Construction of survival and prognosis nomogram for elderly nasopharyngeal carcinoma (≥ 60 years) based on SEER Database
-
摘要:
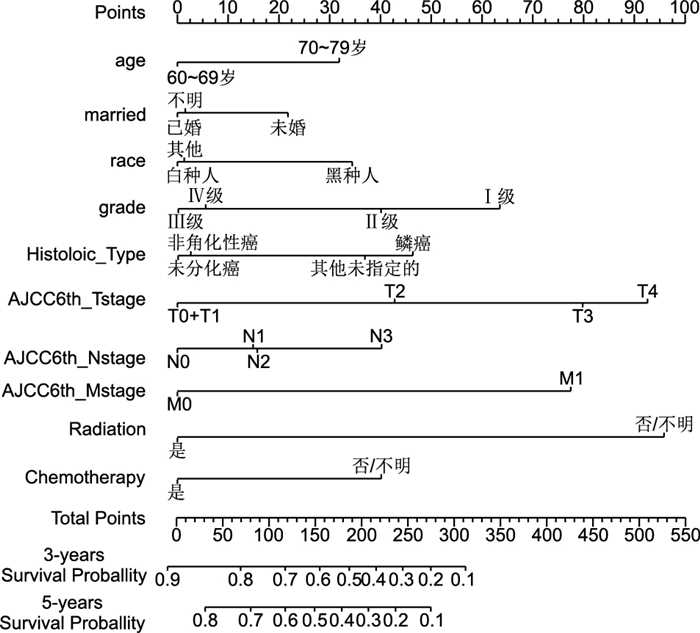
目的 利用美国流行病学监测和结果(surveillance, epidemiology, and end results,SEER)数据库构建老年鼻咽癌患者(≥60岁)生存预后风险预测列线图,预测老年鼻咽癌患者的总生存率,为临床决策提供科学依据。 方法 从数据库中提取2004—2015年期间的老年鼻咽癌患者共1 366例,随机分为建模组和验证组。对建模组采用Cox比例风险回归模型分析患者的预后影响因素,再构建列线图。利用一致性指数(C-index)和校正曲线对列线图进行验证,评估其预测价值。 结果 建模组的Cox比例风险回归模型结果表明:年龄、婚姻、种族、肿瘤分化等级、组织学类型、TNM分期及放化疗均是老年鼻咽癌患者的预后影响因素(均P<0.05),均被用于构建风险预测列线图。风险预测列线图的验证结果表明,建模组的C指数为0.732(95% CI为0.708~0.756),验证组为0.762(95% CI为0.729~0.795);2组的校正曲线均表现出良好的一致性。 结论 本研究构建的老年鼻咽癌患者生存预后的风险预测列线图具有良好的预测价值,可快速准确对患者进行个体化的生存预后评估;有远处转移的80岁以上鼻咽癌患者或许是预立医疗照护计划的切入点。 -
关键词:
- 老年 /
- 鼻咽癌 /
- 监测、流行病学和结果数据库 /
- 生存分析 /
- 风险预测列线图
Abstract:Objective To establish a nomogram to predict the overall survival (OS) rate of elderly patients with nasopharyngeal carcinoma (≥ 60 years) by utilising the database of the Surveillance, Epidemiology and End Results (SEER) program. Methods The data of 1 366 elderly patients with nasopharyngeal carcinoma who were diagnosed between 2004 and 2015 from the SEER database were obtained. These patients were randomly divided into training (n=954) and validation (n=412) cohorts. The Cox Proportional hazards regression model was performed to evaluate the prognostic effects of multiple clinicopathologic factors on OS. Significant prognostic factors were combined to build a nomogram. The predictive performance of the nomogram was evaluated via internal (training cohort data) and external validation (validation cohort data) by calculating the index of concordance (C-index) and plotting calibration curves. Results In the training cohort, the results of Cox proportional hazards regression model showed that age at diagnosis, married status, race, grade, histologic type, TNM stage, radiation and chemotherapy were significantly associated with the survival prognosis (P < 0.05). These factors were used to establish the nomogram. The nomogram showed good accuracy in predicting OS rate, with a C-index of 0.732 (95% CI: 0.708-0.756) in internal validation and a C-index of 0.762(95% CI was 0.729-0.795) in external validation. All calibration curves showed excellent consistency between prediction by nomogram and actual observation. Conclusion A novel nomogram for elderly patients with nasopharyngeal carcinoma is established to predict OS in our study and shows good prognostic significance. It can provide medical personnel with accurate and practical predictive tools which can quickly and accurately assess the survival prognosis of patients individually and guide medical personnel in the follow-up treatment of patients. -
表 1 建模组生存分析变量赋值表
Table 1. Variable assignment table of overall survival analysis in training cohort
变量 赋值方法 年龄 60~69岁=1,70~79岁=2,≥80岁=3 性别 女=1,男=2 婚姻状况 已婚=1,未婚=2,不明=3 种族 黑种人=1,白种人=2,其他人种=3 肿瘤分化等级 高分化(Ⅰ级)=1,中分化(Ⅱ级)=2,低分化(Ⅲ级)=3,未分化(Ⅳ级)=4 组织学类型 鳞癌=1,非角化性癌=2,未分化癌=3,其他未指定的=4 T分期 T0+T1期=1,T2期=2,T3期=3,T4期=4 N分期 N0期=1,N1期=2,N2期=3,N3期=4 M分期 M0期=1,M1期=2 是否放疗 是=1,否/不明=2 是否化疗 是=1,否/不明=2 表 2 建模组和验证组患者的临床基本特征比较[例(%)]
Table 2. Comparison of clinicial basic characteristics between training cohort and validation cohort [cases (%)]
临床基本特征 建模组(n=954) 验证组(n=412) χ2值 P值 年龄(岁) 60~69 546(57.2) 249(60.4) 3.001 0.223 70~79 290(30.4) 125(30.3) ≥80 118(12.4) 38(9.2) 性别 女性 263(27.6) 116(28.2) 0.049 0.824 男性 691(72.4) 296(71.8) 婚姻状态 已婚 595(62.4) 254(61.7) 0.219 0.896 未婚a 307(32.2) 133(32.3) 不明 52(5.5) 25(6.1) 种族 黑种人 91(9.5) 38(9.2) 1.220 0.543 白种人 542(56.8) 247(60.0) 其他人种b 321(33.6) 127(30.8) 肿瘤分化等级 高分化(Ⅰ级) 46(4.8) 15(3.6) 2.267 0.519 中分化(Ⅱ级) 185(19.4) 77(18.7) 低分化(Ⅲ级) 439(46.0) 183(44.4) 未分化(Ⅳ级) 284(29.8) 137(33.3) 组织学类型 鳞状细胞癌 448(47.0) 199(48.3) 1.640 0.650 非角化性癌 203(21.3) 77(18.7) 未分化癌 150(15.7) 72(17.5) 其他未指定的 153(16.0) 64(15.5) T分期 T0+T1 303(31.8) 127(30.8) 1.525 0.677 T2 234(24.5) 101(24.5) T3 212(22.2) 84(20.4) T4 205(21.5) 100(24.3) N分期 N0 351(36.8) 137(33.3) 2.698 0.440 N1 307(32.2) 138(33.5) N2 209(21.9) 90(21.8) N3 87(9.1) 47(11.4) M分期 M0 860(90.1) 372(90.3) 0.007 0.934 M1 94(9.9) 40(9.7) 放射治疗 是 791(82.9) 339(82.3) 0.081 0.777 否/不明 163(17.1) 73(17.7) 化学治疗 是 708(74.2) 300(72.8) 0.291 0.590 否/不明 246(25.8) 112(27.2) 注:a未婚包含单身、分居、离婚和丧偶[12]。b其他人种包括亚洲人、印第安人、阿拉斯加原住民及太平洋岛民。 表 3 单因素生存分析结果
Table 3. Univariate analysis of overall survival
临床病理学特征 中位生存时间(月) 1年生存率 3年生存率 5年生存率 χ2值 P值 年龄(岁) 60~69 67 0.809 0.623 0.526 104.732 <0.001 70~79 43 0.719 0.526 0.410 ≥80 11 0.462 0.243 0.158 性别 女 53 0.733 0.575 0.448 0.033 0.856 男 47 0.739 0.536 0.447 婚姻状态 已婚 60 0.776 0.586 0.496 20.683 <0.001 未婚 28 0.660 0.453 0.344 不明 104 0.788 0.631 0.512 种族 黑种人 29 0.670 0.420 0.274 11.628 0.003 白种人 41 0.708 0.530 0.440 其他 62 0.812 0.606 0.507 肿瘤分化等级 高分化(Ⅰ级) 19 0.536 0.340 0.203 51.029 <0.001 中分化(Ⅱ级) 20 0.589 0.397 0.315 低分化(Ⅲ级) 53 0.760 0.564 0.464 未分化(Ⅳ级) 71 0.845 0.652 0.536 组织学类型 鳞状细胞癌 28 0.650 0.453 0.352 32.358 <0.001 非角化性癌 68 0.838 0.649 0.542 未分化癌 71 0.826 0.650 0.549 其他未指定的 59 0.769 0.569 0.492 T分期 T0+T1 83 0.844 0.674 0.572 55.718 <0.001 T2 56 0.748 0.582 0.483 T3 29 0.691 0.452 0.349 T4 22 0.623 0.415 0.321 N分期 N0 35 0.688 0.495 0.394 9.707 0.021 N1 65 0.778 0.602 0.523 N2 53 0.789 0.588 0.457 N3 28 0.690 0.461 0.372 M分期 M0 56 0.766 0.582 0.481 70.005 <0.001 M1 12 0.496 0.217 0.125 放射治疗 是 61 0.804 0.616 0.506 157.575 <0.001 否/不明 8 0.424 0.201 0.156 化学治疗 是 59 0.796 0.602 0.495 41.132 <0.001 否/不明 19 0.576 0.387 0.310 表 4 多因素Cox比例风险回归分析结果
Table 4. Multivariate Cox regression analysis of overall survival
项目 B SE Wald χ2 P值 RR值 95% CI 年龄(60~69岁) 70~79岁 0.308 0.101 9.280 0.002 1.361 1.116~1.659 ≥80岁 0.967 0.129 56.304 <0.001 2.630 2.043~3.385 性别(女) 男 0.183 0.102 3.215 0.073 1.201 0.983~1.467 婚姻状态(已婚) 未婚 0.247 0.095 6.752 0.009 1.280 1.062~1.541 不明 0.054 0.220 0.060 0.806 1.056 0.686~1.625 种族(黑种人) 白种人 -0.287 0.144 3.995 0.046 0.751 0.566~0.994 其他人种 -0.289 0.156 3.424 0.064 0.749 0.552~1.017 肿瘤分化等级(高分化, Ⅰ级) 中分化(Ⅱ级) -0.207 0.194 1.136 0.287 0.813 0.556~1.190 低分化(Ⅲ级) -0.596 0.187 10.147 0.001 0.551 0.382~0.795 未分化(Ⅳ级) -0.527 0.223 5.587 0.018 0.590 0.381~0.914 组织学类型(鳞癌) 非角化性癌 -0.416 0.127 10.817 0.001 0.660 0.515~0.845 未分化癌 -0.444 0.194 5.242 0.022 0.641 0.438~0.938 其他未指定的 -0.090 0.143 0.392 0.531 0.914 0.690~1.211 T分期(T0+T1) T2 0.404 0.127 10.189 0.001 1.498 1.169~1.919 T3 0.742 0.124 35.813 <0.001 2.100 1.647~2.678 T4 0.874 0.125 48.927 <0.001 2.396 1.876~3.061 N分期(N0) N1 0.131 0.111 1.395 0.238 1.140 0.917~1.418 N2 0.142 0.120 1.405 0.236 1.153 0.911~1.458 N3 0.351 0.160 4.813 0.028 1.421 1.038~1.945 M分期(M0) M1 0.707 0.132 28.683 <0.001 2.027 1.565~2.625 是否放疗(是) 否/不明 0.909 0.116 61.512 <0.001 2.482 1.978~3.116 是否化疗(是) 否/不明 0.348 0.112 9.616 0.002 1.416 1.137~1.764 注:括号内为对照组。 -
[1] 梁锌, 杨剑, 高婷, 等. 中国鼻咽癌流行概况[J]. 中国肿瘤, 2016, 25(11): 835-840. doi: 10.11735/j.issn.1004-0242.2016.11.A001LIANG Z, YANG J, GAO T, et al. Nasopharynx Cancer Epidemiology in China[J]. China Cancer, 2016, 25(11): 835-840. doi: 10.11735/j.issn.1004-0242.2016.11.A001 [2] 中国抗癌协会, 中国抗癌协会肿瘤营养与支持治疗专业委员会, 中国抗癌协会癌症康复与姑息治疗专业委员会, 等. 鼻咽癌营养治疗专家共识[J]. 肿瘤代谢与营养电子杂志, 2018, 5(1): 30-32. https://www.cnki.com.cn/Article/CJFDTOTAL-ZLDX201801008.htmCHINESE ANTI-CANCER ASSOCIATION, CHINESE SOCIETY FOR ONCOLOGICAL NUTRITION AND STUPPORTIVE CARE, THE COMITTEE OF REHABILITATION AND PLLIATIVE CARE, et al. Expert consensus on nutritional therapy for patients with nasopharyngeal carcer[J]. Electron J Metab Nutr Cancer, 2018, 5(1): 30-32. https://www.cnki.com.cn/Article/CJFDTOTAL-ZLDX201801008.htm [3] BRUGEL L, LAURENT M, CAILLET P, et al. Impact of comprehensive geriatric assessment on survival, function, and nutritional status in elderly patients with head and neck cancer: Protocol for a multicentre randomised controlled trial(EGeSOR)[J]. BMC Cancer, 2014, 14: 427. doi: 10.1186/1471-2407-14-427 [4] 曾奇, 郭翔, 李宁炜, 等. 313例老年鼻咽癌患者临床特征及预后的回顾性研究[J]. 癌症, 2008(3): 289-294. doi: 10.3321/j.issn:1000-467X.2008.03.012ZENG Q, GUO X, LI N W, et al. Clinical characteristics and prognosis of aged nasopharyngeal carcinoma patients: A report of 313 cases[J]. Chinese Journal of Cancer, 2008(3): 289-294. doi: 10.3321/j.issn:1000-467X.2008.03.012 [5] 张银. 135例鼻咽癌患者根治性放疗疗效及预后因素分析[D]. 长春: 吉林大学, 2018.ZHANG Y. Analysis of responses and prognostic factors in radical radiotherapy for 135 patients with nasopharyngeal carcinoma[D]. Changchun: Jilin University, 2018. [6] 陆颖. 基于调强放射治疗的鼻咽癌生存预后因素分析[D]. 南宁: 广西医科大学, 2018.LU Y. Discuss on survival and prognosis factors of nasopharyngeal carcinoma based on intensity-modulated radiation therapy[D]. Nanning: Guangxi Medical University, 2018. [7] 左倩倩, 张彦兵, 马婕群, 等. 胃神经内分泌瘤患者预后Nomogram预测模型的构建[J]. 中国肿瘤生物治疗杂志, 2019, 26(5): 569-576. https://www.cnki.com.cn/Article/CJFDTOTAL-ZLSW201905014.htmZUO Q Q, ZHANG Y B, MA J Q, et al. Construction of Nomogram prediction model for prognosis of gastric neuroendocrine neoplasms[J]. Chin J Cancer Biother, 2019, 26(5): 569-576. https://www.cnki.com.cn/Article/CJFDTOTAL-ZLSW201905014.htm [8] 王亚巍. 老年结直肠癌患者(≥60岁)术后肿瘤相关死亡预测模型的构建与临床应用研究[D]. 扬州: 扬州大学, 2019.WANG Y W. Construction and application of tumor-related death prediction model in elderly patients with colorectal cancer (≥60 years old) after surgery[D]. Yangzhou: Yangzhou University, 2019. [9] 田景媛, 李孔玲, 陈罗军, 等. 胰腺导管腺癌术后患者Nomogram预后模型的构建[J]. 现代肿瘤医学, 2019, 27(9): 1571-1575. doi: 10.3969/j.issn.1672-4992.2019.09.025TIAN J Y, LI K L, CHEN L J, et al. The establishment of a prognostic Nomogram for resected pancreatic ductal adenocarcinoma[J]. Modern Oncology, 2019, 27(9): 1571-1575. doi: 10.3969/j.issn.1672-4992.2019.09.025 [10] SONG W, LV C G, MIAO D L, et al. Development and validation of a nomogram for predicting survival in patients with gastrointestinal stromal tumours[J]. Eur J Surg Oncol, 2018, 44(10): 1657-1665. doi: 10.1016/j.ejso.2018.07.004 [11] 章鸣嬛, 陈瑛, 汪城, 等. 美国国立癌症研究所SEER数据库概述及应用[J]. 微型电脑应用, 2015, 31(12): 26-28, 32. doi: 10.3969/j.issn.1007-757X.2015.12.010HANG M H, CHEN Y, WANG C, et al. Application and Summary of SEER of American National Cancer Institute[J]. Microcomputer Applications, 2015, 31(12): 26-28, 32. doi: 10.3969/j.issn.1007-757X.2015.12.010 [12] XU C, LIU X, CHEN Y P, et al. Impact of marital status at diagnosis on survival and its change over time between 1973 and 2012 in patients with nasopharyngeal carcinoma: A propensity score-matched analysis[J]. Cancer Med, 2017, 6(12): 3040-3051. doi: 10.1002/cam4.1232 [13] 蒋艳明. 鼻咽癌预后模型的建立及验证[D]. 南宁: 广西医科大学, 2018.JIANG Y M. Establishment and verification of prognosis model for nasopharyngeal cercinoma[J]. Nanning: Guangxi Medical University, 2018. [14] TANG L Q, LI C F, LI J, et al. Establishment and validation of prognostic nomograms for endemic nasopharyngeal carcinoma[J]. J Natl Cancer Inst, 2015, 108(1): djv291. DOI: 10.1093/jnci/djv291. [15] ZENG L, GUO P, LI J G, et al. Prognostic score models for survival of naso-pharyngeal carcinoma patients treated with intensity-modulated radiotherapy and chemotherapy[J]. Oncotarget, 2015, 6(36): 39373-39383. doi: 10.18632/oncotarget.5781 [16] YEH C N, WANG S Y, CHEN Y Y, et al. A prognostic nomogram for overall survival of patients after hepatectomy for intrahepatic cholangiocarcinoma[J]. Anticancer Res, 2016, 36(8): 4249-4258. [17] 刘鹏弟, 张亚飞, 陆宏伟, 等. 利用SEER数据库进行胃腺癌患者生存预后Nomogram图的构建[J]. 中国普外基础与临床杂志, 2018, 25(10): 1183-1189. https://www.cnki.com.cn/Article/CJFDTOTAL-ZPWL201810007.htmLIU P D, ZHANG Y F, LU H W, et al. Prognostic nomogram for gastric adenocarcinoma: A SEER database-based study[J]. Chinese Journal of Bases and Clinics in General Surgery, 2018, 25(10): 1183-1189. https://www.cnki.com.cn/Article/CJFDTOTAL-ZPWL201810007.htm [18] EIL R, DIGGS B S, WANG S J, et al. Nomogram for predicting the benefit of neoadjuvant chemoradiotherapy for patients with esophageal cancer: A SEER-Medicare analysis[J]. Cancer, 2014, 120(4): 492-498. doi: 10.1002/cncr.28447 [19] SHEN W, SAKAMOTO N, YANG L. Model to predict cause-specific mortality in patients with head and neck adenoid cystic carcinoma: A competing risk analysis[J]. Ann Surg Oncol, 2017, 24(8): 2129-2136. doi: 10.1245/s10434-017-5861-z [20] SONG K, SHI X, WANG H, et al. Can a Nomogram help to predict the overall and cancer-specific survival of patients with chondrosarcoma?[J]. Clin Orthop Relat Res, 2018, 476(5): 987-996. doi: 10.1007/s11999.0000000000000152 [21] FANG C, WANG W, FENG X, et al. Nomogram individually predicts the overall survival of patients with gastroenteropancreatic neuroendocrine neoplasms[J]. Br J Cancer, 2017, 117(10): 1544-1550. doi: 10.1038/bjc.2017.315 [22] CAO L L, LU J, LIN J X, et al. Incidence and survival trends for gastric neuroendocrine neoplasms: An analysis of 3523 patients in the SEER database[J]. Eur J Surg Oncol, 2018, 44(10): 1628-1633. doi: 10.1016/j.ejso.2018.01.082 [23] 陈贤明, 黄少华, 杨帆, 等. 影响鼻咽癌预后的相关因素分析[J]. 东南国防医药, 2014, 16(6): 584-586, 604. doi: 10.3969/j.issn.1672-271X.2014.06.008CHEN X M, HUANG S H, YANG F, et al. Analysis of factors related to the NPC patientsᶉprognosis[J]. Military Medical Journal of Southeast China, 2014, 16(6): 584-586, 604. doi: 10.3969/j.issn.1672-271X.2014.06.008 [24] WU S G, LIAO X L, HE Z Y, et al. Demographic and clinicopathological characteristics of nasopharyngeal carcinoma and survival outcomes according to age at diagnosis: A population-based analysis[J]. Oral Oncol, 2017, 73: 83-87. doi: 10.1016/j.oraloncology.2017.08.006 [25] 张倩, 曹乾. 婚姻状态对肺癌患者生存预后的影响: 基于SEER数据库的研究[J]. 肿瘤防治研究, 2019, 46(7): 617-621. doi: 10.3971/j.issn.1000-8578.2019.18.1425ZHANG Q, CAO Q. Effect of marital status on survival of lung cancer patients investigated based on SEER database[J]. Cancer Research on Prevention and Treatment, 2019, 46(7): 617-621. doi: 10.3971/j.issn.1000-8578.2019.18.1425 [26] WANG X, CAO W, ZHENG C, et al. Marital status and survival in patients with rectal cancer: An analysis of the Surveillance, Epidemiology and End Results(SEER) database[J]. Cancer Epidemiol, 2018, 54: 119-124. doi: 10.1016/j.canep.2018.04.007 [27] ZHOU H, ZHANG Y, SONG Y, et al. Marital status is an independent prognostic factor for pancreatic neuroendocrine tumors patients: An analysis of the Surveillance, Epidemiology, and End Results (SEER) database[J]. Clin Res Hepatol Gastroenterol, 2017, 41(4): 476-486. doi: 10.1016/j.clinre.2017.02.008 [28] HUANG S J, TANG Y Y, LIU H M, et al. Impact of age on survival of locoregional nasopharyngeal carcinoma: An analysis of the surveillance, epidemiology, and end results program database, 2004-2013[J]. Clin Otolaryngol, 2018, 43(5): 1209-1218. doi: 10.1111/coa.13124 [29] HU J, KONG L, GAO J, et al. Use of radiation therapy in metastatic nasopharyngeal cancer improves survival: A SEER analysis[J]. Sci Rep, 2017, 7(1): 721. [30] GUO R, WU H, WANG J, et al. Lymph node status and outcomes for nasopharyngeal carcinoma according to histological subtypes: A SEER population-based retrospective analysis[J]. Adv Ther, 2019, 36(11): 3123-3133. doi: 10.1007/s12325-019-01100-7 [31] 张文东. 鼻咽癌远期生存的影响因素研究[D]. 济南: 山东大学, 2014.ZHANG W D. Study on the influence factors of long-term survival of nasopharyngeal carcinoma[D]. Jinan: Shandong University, 2014. [32] 邓仁丽, 王守碧, 张江辉, 等. 中西文化视野下预立医疗照护计划在医疗卫生体系中的植入[J]. 中国护理管理, 2019, 19(3): 321-325. https://www.cnki.com.cn/Article/CJFDTOTAL-GLHL201903007.htmDENG R L, WANG S B, ZHANG J H, et al. To embed advance care planning into the health care system in China in the vision of Chinese and western culture[J]. Chinese Nursing Management, 2019, 19(3): 321-325. https://www.cnki.com.cn/Article/CJFDTOTAL-GLHL201903007.htm -





 下载:
下载: