Predictive effect of HPV typing, SCC-Ag and NLR on lymph node metastasis of early cervical cancer
-
摘要:
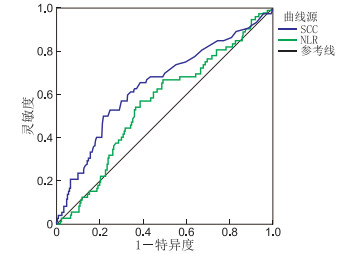
目的 探讨鳞状细胞癌抗原(SCC-Ag)、中性粒细胞与淋巴细胞比值(NLR)与早期宫颈鳞癌患者临床病理特征的相关性, 以及人乳头瘤病毒(HPV)分型、SCC-Ag、NLR联合对早期宫颈癌淋巴结转移的预测作用。 方法 选取2018年1月-2020年10月于蚌埠医学院第一附属医院术前常规行血清SCC-Ag及血常规检测的ⅠA2~ⅡA期宫颈鳞癌患者共302例, 其中明确HPV分型的共194例。对明确HPV分型的宫颈癌与淋巴结转移进行相关性分析, 对NLR及SCC-Ag与临床病理特征的相关性进行单因素及多因素分析; 绘制ROC曲线, 确定NLR及SCC-Ag对早期宫颈鳞癌淋巴结转移的最佳截断值, 以及联合诊断对早期宫颈癌淋巴结转移的预测作用。 结果 194例确定HPV分型的患者中, HPV16阳性对淋巴结转移的灵敏度为52.94%, 特异度为27.50%。多因素分析结果显示, 肿瘤大小、肌层浸润深度、淋巴结转移状况是SCC-Ag滴度>2.0 ng/mL的独立影响因素, 淋巴结转移是NLR>1.753的独立危险因素。ROC曲线显示最佳截断值SCC为4.15 ng/mL、NLR为1.900, 联合诊断与临床病理诊断之间, 在检出阳性率上差异无统计学意义(χ2=0.03, P=0.869)。联合诊断时特异度为81.00%, 阳性似然比为45.71%, 阴性似然比为81.82%, 诊断效能相对较高。 结论 联合诊断对早期宫颈癌转移有一定的预测价值。 -
关键词:
- 人乳头瘤病毒分型 /
- 鳞状细胞癌抗原 /
- 中性粒细胞与淋巴细胞比值 /
- 宫颈癌 /
- 淋巴结转移
Abstract:Objective To investigate the correlation between squamous cell carcinoma antigen (SCC-Ag), neutrophil to lymphocyte ratio (NLR) and clinicopathological characteristics of patients with early cervical squamous cell carcinoma, and discuss the predictive effect of HPV typing, SCC-Ag and NLR on lymph node metastasis of early cervical carcinoma. Methods A total of 302 patients with stageⅠA2-ⅡA cervical squamous cell carcinoma with serum SCC-Ag and routine blood tests before treatment in the First Affiliated Hospital of Bengbu Medical College from January 2018 to October 2020 were selected. Among them, 194 cases were identified with HPV type. The correlation between cervical cancer with HPV type and lymph node metastasis was analyzed. Univariate and multivariate analyses of the association between NLR and SCC-Ag and clinicopathological outcomes were performed in combination with patient-related cases. The ROC curve was drawn to determine the optimal truncation value of NLR and SCC-Ag for lymph node metastasis of early cervical squamous cell carcinoma, as well as the predictive effect of combined diagnosis on lymph node metastasis of early cervical carcinoma. Results Among 194 patients with HPV typing, the sensitivity and specificity of HPV16 positive for lymph node metastasis were 52.94% and 27.50%, respectively. Multivariate analysis showed that tumor size, invasion depth and lymph node metastasis were independent risk factors for SCC Ag titer>2.0 ng/mL, and lymph node metastasis was independent risk factor for NLR>1.753. ROC curve showed that the optimal cut-off value of SCC and NLR were 4.15 ng/mL and 1.900, respectively. There was no significant difference in positive rate between combined diagnosis and clinicopathological diagnosis (χ2=0.030, P=0.869). The specificity, positive likelihood ratio and negative likelihood ratio for combined diagnosis were 81.00%, 45.71% and 81.82%, respectively, which were relatively high. Conclusion Combined diagnosis has certain predictive value for early cervical cancer metastasis. -
表 1 治疗前SCC-Ag及NLR与临床病理特征的单因素分析(例)
Table 1. Univariate analysis of SCC-Ag, NLR and clinicopathological characteristics before treatment (cases)
因素 例数 SCC-Ag χ2值 P值 NLR χ2值 P值 ≤2.0 ng/mL >2.0 ng/mL ≤1.753 >1.753 FIGO分期 18.334 <0.001 4.636 0.098 ⅠA期 11 9 2 9 2 ⅠB期 204 117 87 100 104 ⅡA期 87 29 58 42 45 肿瘤大小(cm) 37.020 <0.001 1.613 0.204 <4 163 110 53 87 76 ≥4 139 45 94 64 75 临床分级 0.423 0.809 0.227 0.893 Ⅰ~Ⅱ 21 12 9 11 10 Ⅱ 184 95 89 90 94 Ⅱ~Ⅲ 97 48 49 50 47 年龄(岁) 0.448 0.485 0.277 0.599 ≤40 37 17 20 17 20 >40 265 138 127 134 131 肌层浸润深度 47.628 <0.001 5.025 0.025 <1/2 94 76 18 56 38 >1/2 208 79 129 95 113 盆腔淋巴结转移 14.213 <0.001 4.669 0.031 有 72 23 49 28 44 无 340 132 98 123 107 脉管浸润 4.862 0.027 2.855 0.091 无 251 136 115 131 120 有 51 19 32 20 31 生长方式 18.000 <0.001 1.295 0.523 外生型 58 31 27 27 31 内生型 208 94 114 103 105 其他型 36 30 6 21 15 表 2 临床病理特征与术前SCC-Ag水平的多因素分析
Table 2. Multivariate analysis of clinicopathological features and preoperative SCC-Ag levels
变量 B SE Wald χ2 P值 OR值 95% CI 年龄 -0.489 0.441 1.226 0.268 0.613 0.258~1.457 肿瘤直径 1.229 0.278 19.465 <0.001 3.417 1.979~5.897 浸润深度 1.460 0.357 17.740 <0.001 4.305 2.182~8.490 脉管浸润 0.005 0.392 < 0.001 0.991 1.005 0.466~2.166 淋巴结转移 0.703 0.338 4.338 0.037 2.021 1.042~3.917 临床分期 -2.517 1.224 4.225 0.040 0.081 0.007~0.890 生长方式 1.018 0.494 4.248 0.039 2.767 1.051~7.283 临床分级 0.022 0.614 0.001 0.972 1.022 0.307~3.402 注:变量赋值如下,年龄≤40岁=0,>40岁=1;肿瘤直径<4 cm=0,≥4 cm=1;浸润深度<1/2=0,>1/2=1;无脉管浸润=0,有脉管浸润=1;无淋巴结转移=0,有淋巴结转移=1。临床分级、生长方式、临床分期设哑变量赋值,分为变量1与变量2。Ⅰ~Ⅱ级=“变量1=1”、Ⅱ级=“变量2=1”、Ⅱ~Ⅲ级=“变量1与变量2=0”;外生型=“变量1=1”、内生型=“变量2=1”、其他型=“变量1与变量2=0”;ⅠA期“变量1=1”、ⅠB期=“变量2=1”、ⅡA期=“变量1与变量2=0”。 表 3 HPV分型、SCC与NLR诊断早期宫颈癌淋巴结转移的相关分析
Table 3. Correlation analysis of HPV typing, SCC and NLR in the diagnosis of lymph node metastasis of early cervical cancer
项目 灵敏度(%) 特异度(%) 阳性似然比(%) 阴性似然比(%) HPV分型 52.94 27.50 13.43 73.33 SCC-Ag 68.16 63.46 33.33 81.16 NLR 61.11 59.13 29.14 81.45 联合 47.06 81.00 45.71 81.82 表 4 HPV分型、SCC-Ag及NLR联合诊断与早期宫颈癌淋巴结转移情况(例)
Table 4. HPV typing, SCC-Ag and NLR combined diagnosis and lymph node metastasis of early cervical cancer (cases)
联合诊断 淋巴结转移 合计 + - + 16 19 35 - 18 81 99 合计 34 100 134 -
[1] ARBYN M, WEIDERPASS E, BRUNI L, et al. Estimates of incidence and mortality of cervical cancer in 2018: A worldwide analysis[J]. Lancet Glob Health, 2020, 8(2): 191-203. doi: 10.1016/S2214-109X(19)30482-6 [2] BHATLA N, AOKI D, SHARMA D N, et al. Cancer of the cervix uteri[J]. Int J Gynaecol Obstet, 2018, 143(2): 22-36. [3] 代维. 宫颈薄层液基细胞学联合高危型人乳头瘤病毒检测在宫颈上皮内瘤变筛查中的价值[J]. 中国妇幼保健, 2017, 32(21): 5438-5440. https://www.cnki.com.cn/Article/CJFDTOTAL-ZFYB201721087.htmDAU W. The value of cervical thin-layer fluid-based cytology combined with high-risk HPV testing in cervical intraepithelial neoplasia screening[J]. Maternal and Child Health Care of China, 2017, 32(21): 5438-5440. https://www.cnki.com.cn/Article/CJFDTOTAL-ZFYB201721087.htm [4] 高琳, 王佐君, 张玲, 等. HPV-DNA分型与血清SCC-Ag、CA125联合检测在宫颈癌早期诊断中的价值[J]. 中国妇幼保健, 2018, 33(24): 5953-5956. https://www.cnki.com.cn/Article/CJFDTOTAL-ZFYB201824095.htmGAO L, WANG Z J, ZHANG L, et al. The value of combined testing with serum SCC-Ag and CA125 in the early diagnosis of cervical cancer[J]. Maternal & Child Health Care of China, 2018, 33 (24): 5953-5956. https://www.cnki.com.cn/Article/CJFDTOTAL-ZFYB201824095.htm [5] YOU W Z, LI S C, DU R. Epidemiological study of high-risk human papillomavirus infection in subjects with abnormal cytological findings in cervical cancer screening[J]. Exp Ther Med, 2018, 15(1): 412-418. [6] 邱峰, 黄匡, 唐虹, 等. HPV分型及血清肿瘤标志物在宫颈癌诊断中的临床意义[J]. 检验医学与临床, 2017, 14(14): 2011-2013, 2016. https://www.cnki.com.cn/Article/CJFDTOTAL-JYYL201714004.htmQIU F, HUANG K, TANG H, et al. The significance of HPV typing and the tumor markers in cervical cancers[J]. Laboratory Medicine and Clinic, 2017, 14 (14): 2011-2013, 2016. https://www.cnki.com.cn/Article/CJFDTOTAL-JYYL201714004.htm [7] 王晓娟, 散琴, 王月明, 等. CEA、CA125、SCC-Ag、CA199及CYFRA21-1等肿瘤标志物在宫颈癌中诊断的价值和意义[J]. 海南医学院学报, 2017, 23(18): 2573-2576. https://www.cnki.com.cn/Article/CJFDTOTAL-HNYY201718032.htmWANG X J, SAN Q, WANG Y M, et al. The value and significance of tumor markers such as CEA, CA125, SCC-Ag, CA199 and CYFRA21-1 in diagnosis of cervical cancer[J]. Journal of Hainan Medical University, 2017, 23(18): 2573-2576. https://www.cnki.com.cn/Article/CJFDTOTAL-HNYY201718032.htm [8] 陈军莹, 姚德生, 伍志娟. SCC-Ag在宫颈鳞癌病例中诊断淋巴结转移效能的meta分析[J]. 肿瘤防治研究, 2012, 39(14): 811-817. https://www.cnki.com.cn/Article/CJFDTOTAL-ZLFY201207014.htmCHEN J Y, YAO D S, WU Z J. Diagnostic Value of Serum Squamous Cell Carcinoma Antigen on Lymphatic Metastasis in Cervical Cancer: a Meta analysis[J]. Cancer Research on Prevention and Treatment, 2012, 39 (14): 811-817. https://www.cnki.com.cn/Article/CJFDTOTAL-ZLFY201207014.htm [9] 赵德英, 张惠等, 方红艳, 等. SCC-Ag与宫颈癌临床病理特征的相关性及对淋巴结转移的预测价值[J]. 武汉大学学报(医学版), 2016, 37(5): 777-781. https://www.cnki.com.cn/Article/CJFDTOTAL-HBYK201605019.htmZHAO D Y, ZHANG H, FANG H Y, et al. Correlations with Clinicopathological Findings and Diagnostic Value for Lymph Node Metastasis of Pretreatment Serum SCC-Ag Levels in Cervical Cancer[J]. Medical Journal of Wuhan University, 2016, 37(5): 777-781. https://www.cnki.com.cn/Article/CJFDTOTAL-HBYK201605019.htm [10] 李可心, 孙洪赞, 辛军, 等. 早期宫颈癌盆腔淋巴结转移危险因素及PET/CT诊断[J]. 中国医学影像技术, 2018, 34(2): 265-269. https://www.cnki.com.cn/Article/CJFDTOTAL-ZYXX201802035.htmLI K X, SUN HZ, XIN J, et al. Risk factors and PET/CT diagnosis of pelvic lymph node metastasis in early-stage cervical cancer[J]. Chinese Journal of Medical Imaging Technology, 2018, 34(2): 265-269. https://www.cnki.com.cn/Article/CJFDTOTAL-ZYXX201802035.htm [11] 张冬雅, 郭红军. 18F-FDG PET-CT联合血清SCC-Ag检测对宫颈癌盆腔淋巴结转移的诊断价值[J]. 中国CT和MRI杂志, 2019, 17(3): 105-108, 153. https://www.cnki.com.cn/Article/CJFDTOTAL-CTMR201903032.htmZHANG D Y, GUO H J. Value of 18F-FDG PET-CT combined with serum SCC-Ag in diagnosing pelvic lymph node metastasis of cervical cancer[J]. Chinese Journal of CT and MRI, 2019, 17(3): 105-108, 153. https://www.cnki.com.cn/Article/CJFDTOTAL-CTMR201903032.htm [12] HAN S, CHENG Z, ZHAO X, et al. Diagnostic value of heat shock protein 90α and squamous cell carcinoma antigen in detection of cervical cancer[J]. J Int Med Res, 2019, 47(11): 5518-5525. doi: 10.1177/0300060519865634 [13] LIU Z, SHI H. Prognostic role of squamous cell carcinoma antigen in cervical cancer: A meta-analysis[J]. Dis Markers, 2019(1): 6710352. DOI: 10.1155/2019/6710352. [14] 秦成义. 术前外周血中性粒细胞/淋巴细胞比值在结直肠癌预后评估中的价值[J]. 中国中西医结合消化杂志, 2019, 27(12): 925-928, 933. https://www.cnki.com.cn/Article/CJFDTOTAL-ZXPW201912010.htmQIN C Y. The value of preoperative peripheral blood neutrophil/lymphocyte ratio in the prognosis of colorectal cancer[J]. Chinese Journal of Integrated Traditional and Western Medicine on Digestion, 2019, 27(12): 925-928, 933. https://www.cnki.com.cn/Article/CJFDTOTAL-ZXPW201912010.htm [15] PRABAWA I P Y, BHARGAH A, LIWANG F, et al. Pretreatment neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR) as a predictive value of hematological markers in cervical cancer[J]. Asian Pac J Cancer Prev, 2019, 20(3): 863-868. doi: 10.31557/APJCP.2019.20.3.863 [16] 王金凤, 李琛, 黄康榕, 等. 术前中性粒细胞和淋巴细胞比值、单核细胞和淋巴细胞比值与宫颈癌患者临床病理特征的相关性[J]. 兰州大学学报(医学版), 2019, 45(5): 25-29. https://www.cnki.com.cn/Article/CJFDTOTAL-LZYX201905008.htmWANG J F, LI S C, HUANG K R, et al. Correlation between preoperative neutrophil-to-lymphocyte ratio, monocyte-to-lymphocyte ratio and clinical pathologic features in patients with cervical cancer[J]. Journal of Lanzhou University (Medical Sciences), 2019, 45(5): 25-29. https://www.cnki.com.cn/Article/CJFDTOTAL-LZYX201905008.htm [17] ZHU M, FENG M, HE F, et al. Pretreatment neutrophillymphocyte and platelet-lymphocyte ratio predict clinical outcome and prognosis for cervical cancer[J]. Clin Chim Acta, 2018, 483(24): 296-302. [18] 梅冰洁, 张国楠. 中性粒细胞、血小板与淋巴细胞比值对中晚期宫颈癌患者预后的评估价值[J]. 现代妇产科进展, 2019, 28(12): 892-895. https://www.cnki.com.cn/Article/CJFDTOTAL-XDFC201912003.htmMEI B J, ZHANG G N. Prognostic value of neutrophil, platelet to lymphocyte ratio in patients with advanced cervical cancer[J]. Progress in Obstetrics and Gynecology, 2019, 28(12): 892-895. https://www.cnki.com.cn/Article/CJFDTOTAL-XDFC201912003.htm [19] TAS M, YAVUZ A, AK M, et al. Neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio in discriminating precancerous pathologies from cervical cancer[J]. J Oncol, 2019(75): 2476082. [20] 林元, 苏红娥, 符春丽, 等. 术前中性粒细胞/淋巴细胞比值与宫颈癌患者术后生存和复发的关系[J]. 现代肿瘤医学, 2020, 28(14): 2501-2504. https://www.cnki.com.cn/Article/CJFDTOTAL-SXZL202014033.htmLIN Y, SU H G, FU C L, et al. The relationship between preoperative neutrophil to lymphocyte ratio and survival and recurrence of cervical cancer patients[J]. Journal of Modern Oncology, 2020, 28(14): 2501-2504. https://www.cnki.com.cn/Article/CJFDTOTAL-SXZL202014033.htm [21] 赵雅文, 董頔, 薛茜文, 等. 术前外周血中NLR、PLR、LMR与早期宫颈癌患者预后的相关性研究[J]. 新疆医科大学学报, 2020, 43(8): 997-1003. https://www.cnki.com.cn/Article/CJFDTOTAL-XJYY202008004.htmZHAO W Y, DONG D, XUE Q W, et al. Correlation between NLR, PLR and LMR in preoperative peripheral blood and prognosis of patients with early cervical cancer[J]. Journal of Xinjiang Medical University, 2020, 28(14): 2501-2504. https://www.cnki.com.cn/Article/CJFDTOTAL-XJYY202008004.htm [22] 王欣, 李永霞, 胡丹, 等. 术前外周血中性粒细胞与淋巴细胞比率、血小板与淋巴细胞比率与宫颈癌的相关性研究[J]. 兰州大学学报(医学版), 2020, 46(5): 55-60. https://www.cnki.com.cn/Article/CJFDTOTAL-LZYX202005010.htmWANG X, LI Y X, HU D, et al. Correlation study between preoperative NLR, PLR in peripheral blood and cervical cancer[J]. Journal of Lanzhou University (Medical Sciences), 2020, 46(5): 55-60. https://www.cnki.com.cn/Article/CJFDTOTAL-LZYX202005010.htm -





 下载:
下载: