Analysis of relationship between non-invasive cardiac output determination and heart rate recovery after exercise
-
摘要:
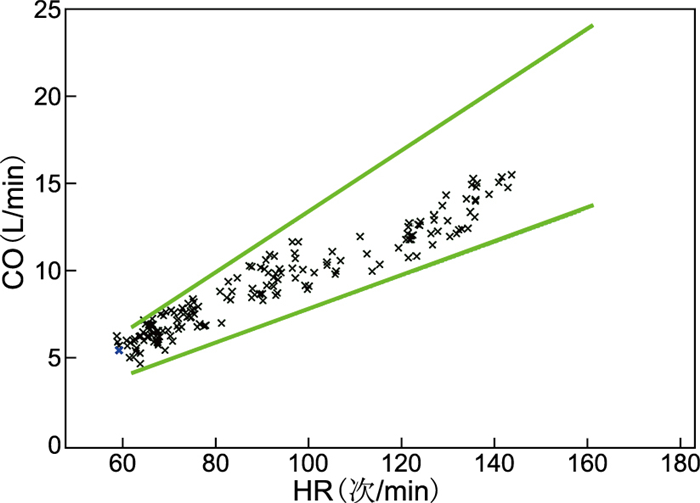
目的 探讨次级限量运动负荷试验中运动心功能与运动后心率恢复的相关性及临床意义。 方法 随机选择2019年8月1日—2021年9月9日在安徽医科大学附属阜阳医院就诊的74例同步行次级限量运动试验及运动心排患者,根据运动中心排血量(CO)的水平分为异常组(35例)和正常组(39例),对比分析各项临床资料、运动心功能各项指标及平板运动试验的数据。 结果 (1) 2组基线资料(年龄、性别、体重指数、病史)差异均无统计学意义(均P>0.05);(2)2组静息状态射血分数(EF)及心指数(CI)、左心做功指数(LCWI)、外周血管阻力(SVR)差异均无统计学意义(均P>0.05);(3)运动峰值:CI、LCWI异常组较正常组显著减低(均P<0.01),SVR异常组较正常组显著增高(P<0.05);(4)每搏输出量(SV)在静息及运动峰值时异常组均低于正常组,差异有统计学意义(P<0.05);(5)静息心率:异常组为(87.688±12.966)次/min,高于正常组的(77.359±11.226)次/min,P<0.05;(6)运动后心率恢复:异常组HRR1为(22.971±8.259)次/min,HRR2为(37.229±8.110)次/min,较正常组明显减低[(27.769±9.184)次/min、(42.513±10.298)次/min,均P<0.05]。 结论 静息心率和运动后心率恢复与运动心功能密切相关,静息心率高和运动后心率恢复不良均可提示心脏功能受损或不良。 Abstract:Objective To investigate the correlation between cardiac function during secondary limited exercise load test and heart rate recovery after exercise and its clinical significance. Methods A total of 74 patients admitted to Fuyang Hospital Affiliated to Anhui Medical University from August 1, 2019 to September 9, 2021 were randomly selected from secondary limited exercise treadmill test and exercise cardiac output test. They were divided into abnormal group (n=35) and normal group (n=39) in accordance with the cardiac output (CO) level of the exercise centre. The clinical data, exercise cardiac function index and Submaximal treadmill exercise test data were compared and analysed. Results (1) No significant difference was observed in the baseline data (age, gender, body mass index and medical history) between the two groups (all P > 0.05). (2) No statistical difference was found in the ejection fraction (EF), resting state cardiac index (CI), left cardiac work index (LCWI) and systemic vascular resistance (SVR) between the two groups (all P > 0.05). (3) The peak movement of CI and LCWI of the abnormal group were significantly lower than those of the normal group (all P < 0.01), whilst SVR of the abnormal group was significantly higher than that of the normal group (P < 0.05). (4) For stroke volume (SV) in static, the resting heart rate of abnormal group was lower than that of normal group at peak rest and exercise, with statistical difference (P < 0.05). (5) The resting heart rate of abnormal group [(87.688±12.966) times/min] was higher than that of normal group [(77.359±11.226) times/min, P < 0.05]. (6) For heart rate recovery after exercise, the HRR1 [(22.971±8.259) times/min] and HRR2 [(37.229±8.110) times/min] of abnormal group were significantly lower than those of normal group [(27.769±8.110) times/min and (42.513±10.298) times/min, all P < 0.05]. Conclusion Resting heart rate and post-exercise heart rate recovery are closely related to exercise cardiac function. High resting heart rate and poor heart rate recovery after exercise may indicate impaired or poor cardiac function. -
表 1 2组行次极量运动负荷试验患者基本资料比较
Table 1. Comparison of basic data of two groups of patients
组别 例数 性别(例) 年龄(x±s,岁) BMI(x±s) 运动平板试验(例) 收缩压(x±s,mm Hg) 舒张压(x±s,mm Hg) 伴血脂异常[例(%)] 伴糖尿病[例(%)] 伴高血压[例(%)] 伴冠心病[例(%)] 男性 女性 阳性 阴性 异常组 35 22 13 45.943±10.035 24.530±2.666 8 27 122.940±19.225 84.290±11.610 14(40.0) 7(20.0) 9(25.7) 2(5.7) 正常组 39 21 18 47.923±12.583 24.564±3.009 13 26 126.870±12.796 82.280±9.202 8(20.5) 5(12.8) 7(17.9) 3(7.6) 统计量 0.615a -0.743b -0.051b 0.996 -1.045b 0.827b P值 0.433 0.460 0.960 0.318 0.300 0.411 0.080c 0.531c 0.573c 0.999c 注:a为χ2值,b为t值,c为采用Fisher精确检验。 表 2 2组行次极量运动负荷试验患者心功能指标比较(x±s)
Table 2. Comparison of cardiac function indexes between two groups of patients
组别 例数 SV(mL) CI[L/(min·m2)] LCWI[(kg·m)/m2] SVR[(dyn·s)/cm5] EF(%) 静息状态 运动峰值 静息状态 运动峰值 静息状态 运动峰值 静息状态 运动峰值 静息状态 运动峰值 异常组 35 69.783±15.569 93.306±23.637 3.317±0.879 7.834±1.562 4.497±1.869 11.397±2.614 1 312.800±247.603 629.800±203.749 60.151±9.692 70.689±11.747 正常组 39 79.113±12.203 115.059±20.237 3.367±0.579 9.282±1.413 4.508±0.958 13.500±2.600 1 319.080±260.313 520.462±94.064 61.192±11.743 71.759±12.549 t值 -2.884 -4.264 -0.289 -4.187 -0.031 -3.465 -0.106 3.014 -0.413 -0.378 P值 0.005 <0.001 0.773 <0.001 0.975 <0.001 0.916 0.004 0.681 0.707 表 3 2组行次极量运动负荷试验患者心率恢复相关指标比较
Table 3. Comparison of related indexes of heart rate recovery between two groups of patients
组别 例数 初始心率(x±s,次/min) 峰值心率(x±s,次/min) HRR1(x±s,次/min) HRR2(x±s,次/min) HRR3(x±s,次/min) 运动心率峰值时间(x±s,min) 心率恢复平稳时间(例) <4 min ≥4 min且<6 min ≥6 min 异常组 35 88.110±13.584 151.657±11.448 22.971±8.259 37.229±8.110 45.114±10.437 13.491±4.386 18 13 4 正常组 39 77.359±11.226 146.154±13.416 27.769±9.184 42.513±10.298 48.564±9.489 14.066±3.477 17 15 7 统计量 3.727a 1.887a -2.353a -2.433a -1.489a -0.629a -0.817b P值 <0.001 0.063 0.021 0.017 0.141 0.531 0.414 注:a为t值,b为Z值。 -
[1] 张玉娟. 平板运动试验后心率恢复延迟对冠心病诊断价值的研究[D]. 苏州: 苏州大学, 2020.ZHANG Y J. Diagnostic value of delayed heart rate recovery after treadmill exercise test for coronary heart disease[D]. Suzhou: Suzhou University, 2020. [2] QIU S H, CAI X, SUN Z L, et al. Heart rate recovery and risk of cardiovascular events and all-cause mortality: A meta-analysis of prospective cohort studies[J]. J Am Heart Assoc, 2017, 6(5): e005505. doi: 10.1161/JAHA.117.005505 [3] 刘小群, 黄峰, 朱鹏立. 运动后心率恢复的临床意义[J]. 中华高血压杂志, 2021, 29(5): 413-419. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGGZ202105005.htmLIU X Q, HUANG F, ZHU P L. Clinical significance of heart rate recovery after exercise[J]. Chinese Journal of Hypertension, 2021, 29(5): 413-419. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGGZ202105005.htm [4] 李晨洋, 叶继伦, 张旭, 等. 基于胸阻抗法的心排量检测系统研制[J]. 中国医学物理学杂志, 2019, 36(7): 818-825. doi: 10.3969/j.issn.1005-202X.2019.07.014LI C Y, YE J L, ZHANG X, et al. Development of cardiac output monitor based on thoracic impedance method[J]. Chinese Journal of Medical Physics, 2019, 36(7): 818-825. doi: 10.3969/j.issn.1005-202X.2019.07.014 [5] 王卓清, 李永豪, 郭元芳, 等. 心功能不同时期患者的无创血流动力学检测分析[J]. 军事医学, 2017, 41(8): 675-679. https://www.cnki.com.cn/Article/CJFDTOTAL-JSYX201708014.htmWANG Z Q, LI Y H, GUO Y F, et al. Analysis of noninvasive hemodynamics in patients with cardiac disfunction during different periods[J]. Military Medical Sciences, 2017, 41(8): 675-679. https://www.cnki.com.cn/Article/CJFDTOTAL-JSYX201708014.htm [6] 何方田. 临床心电图精典[M]. 杭州: 浙江大学出版社, 2018: 452-453.HE F T. Classic clinical electrocardiogram[M]. Hangzhou: Zhejiang University Press, 2018: 452-453. [7] 徐关祥, 宋义林. 基于胸部电阻抗法的无拘束心排血量检测系统[J]. 中国医疗器械杂志, 2018, 42(6): 405-408. doi: 10.3969/j.issn.1671-7104.2018.06.004XU G X, SONG Y L. Unconstrained Cardiac Output Measurement System Based on Thoracic Electrical Impedance Method[J]. Chinese Journal of Medical lnstrumentation, 2018, 42(6): 405-408. doi: 10.3969/j.issn.1671-7104.2018.06.004 [8] HARADA T, YAMAGUCHI M, OMOTE K, et al. Cardiac power output is independently and incrementally associated with adverse outcomes in heart failure with preserved ejection fraction[J]. Circ Cardiovasc Imaging, 2022, 15(2): e013495. doi: 10.1161/CIRCIMAGING.121.013495 [9] PANDHITA B A W, OKWOSE N C, KOSHY A, et al. Noninvasive assessment of cardiac output in advanced heart failure and heart transplant candidates using the bioreactance method[J]. J Cardiothorac Vasc Anesth, 2021, 35(6): 1776-1781. doi: 10.1053/j.jvca.2020.09.109 [10] CORRIERI N, DEL TORTO A, VIGNATI C, et al. Cardiac output changes during exercise in heart failure patients: Focus on mid-exercise[J]. ESC Heart Fail, 2021, 8(1): 55-62. doi: 10.1002/ehf2.13005 [11] 曹雅兰, 向姝婷, 王钰, 等. 射血分数保留心力衰竭患者无创血流动力学与超声心动图一年随访的对比研究[J]. 中国医师进修杂志, 2020, 43(8): 691-695. doi: 10.3760/cma.j.cn115455-20200210-00119CAO Y L, XIANG Z T, WANG Y, et al. Comparative study of non-invasive hemodynamics and echocardiography on heart failure with preserved ejection fraction patients: one year follow-up[J]. Chinese Journal of Postgraduates of Medicine, 2020, 43(8): 691-695. doi: 10.3760/cma.j.cn115455-20200210-00119 [12] 吕航. 平板运动后心率恢复对冠心病的诊断价值[J]. 实用心电学杂志, 2019, 28(1): 38-41. https://www.cnki.com.cn/Article/CJFDTOTAL-SYXD201901031.htmLV H. Diagnostic value of heart rate recovery after treadmill exercise in patients with coronary heart disease[J]. Journal of Practical Electrocardiology, 2019, 28(1): 38-41. https://www.cnki.com.cn/Article/CJFDTOTAL-SYXD201901031.htm [13] PEARSON M J, SMART N A. Exercise therapy and autonomic function in heart failure patients: A systematic review and meta-analysis[J]. Heart Failure Reviews, 2017, 23(11): 1-18. [14] 康菁芬. 运动心肌血流灌注显像负荷试验心率恢复与心功能参数的相关性分析[D]. 太原: 山西医科大学, 2021.KANG J F. Correlation between heart rate recovery and cardiac function parameters in exercise myocardial perfusion imaging stress test[D]. Taiyuan: Shanxi Medical University, 2021. [15] SADOUDI-ÉPSE-YAKER G, SAID-OUAMER D, BENKHEDDA S. The information provided by the exercise capacity and the heart rate recovery during an exercise test in athletes[J]. Retour Au Numéro, 2018, 10(1): 124. [16] RODRÍGUEZ-FERNÁNDEZ A, SANCHEZ-SANCHEZ J, RAMIREZ-CAMPILLO R, et al. Relationship between repeated sprint ability, aerobic capacity, intermittent endurance, and heart rate recovery in youth soccer players[J]. Strength Cond Res, 2019, 33(12): 3406-3413. doi: 10.1519/JSC.0000000000002193 [17] 刘红敏, 陈朔华, 吴云涛, 等. 静息心率加快增加人群新发心力衰竭风险[J]. 中华心血管病杂志, 2020, 48(5): 413-419. doi: 10.3760/cma.j.cn112148-20190703-00374LIU H M, CHEN S H, WU Y T, et al. A cohort study on the association between resting heart rate and the risk of new-onset heart failure[J]. Chinese Journal of Cardiology, 2020, 48(5): 413-419. doi: 10.3760/cma.j.cn112148-20190703-00374 [18] SHI Y Y, ZHOU W, LIU X J, et al. Resting heart rate and the risk of hypertension and heart failure: A dose-response meta-analysis of prospective studies[J]. Hypertens, 2018, 36(5): 995-1004. doi: 10.1097/HJH.0000000000001627 [19] 叶丽丽, 邱健, 阮云军. 静息心率与冠心病患者冠状动脉病变和左心室功能的相关性[J]. 实用医学杂志, 2017, 33(22): 3756-3759. doi: 10.3969/j.issn.1006-5725.2017.22.020YE L L, QIU J, RUAN Y J. Association of resting heart rate and coronary artery lesions with left ventricular function in coronary heart disease[J]. The Journal of Practical Medicine, 2017, 33(22): 3756-3759. doi: 10.3969/j.issn.1006-5725.2017.22.020 [20] 施益忠, 姚亚军, 陈维明, 等. 交感-肾上腺髓质系统的改变对心衰的评估意义[J]. 中华全科医学, 2015, 13(1): 154-156. https://www.cnki.com.cn/Article/CJFDTOTAL-SYQY201501060.htmSHI Y Z, YAO Y J, CHEN W M, et al. he significance of sympathetic - adrenal medulla system changes in the evaluation of heart failure[J]Chinese Journal of General Practice, 2015, 13(1): 154-156. https://www.cnki.com.cn/Article/CJFDTOTAL-SYQY201501060.htm [21] 陆铭, 蒋庆渊, 刘春兰, 等. 心率控制对慢性心力衰竭患者炎症因子及心功能的影响[J]. 实用医学杂志, 2017, 33(19): 3235-3239. doi: 10.3969/j.issn.1006-5725.2017.19.021LU M, JIANG Q Y, LIU C L, et al. Influence of intensive heart rate control on inflammatory factor and cardiac function in patients with chronic heart failure[J]. The Journal of Practical Medicine, 2017, 33(19): 3235-3239. doi: 10.3969/j.issn.1006-5725.2017.19.021 -





 下载:
下载: