方法 回顾性分析2010年1月—2019年12月在蚌埠医学院第一附属医院肝胆外科术后病理为HC患者的资料,共有100例患者被纳入。通过受试者工作特征(ROC)曲线确定NLR和PLR的最佳截止值,统计分析术前NLR和PLR与HC病理特征及T分期的关系, 以及对T分期的预测价值。 结果 ROC曲线确定最佳截止值,高NLR组(NLR>4.12, 56例)和低NLR组(NLR≤4.12, 44例);高PLR组(>184.56, 48例)和低PLR组(≤184.56,52例)。单因素分析表明,术前NLR与肿瘤位置和T分期有相关性(均P < 0.05),与性别、年龄、分化程度、肿瘤大小等无关(均P > 0.05);术前PLR与T分期、肿瘤大小和淋巴结转移有相关性(均P < 0.05), 与性别、年龄、分化程度、肿瘤位置等无关(均P > 0.05)。多因素分析结果表明,术前NLR与T分期(OR=2.999, P=0.026)和肿瘤位置(OR=0.346, P=0.032)有关;术前PLR与T分期(OR=3.635, P=0.007)和肿瘤大小(OR=1.728, P=0.031)有关,与淋巴结转移转移无关(P > 0.05)。术前NLR和PLR的ROC曲线面积为0.811和0.794,对T分期有预测价值。 结论 术前NLR和PLR是一种简单、实用的检测指标,可用于术前对HC病理特征的评估,对T分期有预测价值。 -
关键词:
- 肝门胆管癌 /
- 中性粒细胞与淋巴细胞比 /
- 血小板与淋巴细胞比
Abstract:Objective To study the relationship between preoperative neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR) with the clinicopathological characteristics and T staging of hilar cholangiocarcinoma (HC). Methods The data of patients with HC were analyzed retrospectively. The receiver operating characteristic (ROC) curve was used to determine the best cut-off values of NLR and PLR. Statistical analysis of preoperative NLR and PLR and HC pathological characteristics and the relationship between T staging and the predictive value of T staging. Results The ROC curve was used to determine the best cut-off value: high-NLR group (NLR>4.12, 56 cases), low-NLR group (NLR≤4.12, 44 cases), high-PLR group (>184.56, 48 cases) and low-PLR group (≤184.56, 52 cases). Univariate analysis showed that preoperative NLR was correlated with tumour location and T stage (all P < 0.05) and had no correlation with gender, age, degree of differentiation and tumour size (all P > 0.05). Preoperative PLR was correlated with T stage, tumour size and lymph node metastasis (all P < 0.05) and had no correlation with gender, age, degree of differentiation and tumour location (all P > 0.05). Multivariate analysis showed that preoperative NLR was associated with T staging (OR=2.999, P=0.026) and tumour location (OR=0.346, P=0.032). Preoperative PLR was related to T stage (OR=3.635, P=0.007) and tumour size (OR=1.728, P=0.031), but not to lymph node metastasis (P > 0.05). The ROC curve areas of NLR and PLR before surgery were 0.811 and 0.794, respectively, which have predictive value for T staging. Conclusion Preoperative NLR and PLR are simple and practical detection indicators that can be used to evaluate the pathological characteristics of HC before surgery and have predictive value for T staging. -
表 1 术前NLR水平与100例肝门胆管癌患者临床病理特征的关系(例)
项目 类别 例数 NLR χ2值 P值 高NLR组 低NLR组 性别 男性 67 39 28 0.402 0.526 女性 33 17 16 年龄(岁) >63 54 27 27 1.715 0.190 ≤63 46 29 17 分化程度 高 6 2 4 中 73 42 31 1.332 0.906 低 21 12 9 T分期 ≥T2b 45 18 27 8.501 0.004 <T2b 55 38 17 肿瘤大小(cm) >2.5 45 30 15 3.778 0.052 ≤2.5 55 26 29 肿瘤位置 汇合部以上 52 35 17 5.622 0.018 汇合部及以下 48 21 27 淋巴结转移 阳性 37 25 12 3.189 0.074 阴性 63 31 32 TNM分期 >Ⅱ期 40 25 15 1.143 0.285 ≤Ⅱ期 60 31 29 表 2 术前PLR水平与100例肝门胆管癌患者临床病理特征的关系(例)
项目 类别 例数 PLR χ2值 P值 高PLR组 低PLR组 性别 男性 67 33 34 0.128 0.721 女性 33 15 18 年龄(岁) >63 54 22 32 2.478 0.115 ≤63 46 26 20 分化程度 高 6 1 5 4.046 0.132 中 73 39 34 低 21 8 13 T分期 ≥T2b 45 14 31 9.350 0.002 <T2b 55 34 21 肿瘤大小(cm) >2.5 45 27 18 4.720 0.030 ≤2.5 55 21 34 肿瘤位置 汇合部以上 52 29 23 2.620 0.106 汇合部及以下 48 19 29 淋巴结转移 阳性 37 24 13 6.692 0.010 阴性 63 24 39 TNM分期 >Ⅱ期 40 24 16 2.620 0.106 ≤Ⅱ期 60 24 36 表 3 术前NLR与100例肝门胆管癌患者临床病理特征关系的多因素分析
影响因素 B SE Wald χ2 P值 OR(95%CI) T分期 0.949 0.425 4.993 0.026 2.999(1.138~7.901) 肿瘤位置 0.894 0.425 4.420 0.032 0.346(0.131~0.911) 表 4 术前PLR与100例肝门胆管癌患者临床病理征特征关系的多因素分析
影响因素 B SE Wald χ2 P值 OR(95%CI) T分期 -1.137 0.447 6.466 0.007 3.635(1.416~9.333) 肿瘤大小 1.105 0.448 6.074 0.031 1.728(1.050~2.846) 淋巴结转移 0.158 0.442 0.127 0.721 1.171(0.493~2.783) -
[1] RIZVI S, KHAN S A, HALLEMEEIER C L, et al. Cholangiocarcinomaevolving concepts and therapeutic strategies[J]. Nat Rev Clin Oncol, 2018, 15(2): 95-111. doi: 10.1038/nrclinonc.2017.157 [2] ABDULLAH M, STUART R, JEREMY F, et al. Surgery for hilar cholangiocarcinoma: The newcastle upon tyne liver unit experience[J]. Eur Surg, 2019, 51(4): 197-205. doi: 10.1007/s10353-019-0599-4 [3] JEROEN L, VAN V, MARCIA P, et al. The prognostic value of portal vein and hepatic artery involvement in patients with perihilar cholangiocarcinoma[J]. HPB, 2018, 20(1): 83-92. doi: 10.1016/j.hpb.2017.08.025 [4] MICHAEL E, WILLIAM R. Surgical management of hilar cholangiocarcinoma at memorial sloan kettering cancer center[J]. Ann Gastroenterol Surg, 2018, 2(4): 304-312. doi: 10.1002/ags3.12181 [5] SONG X, WANG Y, ZHANG A, et al. Advances in research on the interaction between inflammation and cancer[J]. J Int Med Res, 2019, 48(4): 300060519895347. http://www.ncbi.nlm.nih.gov/pubmed/31885347 [6] ALLER M, ARIAS A, ARIAS J, et al. Carcinogenesis: The cancer cell-mast cell connection[J]. Inflamm Res, 2019, 68(2): 103-116. doi: 10.1007/s00011-018-1201-4 [7] HUSZNO J, KOLOSZA Z, MROCHEM J, et al. The role of neutrophil-lymphocyte ratio, platelet-lymphocyte ratio, and platelets in the prognosis of metastatic renal cell carcinoma[J]. Oncology, 2019, 97(1): 1-11. doi: 10.1159/000499583 [8] 侯仕强, 金春景, 石碑田, 等. 术前NLR、PLR和MLR在胶质瘤患者预后中的应用研究[J]. 中华全科医学, 2020, 18(7): 1118-1121. https://www.cnki.com.cn/Article/CJFDTOTAL-SYQY202007016.htm [9] SAKAI M, SOHDA M, SAITO H, et al. Impact of combined assessment of systemic inflammation and presarcopenia on survival for surgically resected esophageal cancer[J]. Am J Surg, 2021, 221(1): 149-154. doi: 10.1016/j.amjsurg.2020.05.029 [10] 冯志强, 郭玉明, 赵君会, 等. 行肝切除术肝细胞癌患者炎性指标水平变化及与预后的相关性[J]. 中华实用诊断与治疗杂志, 2020, 34(9): 891-895. https://www.cnki.com.cn/Article/CJFDTOTAL-HNZD202009007.htm [11] ZHANG X, ZHAO W, YU Y, et al. Clinicopathological and prognostic significance of platelet-lymphocyte ratio (PLR) in gastric cancer: An updated meta-analysis[J]. World J Surg Oncol, 2020, 18(1): 191-203. doi: 10.1186/s12957-020-01952-2 [12] 孙家和, 刘元, 李志祥, 等. 术前中性粒细胞/淋巴细胞比值对cN0期甲状腺微小乳头状癌中央区淋巴结转移的预测价值[J]. 中华全科医学, 2020, 18(12): 2006-2009. https://www.cnki.com.cn/Article/CJFDTOTAL-SYQY202012009.htm [13] ZHU W, XIE W, ZHANG Z, et al. Postoperative complications and survival analysis of surgical resection for hilar cholangiocarcinoma: A retrospective study of fifty-nine consecutive patients[J]. Chin Med Sci J, 2020, 35(2): 157-169. http://www.sciencedirect.com/science/article/pii/S1001929420300353 [14] CHUN Y, PAWLIK T, VAUTHEY J. 8th edition of the AJCC cancer staging manual: Pancreas and hepatobiliary cancers[J]. Ann Surg Oncol, 2018, 25(4): 845-847. doi: 10.1245/s10434-017-6025-x [15] DREYER S, POWELL A, MCSORLEY S, et al. The pretreatment systemic inflammatory response is an important determinant of poor pathologic response for patients undergoing neoadjuvant therapy for rectal cancer[J]. Ann Surg Oncol, 2017, 24(5): 1295-1303. doi: 10.1245/s10434-016-5684-3 [16] PENG H, LUO X. Prognostic significance of elevated pretreatment systemic inflammatory markers for patients with prostate cancer: A meta-analysis[J]. Cancer Cell Int, 2019, 19(1): 70-88. doi: 10.1186/s12935-019-0785-2 [17] RAKIC A, BEAUDRY P, MAHONEY D. The complex interplay between neutrophils and cancer[J]. Cell Tissue Res, 2018, 371(3): 517-529. doi: 10.1007/s00441-017-2777-7 [18] VASUNDHARA S, MANU D, MANIKA V, et al. Systemic delivery of the tumor necrosis factor gene to tumors by a novel dual DNA-nanocomplex in a nanoparticle system[J]. Nanomedicine, 2017, 13(5): 1833-1839. doi: 10.1016/j.nano.2017.03.004 [19] SONG W, PARTH T, DAVID A, et al. Conditioned medium from stimulated macrophages inhibits growth but induces an inflammatory phenotype in breast cancer cells[J]. Biomed Pharmacother, 2018, 106(10): 247-254. http://www.onacademic.com/detail/journal_1000040417512910_fa57.html [20] SUDAN S, DESHMUKH S, POOSARLA T, et al. Resistin: An inflammatory cytokine with multi-faceted roles in cancer[J]. BBA-Reviews on Cancer, 2020, 1874(2): 188419-188428. http://www.ncbi.nlm.nih.gov/pubmed/32822824 [21] FENG Y, WANG J, TAN D, et al. Relationship between circulating inflammatory factors and glioma risk and prognosis: A meta-analysis[J]. Cancer Med, 2019, 8(17): 7454-7468. doi: 10.1002/cam4.2585 [22] CHUAN T, WEI S, XIA T, et al. Prognostic significance of platelet-to-lymphocyte ratio in patients with ovarian cancer: A meta-analysis[J]. Eur J Clin Invest, 2018, 48(5): e12917. doi: 10.1111/eci.12917 [23] GIAKOUSTIDIS A, NEOFYTOU K, C0STA N, et al. Identifying the role of neutrophil-to-lymphocyte ratio and platelets-to-lymphocyte ratio as prognostic markers in patients undergoing resection of pancreatic ductal adenocarcinoma[J]. J Hepatobiliary Pancreat Surg, 2018, 22(3): 197-207. doi: 10.14701/ahbps.2018.22.3.197 [24] PORTIER I, CAMPBELL R. Role of platelets in detection and regulation of infection[J]. Arterioscler Thromb Vasc Biol, 2021, 41(1): 70-78. http://www.ncbi.nlm.nih.gov/pubmed/33115274 [25] PLANTUREUX L, MEGE D, CRESCENCE L, et al. Impacts of cancer on platelet production, activation and education and mechanisms of cancer-associated thrombosis[J]. Cancers, 2018, 10(11): 441-464. doi: 10.3390/cancers10110441 [26] HU H, JIN Y, ZHOU R, et al. Clinical value of inflammation-based prognostic scores to predict the resectability of hyperbilirubinemia patients with potentially resectable hilar cholangiocarcinoma[J]. J Gastrointest Surg, 2019, 23(3): 510-517. doi: 10.1007/s11605-018-3892-9 -





 下载:
下载: