Association of related markers in blood routine examination with diagnosis and severity of acute cerebral infarction
-
摘要:
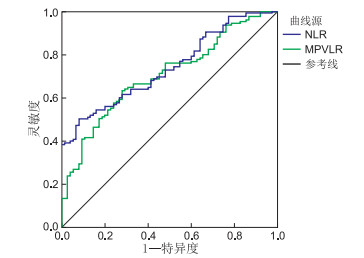
目的 探讨血常规检验中性粒细胞/淋巴细胞比值(NLR)、平均血小板体积/淋巴细胞比值(MPVLR)与急性脑梗死(acute cerebral infarction, ACI)发病及严重程度之间的关系。 方法 收集安徽医科大学附属巢湖医院2018年8月—2020年6月收治的125例发病24 h内入院ACI患者作为研究对象,根据美国国立卫生研究院卒中量表(NIHSS)评分将其分为轻型ACI组(NIHSS < 5分,70例)和中重型ACI组(NIHSS≥5分,55例)。收集同一时期在安徽医科大学附属巢湖医院体检中心检查的75名健康人群为对照组。采用ROC曲线分析NLR、MPVLR预测ACI发病的价值。通过Pearson相关分析法评估中性粒细胞(NE)、NLR、MPVLR、血小板/中性粒细胞比值(PNR)、淋巴细胞(LYM)与NIHSS评分的相关性。采用多因素logistic回归模型分析脑梗死严重程度的独立危险因素。 结果 ACI组的平均血小板体积(MPV)、NLR、MPVLR水平显著高于对照组,LYM、PNR水平显著低于对照组;中重型ACI组患者的NLR、MPVLR水平均显著高于轻型ACI组,LYM、PNR水平低于轻型ACI组,差异均有统计学意义(均P < 0.05)。NLR、MPVLR诊断ACI曲线下面积分别为0.739(0.672~0.806)、0.704(0.632~0.776)。ACI患者NE、NLR、MPVLR水平与NIHSS评分呈正相关(r=0.475、0.582、0.220,均P < 0.05),ACI患者PNR、LYM水平与NIHSS评分呈负相关(r=-0.359、-0.223,均P < 0.05)。NLR为ACI严重程度的独立危险因素(P < 0.05)。 结论 NLR、MPVLR与ACI发病及病情进展密切相关,NLR可能为ACI严重程度的独立危险因素,监测NLR、MPVLR水平对ACI患者病情评估及早期干预治疗具有指导价值。 -
关键词:
- 中性粒细胞淋巴细胞比值 /
- 平均血小板体积淋巴细胞比值 /
- 急性脑梗死 /
- 血常规
Abstract:Objective To investigate the relationship between diagnosis and severity of acute cerebral infarction (ACI) and neutrophil/lymphocyte ratio (NLR) and mean platelet volume/lymphocyte ratio (MPVLR). Methods From October August 2018 to June 2020, 125 ACI patients from Chaohu Hospital Affiliated to Anhui Medical University who were admitted within 24 h after onset were enrolled. They were divided into the mild ACI group (NIHSS < 5 points, n=70) and moderate and severe ACI group (NIHSS ≥ 5 points, n=55) according to the National Institutes of Health Stroke Scale (NIHSS) score. Another 75 healthy volunteers examined in our physical examination centre were selected as the control group. The values of NLR and MPVLR in predicting ACI were determined by constructing receiver operating characteristic curves. Pearson correlation analysis was used to evaluate the correlation between NE, NLR, MPVLR, PNR, and LYM and NIHSS score. The independent risk factors of ACI severity were analysed by multivariate logistic regression analysis. Results Serum MPV, NLR and MPVLR levels in the ACI group were significantly higher, whilst the levels of LYM and PNR were significantly lower than those of the control group (P < 0.05). The levels of NLR and MPVLR in the moderate and severe ACI group were significantly higher, whilst the levels of PNR and LYM were obviously lower than those in the mild ACI group (P < 0.05). The areas under the curve of NLR and MPVLR to predict ACI were 0.739 (0.672-0.806) and 0.704 (0.632-0.776), respectively. The NE, NLR and MPVLR levels in ACI were positively correlated with the NIHSS score (r=0.475, 0.582, 0.220, P < 0.05). The PNR and LYM levels were negatively correlated with the NIHSS score (r=-0.359, -0.223, P < 0.05). NLR was an independent risk factor for the severity of ACI (P < 0.05). Conclusion NLR and MPVLR have certain clinical significance for ACI diagnosis and evaluating the severity of ACI. NLR may be an independent risk factor for the severity of ACI. Monitoring these two indicators has a certain guiding value for the early evaluation and treatment of ACI. -
表 1 3组研究对象一般临床资料比较
组别 例数 年龄
(x±s,岁)性别[例(%)] 高血压
[例(%)]糖尿病
[例(%)]吸烟史
[例(%)]饮酒史
[例(%)]冠心病
[例(%)]女性 男性 对照组 75 63.73±6.08 31(41.3) 44(58.7) 35(46.7) 16(21.3) 12(16.0) 10(13.3) 7(9.3) 轻型ACI组 70 64.20±9.97 29(41.4) 41(58.6) 40(57.1) 22(31.4) 15(21.4) 12(17.1) 10(14.3) 中重型ACI组 55 66.62±10.01 24(43.6) 31(56.3) 33(60.0) 10(18.1) 10(18.1) 13(23.6) 8(14.5) 统计量 1.904a 0.084b 2.699b 3.431b 0.713b 2.343b 1.102b P值 0.152 0.959 0.259 0.680 0.700 0.310 0.576 注:a为F值,b为χ2值。 表 2 ACI组与对照组血常规相关指标比较(x±s)
组别 例数 WBC
(×109/L)RBC
(×1012/L)NE
(×109/L)LYM
(×109/L)PLT
(×109/L)MPV
(fL)NLR PNR MPVLR 对照组 75 6.16±1.61 4.60±0.47 3.57±0.93 1.94±0.61 205.17±52.35 11.64±1.26 1.91±0.54 60.95±20.99 6.43±1.81 ACI组 125 7.04±2.67 4.33±0.55 4.80±2.50 1.60±0.51 182.52±57.39 12.06±1.42 3.27±1.94 44.32±19.73 8.44±3.35 t值 2.888 -3.548 4.067 -4.123 -2.791 2.110 7.384 -5.633 5.687 P值 0.004 <0.001 <0.001 <0.001 0.006 0.036 <0.001 <0.001 <0.001 表 3 轻型与中重型ACI组血常规相关指标比较(x±s)
组别 例数 WBC
(×109/L)RBC
(×1012/L)NE
(×109/L)LYM
(×109/L)PLT
(×109/L)MPV
(fL)NLR PNR MPVLR 轻型ACI组 70 6.45±1.82 4.39±0.51 4.10±1.62 1.73±0.53 189.44±56.43 12.17±1.27 2.52±1.14 48.44±19.24 7.79±2.64 中重型ACI组 55 7.78±3.34 4.25±0.59 5.69±3.10 1.47±0.48 186.43±58.87 11.93±1.59 4.18±2.23 39.09±19.25 9.04±3.39 t值 2.669 -1.349 3.455 -2.832 0.675 -0.927 5.018 -2.697 2.323 P值 0.009 0.180 0.001 0.005 0.501 0.356 <0.001 0.008 0.022 表 4 ACI严重程度的多因素logistic回归分析
项目 B SE Wald χ2 P值 OR(95% CI) NLR 0.661 0.271 5.934 0.015 1.936(1.138~3.294) MPVLR -0.019 0.121 0.025 0.874 0.981(0.774~1.243) WBC -0.029 0.166 0.031 0.861 0.971(0.702~1.344) PNR 0.004 0.013 0.080 0.777 1.004(0.979~1.029) 注: 因变量ACI严重程度赋值, 轻度=0, 中重度=1;自变量WBC、NLR、PNR、MPVLR均以实际值赋值。 -
[1] 单伟. 急性脑梗死超早期溶栓的临床效果分析[J]. 当代医学, 2021, 27(6): 152-153. https://www.cnki.com.cn/Article/CJFDTOTAL-DDYI202106062.htm [2] VIDALE S, CONSOLI A, ARNABOLDI M. Postischemic Inflammation in Acute Stroke[J]. J Clin Neurol, 2017, 13(1): 1-9. doi: 10.3988/jcn.2017.13.1.1 [3] MESHAAL M S, NAGI A, ELDAMATY A, et al. Neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR) as independent predictors of outcome in infective endocarditis (IE)[J]. Egypt Heart J, 2019, 71(1): 13. doi: 10.1186/s43044-019-0014-2 [4] 刘洁香, 胡蛟龙, 李素颀, 等. 外周血中性粒细胞与淋巴细胞比值对急性胸痛患者中高危胸痛的诊断价值[J]. 中国临床医生杂志, 2021, 49(4): 442-446. doi: 10.3969/j.issn.2095-8552.2021.04.020 [5] BALTA S, CELIK T, MIKHAILIDIS D P, et al. The relation between atherosclerosis and the neutrophil-lymphocyte ratio[J]. Clin Appl Thromb Hemost, 2016, 22(5): 405-411. doi: 10.1177/1076029615569568 [6] 靳磊, 李敏, 高坡, 等. 应用血小板参数和中性粒细胞与淋巴细胞比值预测早期急性脑梗死严重程度[J]. 中华老年心脑血管病杂志, 2020, 22(6): 605-608. doi: 10.3969/j.issn.1009-0126.2020.06.012 [7] 脑梗死临床特点及诊治方法[J]. 临床误诊误治, 2020, 33(7): 2. [8] DU J, WANG Q, HE B, et al. Association of mean platelet volume and platelet count with the development and prognosis of ischemic and hemorrhagic stroke[J]. Int J Lab Hematol, 2016, 38(3): 233-239. doi: 10.1111/ijlh.12474 [9] 杨静, 史兆春, 戚志强, 等. 血小板-中性粒细胞比值与急性脑梗死患者神经功能损害及预后的相关性研究[J]. 南京医科大学学报(自然科学版), 2021, 41(3): 376-380. https://www.cnki.com.cn/Article/CJFDTOTAL-NJYK202103011.htm [10] JIN P P, LI X M, CHEN J, et al. Platelet-to-neutrophil ratio is a prognostic marker for 90-days outcome in acute ischemic stroke[J]. J Clin Neurosci, 2019(63): 110-115. http://www.onacademic.com/detail/journal_1000041590048799_4829.html [11] FARAH R, SAMRA N. Mean platelets volume and neutrophil to lymphocyte ratio as predictors of stroke[J]. J Clin Lab Anal, 2018, 32(1): e22189. doi: 10.1002/jcla.22189 [12] DÍAZ J M, BOIETTI B R, VAZQUEZ F J, et al. Mean platelet volume as a prognostic factor for venous thromboembolic disease[J]. Rev Med Chil, 2019, 147(2): 145-152. doi: 10.4067/s0034-98872019000200145 [13] XU M, HE X Y, HUANG P. The relationship between the mean platelet volume and carotid atherosclerosis and prognosis in patients with acute cerebral[J]. Biomed Res Int, 2020, 2020: 6685740. http://www.researchgate.net/publication/348158587_The_Relationship_between_the_Mean_Platelet_Volume_and_Carotid_Atherosclerosis_and_Prognosis_in_Patients_with_Acute_Cerebral_Infarction [14] CHEN S Y, LIN Y S, CHENG Y F, et al. Mean platelet volume-to-lymphocyte ratio predicts poor functional outcomes among ischemic stroke patients treated with intravenous thrombolysis[J]. Front Neurol, 2019(10): 1274. http://www.ncbi.nlm.nih.gov/pubmed/31920909 [15] 彭斌, 吴波. 中国急性缺血性脑卒中诊治指南2018[J]. 中华神经科杂志, 2018, 51(9): 666-682. https://www.cnki.com.cn/Article/CJFDTOTAL-XDJB201911024.htm [16] LALLUKKA T, ERVASTI J, LUNDSTRÖM E, et al. Trends in diagnosis-specific work disability before and after stroke: A longitudinal population-based study in Sweden[J]. J Am Heart Assoc, 2018, 7(1): e006991. http://www.onacademic.com/detail/journal_1000040474928910_b0b1.html [17] SAAND A R, YU F, CHEN J, et al. Systemic inflammation in hemorrhagic strokes-A novel neurological sign and therapeutic target?[J]. J Cereb Blood Flow Metab, 2019, 39(6): 959-988. doi: 10.1177/0271678X19841443 [18] BOZLU G, AKAR A, DURAK F, et al. Role of mean platelet volume-to-lymphocyte ratio in the diagnosis of childhood appendicitis[J]. Arch Argent Pediatr, 2019, 117(6): 375-380. http://www.ncbi.nlm.nih.gov/pubmed/31758879 [19] MING L, JIANG Z, MA J, et al. Platelet-to-lymphocyte ratio, neutrophil-to-lymphocyte ratio, and platelet indices in patients with acute deep vein thrombosis[J]. Vasa, 2018, 47(2): 143-147. doi: 10.1024/0301-1526/a000683 [20] 吴凡, 马俊芬, 平杰丹, 等. 早期平均血小板体积/淋巴细胞比值对急性脑梗死的诊断价值[J]. 郑州大学学报(医学版), 2020, 55(1): 89-92. https://www.cnki.com.cn/Article/CJFDTOTAL-HNYK202001022.htm [21] SUN Y, YOU S, ZHONG C, et al. Neutrophil to lymphocyte ratio and the hematoma volume and stroke severity in acute intracerebral hemorrhage patients[J]. Am J Emerg Med, 2017, 35(3): 429-433. doi: 10.1016/j.ajem.2016.11.037 [22] GILES J A, GREENHALGH A D, DENES A, et al. Neutrophil infiltration to the brain is platelet-dependent, and is reversed by blockade of platelet GPIbα[J]. Immunology, 2018, 154(2): 322-328. doi: 10.1111/imm.12892 [23] ZHANG N, TSE G, LIU T. Neutrophil-lymphocyte ratio in the immune checkpoint inhibitors-related atherosclerosis[J]. Eur Heart J, 2021, 42(22): 2215. http://www.researchgate.net/publication/350286848_Neutrophil-lymphocyte_ratio_in_the_immune_checkpoint_inhibitors-related_atherosclerosis [24] ADAMSTEIN N H, MACFADYEN J G, ROSE L M, et al. The neutrophil-lymphocyte ratio and incident atherosclerotic events: Analyses from five contemporary randomized trials[J]. Eur Heart J, 2021, 42(9): 896-903. -





 下载:
下载: