Efficacy analysis of early radiotherapy versus delayed radiotherapy in 68 cases of EGFR-mutant lung adenocarcinoma with brain metastases
-
摘要:
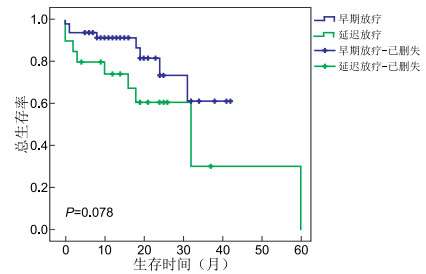
目的 探讨早期放疗与延迟放疗对EGFR突变型肺腺癌合并脑转移患者的疗效和影响因素。 方法 收集2016年1月1日—2020年12月31日就诊于蚌埠医学院第一附属医院的68例EGFR突变型肺腺癌脑转移患者的资料。根据脑放疗时机将患者分为2组,早期放疗组48例:脑部放疗同步表皮生长因子受体酪氨酸激酶抑制剂(EGFR-TKIs);延迟放疗组20例:先行EGFR-TKIs治疗,脑部病灶进展后行颅脑放疗。评估2组患者颅内无进展生存时间(iPFS)和总生存时间(OS),同时行预后影响因素分析。 结果 所有患者的中位OS为26个月。早期放疗组比延迟放疗组的iPFS有延长趋势,1年、2年、3年iPFS率分别为91.3%、73.5%、61.3%和74.3%、60.8%、30.4%(P=0.078);早期放疗组比延迟放疗组的OS也呈延长趋势,1年、2年、3年的OS率分别为81.6%、51.5%、51.5%和65.0%、51.2%、20.5%,但差异均无统计学意义(P=0.321)。多因素分析显示Lung-mol GPA评分高(2.5~4.0分)的患者OS明显优于评分低(0~2.0分)的患者(P<0.001);ECOG评分低与更好的iPFS相关(P=0.010)。 结论 EGFR突变型脑转移患者的早期颅脑放疗对比延迟放疗,iPFS和OS有延长趋势,但差异无统计学意义。ECOG评分和Lung-mol GPA评分分别为iPFS和OS的独立预后因素。 Abstract:Objective To investigate the efficacy and influencing factors of early radiotherapy versus delayed radiotherapy in EGFR-mutant lung adenocarcinoma patients with brain metastasis. Methods A total of 68 cases of EGFR-mutant lung adenocarcinoma patients with brain metastases, who were admitted in the First Affiliated Hospital of Bengbu Medical College from January 1, 2016 to December 31, 2020. The patients were divided into two groups according to the timing of brain radiotherapy. The early radiotherapy group (n=48) received brain radiotherapy and epidermal growth factor receptor tyrosine kinase inhibitor (EGFR-TKI) simultaneously. In the delayed radiotherapy group (n=20), EGFR-TKI was performed initially, and brain radiotherapy was performed after the brain lesions progressed. Intracranial progression-free survival (iPFS) and overall survival (OS) of the two groups were evaluated, and prognostic factors were analysed. Results The median OS of all patients was 26 months. The iPFS of the early radiotherapy group was prolonged compared with the delayed group. The 1-year, 2-year and 3-year iPFS rates were 91.3%, 73.5%, 61.3% and 74.3%, 60.8%, 30.4%, respectively (P=0.078). The OS of the early radiotherapy group was also longer than that of the delayed radiotherapy group. The OS rates were 81.6%, 51.5%, 51.5% and 65.0%, 51.2%, 20.5%, respectively, with no significant difference (P=0.321). The OS of patients with high Lung-mol GPA score was better than the OS of patients with low score (P < 0.001). Low ECOG score indicated good iPFS (P=0.010). Conclusion Compared with delayed radiotherapy, early radiotherapy may prolong iPFS and OS, but no significant statistical difference is found. ECOG and Lung-mol GPA are independent prognostic factors of iPFS and OS, respectively. -
表 1 68例EGFR突变型肺腺癌脑转移患者的临床特征比较(例)
组别 例数 性别 年龄(岁) ECOG评分(分) 脑转移数目(个) 初诊脑转移 颅内症状 颅外转移 Lung-mol GPA(分) 放疗类型 男性 女性 <60 ≥60 0~1 2~3 1~3 >3 无 有 无 有 无 有 0~2.0 2.5~4.0 全脑 局部 全脑+局部 早期放疗 48 18 30 24 24 34 14 19 29 7 41 13 35 32 16 12 36 22 9 17 延迟放疗 20 3 17 9 11 12 8 11 9 3 17 10 10 9 11 4 16 7 9 4 χ2值 3.299 0.141 0.757 1.361 0.109 3.312 2.768 0.017 5.150 P值 0.069 0.707 0.384 0.243 0.740 0.069 0.096 0.897 0.076 表 2 68例EGFR突变型肺腺癌脑转移患者预后单因素分析(%)
项目 例数 iPFS χ2值 P值 OS χ2值 P值 1年 2年 3年 1年 2年 3年 性别 0.244 0.621 0.462 0.496 男性 21 88.9 77.8 38.9 78.9 42.2 21.1 女性 47 84.9 67.3 50.5 74.8 56.6 43.6 年龄(岁) 0.080 0.778 0.021 0.884 <60 24 86.8 74.2 55.7 78.9 48.4 38.7 ≥60 24 85.3 67.7 45.2 73.6 53.8 35.9 ECOG评分 6.703 0.010 0.777 0.378 0~1 34 95.3 79.6 53.0 81.4 58.4 37.9 2~3 14 67.1 52.9 52.9 66.1 40.1 40.1 脑转移数目 0.007 0.935 0.860 0.354 1~3 19 86.4 75.6 47.3 78.7 63.2 37.9 >3 29 85.6 61.7 61.7 74.2 42.8 34.2 初诊脑转移 0.207 0.649 3.361 0.067 无 7 100.0 75.0 50.0 90.0 78.8 59.1 有 41 83.6 70.0 50.0 73.5 46.0 32.7 颅内症状 0.312 0.576 5.269 0.022 无 13 91.3 69.6 23.2 63.6 36.3 13.6 有 35 83.7 70.3 60.2 82.7 60.7 52.0 颅外转移 0.009 0.923 1.024 0.312 无 32 87.0 70.0 42.0 81.2 56.1 42.1 有 16 85.2 69.7 55.8 68.4 46.9 31.3 Lung-mol GPA(分) 1.531 0.216 15.855 <0.001 0~2.0 12 69.6 69.6 69.6 55.6 0.0 0.0 2.5~4.0 36 90.2 72.2 50.6 86.2 63.3 45.5 放疗类型 3.846 0.146 0.585 0.747 全脑 22 84.6 53.6 53.6 77.6 40.5 27.0 局部 9 77.8 69.1 34.6 69.6 61.8 37.1 全脑+局部 17 95.2 84.7 84.7 79.5 54.4 54.4 脑放疗时机 3.104 0.078 0.986 0.321 早期放疗 48 91.3 73.5 61.3 81.6 51.5 51.5 延迟放疗 20 74.3 60.8 30.4 65.0 51.2 20.5 -
[1] SONG Y, WU Y L, CAO L J, et al. Efficacy and safety of gefitinib as third line treatment in NSCLC patients with activating EGFR mutations treated with first-line gefitinib followed by second-line chemotherapy: A single-arm, prospective, multicenter phase Ⅱ study (RECHALLENGE, CTONG1304)[J]. Am J Clin Oncol, 2019, 42(5): 432-439. doi: 10.1097/COC.0000000000000538 [2] RAMALINGAM S S, VANSTEENKISTE J, PLANCHARD D, et al. Overall survival with osimertinib in untreated, EGFR-mutated advanced NSCLC[J]. N Engl J Med, 2020, 382(1): 41-50. doi: 10.1056/NEJMoa1913662 [3] BROWN P D, JAECKLE K, BALLMAN K V, et al. Effect of radiosurgery alone vs radiosurgery with whole brain radiation therapy on cognitive function in patients with 1 to 3 brain metastases: A randomized clinical trial[J]. JAMA, 2016, 316(4): 401-409. doi: 10.1001/jama.2016.9839 [4] ACHROL A S, RENNERT R C, ANDERS C, et al. Brain metastases[J]. Nat Rev Dis Primers, 2019, 5(1): 5. doi: 10.1038/s41572-018-0055-y [5] SPERDUTO P W, YANG T J, BEAL K, et al. Estimating survival in patients with lung cancer and brain metastases: An update of the graded prognostic assessment for lung cancer using molecular markers (Lung-molGPA)[J]. JAMA Oncol, 2017, 3(6): 827-831. doi: 10.1001/jamaoncol.2016.3834 [6] ZHU Q, SUN Y, CUI Y, et al. Clinical outcome of tyrosine kinase inhibitors alone or combined with radiotherapy for brain metastases from epidermal growth factor receptor (EGFR) mutant non small cell lung cancer (NSCLC)[J]. Oncotarget, 2017, 8(8): 13304-13311. doi: 10.18632/oncotarget.14515 [7] CHEN Y, WEI J, CAI J, et al. Combination therapy of brain radiotherapy and EGFR-TKIs is more effective than TKIs alone for EGFR-mutant lung adenocarcinoma patients with asymptomatic brain metastasis[J]. BMC Cancer, 2019, 19(1): 793. doi: 10.1186/s12885-019-6005-6 [8] MAGNUSON W J, LESTER-COLL N H, WU A J, et al. Management of brain metastases in tyrosine kinase inhibitor-naive epidermal growth factor receptor mutant non-small cell lung cancer: A retrospective multi-institutional analysis[J]. J Clin Oncol, 2017, 35(1): 1070-1077. [9] YU X, FAN Y. Real-World data on prognostic factors for overall survival in EGFR-Mutant Non-Small-Cell lung cancer patients with brain metastases[J]. J Cancer, 2019, 10(15): 3486-3493. doi: 10.7150/jca.30292 [10] LI C, GUO J, ZHAO L, et al. Upfront whole brain radiotherapy for multiple brain metastases in patients with EGFR-mutant lung adenocarcinoma[J]. Cancer Manag Res, 2019, 11: 3433-3443. doi: 10.2147/CMAR.S196881 [11] BYEON S, HAM J S, SUN J M, et al. Analysis of the benefit of sequential cranial radiotherapy in patients with EGFR mutant non-small cell lung cancer and brain metastasis[J]. Med Oncol, 2016, 33(8): 97. doi: 10.1007/s12032-016-0811-3 [12] 蒋一玲, 张传领, 陈承, 等. 贝伐珠单抗联合靶向治疗对EGFR突变型非小细胞肺癌患者的疗效观察[J]. 中华全科医学, 2021, 19(8): 1306-1309. https://www.cnki.com.cn/Article/CJFDTOTAL-SYQY202108015.htm [13] JABLONSKA P A, BOSCH-BARRERA J, SERRANO D, et al. Challenges and novel opportunities of radiation therapy for brain metastases in non-small cell lung cancer[J]. Cancers (Basel), 2021, 13(9): 2141. doi: 10.3390/cancers13092141 [14] SPERDUTO P W, YANG T J, BEAL K, et al. The effect of gene alterations and tyrosine kinase inhibition on survival and cause of death in patients with adenocarcinoma of the lung and brain metastases[J]. Int J Radiat Oncol Biol Phys, 2016, 96(2): 406-413. doi: 10.1016/j.ijrobp.2016.06.006 [15] WU Y L, AHN M J, GARASSINO M C, et al. CNS efficacy of osimertinib in patients with T790M-Positive advanced non-small-cell lung cancer: Data From a randomized phase Ⅲ trial (AURA3)[J]. J Clin Oncol, 2018, 36(26): 2702-2709. doi: 10.1200/JCO.2018.77.9363 -





 下载:
下载: