Analysis of complications and influencing factors of sinus tarsal incision mini-plate combined with hollow nail internal fixation for treatment of calcaneal fractures
-
摘要:
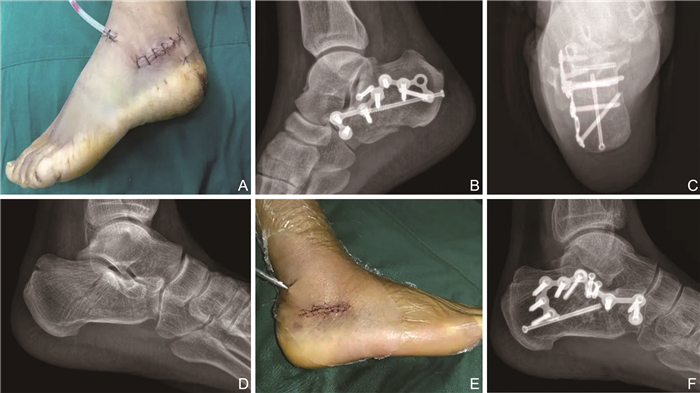
目的 研究跗骨窦切口微型钢板联合空心钉内固定治疗跟骨骨折的并发症及影响因素。 方法 选取2018年7月—2020年6月浙江大学医学院附属第二医院创伤骨科收治的84例跟骨骨折患者,并对其临床资料进行回顾性研究,根据不同术式将其分为对照组和跗骨窦组,每组各42例。对照组行外侧“L”形切口内固定手术,跗骨窦组行跗骨窦切口微创钢板及空心钉轴向内固定手术,比较切口长度、出血量、消肿时间、愈合拆线时间、Bohler角、Gissane角、后踝后足功能改善率、并发症发生率。采用logistic回归分析研究术后并发症的影响因素。 结果 跗骨窦组切口长度、出血量、消肿时间、愈合拆线时间短于对照组,差异有统计学意义(均P<0.05)。Bohler角跗骨窦组高于对照组,差异有统计学意义(P<0.05), 而2组Gissane角差异无统计学意义(P>0.05)。跗骨窦组总改善率为90.5%(38/42),高于对照组61.9%的改善率(26/42, P<0.05)。跗骨窦组并发症发生率为28.6%(12/42),低于对照组50.0%(21/42)的发生率,差异有统计学意义(P<0.05)。回归分析显示手术方式、消肿时间、愈合拆线时间、Bohler角、年龄、功能改善是影响术后并发症发生的因素。 结论 跗骨窦切口微型钢板联合空心钉内固定治疗跟骨骨折优于L形切口,而手术方式、消肿时间、愈合拆线时间、Bohler角、年龄、功能改善等因素影响手术预后效果。 Abstract:Objective To explore the complications and influencing factors of calcaneal fractures treated with tarsal sinus incision microplate combined with cannulated screw internal fixation. Methods From July 2018 to June 2020, 84 patients with calcaneal fractures admitted to the Department of Traumatology and Orthopaedics of the Second Affiliated Hospital of Zhejiang University School of Medicine were selected, and their clinical data were retrospectively studied. They were divided into control group and tarsal sinus group in accordance with different surgical procedure, with 42 cases in each group. The control group underwent lateral "L"-shaped incision internal fixation and the tarsal sinus group underwent minimally invasive tarsal sinus incision plate and cannulated screw axial internal fixation. The Bohler angle, Gissane angle, improvement rate of hind ankle and hindfoot function and complication rate were determined. Logistic regression was used to analyse the influencing factors of postoperative complications. Results The length of incision, the amount of blood loss, the time for detumescence and the time for healing and removing sutures in the sinus tarsi group were shorter than those in the control group, the differences were statistically significant (all P < 0.05). The Bohler angle was higher in the sinus tarsi group than in the control group and the difference was statistically significant (P < 0.05). On the contrary, no significant difference was found in the Gissane angle between the two groups (P>0.05). The total improvement rate of the sinus tarsi group was 90.5% (38/42), which was higher than that of the control group at 61.9% (26/42), and the difference was statistically significant (P < 0.05). The incidence of complications in the sinus tarsi group (28.6%, 12/42) was lower than that in the control group (50.0%, 21/42) and the difference was statistically significant (P < 0.05). Regression analysis showed that operation method, swelling time, suture removal time, Bohler angle, age, and functional improvement were independent risk factors for postoperative complications. Conclusion Tarsal sinus incision microplate combined with cannulated screw internal fixation is better than L-shaped incision in the treatment of calcaneal fractures. Factors such as surgical method, detumescence time, healing and suture removal time, Bohler angle, age and functional improvement affect the prognosis of surgery. -
表 1 2组跟骨骨折患者基线资料情况
Table 1. Baseline data of patients with calcaneal fractures in the two groups
组别 例数 性别[例(%)] 骨折部位[例(%)] 分型[例(%)] 年龄(x±s,岁) 男性 女性 右侧 左侧 Ⅱ型 Ⅲ型 对照组 42 23(54.8) 19(45.2) 21(50.0) 21(50.0) 22(52.4) 20(47.6) 55.45±10.42 跗骨窦组 42 25(59.5) 17(40.5) 24(57.1) 18(42.9) 26(61.9) 16(38.1) 57.23±8.45 统计量 0.194a 0.431a 0.378a 0.860b P值 0.659 0.512 0.508 0.392 注:a为χ2值,b为t值。 表 2 2组跟骨骨折患者围手术期指标比较(x±s)
Table 2. Comparison of perioperative indexes between two groups of patients with calcaneal fracture
组别 例数 切口长度(cm) 出血量(mL) 消肿时间(d) 愈合时间(d) 愈合拆线时间(d) Bohler角(°) Gissane角(°) 跗骨窦组 42 5.14±1.25 27.89±14.68 2.08±0.47 46.68±8.49 13.58±0.68 30.69±5.68 128.36±14.68 对照组 42 11.36±1.31 86.69±13.78 3.38±1.24 53.49±10.47 19.68±0.53 28.24±5.37 123.67±14.38 t值 22.252 18.927 6.348 3.274 45.876 2.031 1.479 P值 <0.001 <0.001 <0.001 0.002 <0.001 0.045 0.143 表 3 2组跟骨骨折患者后踝后足功能改善率比较[例(%)]
Table 3. Comparison of function improvement rate of posterior ankle and hind foot in patients with calcaneal fracture between two groups[cases(%)]
组别 例数 优 良 可 差 总改善 跗骨窦组 42 13(31.0) 16(38.1) 9(21.4) 4(9.5) 38(90.5) 对照组 42 3(7.1) 10(23.8) 13(31.0) 16(38.1) 26(61.9) 注:2组总改善率比较,χ2=9.450, P=0.002。 表 4 2组跟骨骨折患者并发症总发生率比较[例(%)]
Table 4. Comparison of the total incidence of complications in patients with calcaneal fracture between two groups[cases(%)]
组别 例数 关节疼痛 距下关节炎 软组织损伤 切口红肿 皮缘坏死 总发生 跗骨窦组 42 1(2.4) 1(2.4) 1(2.4) 5(11.9) 4(9.5) 12(28.6) 对照组 42 4(9.5) 6(14.3) 4(9.5) 4(9.5) 3(7.1) 21(50.0) 注:2组总发生率比较,χ2=4.043,P=0.044。 表 5 有无并发症跟骨骨折患者基础情况比较
Table 5. Comparison of basic condition of patients with and without complication calcaneal fracture
项目 并发症 统计量 P值 无(n=51) 有(n=33) 手术方式[例(%)] 4.043a 0.044 联合术式(n=42) 21(41.2) 21(63.6) 外侧术式(n=42) 30(58.8) 12(36.4) 性别[例(%)] 0.004a 0.949 男性(n=48) 29(56.9) 19(57.6) 女性(n=36) 22(43.1) 14(42.4) 骨折部位[例(%)] 0.350a 0.554 右侧(n=45) 26(51.0) 19(57.6) 左侧(n=39) 25(49.0) 14(42.4) 分型[例(%)] 0.266a 0.606 Ⅱ型(n=48) 28(54.9) 20(60.6) Ⅲ型(n=36) 23(45.1) 13(39.4) 功能改善[例(%)] 18.243a <0.001 无改善(n=20) 4(7.8) 16(48.5) 有改善(n=64) 47(92.2) 17(51.5) 消肿时间(x±s,d) 2.49±0.97 3.10±1.29 2.460b 0.016 愈合拆线时间(x±s,d) 16.15±3.03 17.37±3.18 1.756b 0.083 Bohler角(x±s,°) 29.24±6.13 29.81±4.83 0.452b 0.652 Gissane角(x±s,°) 126.55±16.11 125.19±12.19 0.415b 0.679 切口长度(x±s,cm) 7.75±3.18 9.02±3.57 1.701b 0.093 出血量(x±s,mL) 62.08±34.08 49.88±29.66 1.685b 0.096 年龄(x±s,岁) 59.02±15.66 64.06±15.17 1.467b 0.146 愈合时间(x±s,d) 49.38±11.68 51.47±11.38 1.970 0.052 注:a为χ2值, b为t值。 表 6 跟骨骨折患者并发症影响因素的多因素logistic回归分析
Table 6. Multivariate logistic regression analysis of influencing factors of complications in patients with calcaneal fracture
变量 B SE Wald χ2 P值 OR值 95% CI 手术方式 -11.641 4.726 6.067 0.014 0.000 0.000~0.093 消肿时间 1.026 0.437 5.526 0.019 2.791 1.186~6.568 愈合拆线时间 -1.991 0.781 6.494 0.011 0.137 0.030~0.631 Bohler角 0.155 0.077 4.050 0.044 1.167 1.004~1.357 年龄 -0.052 0.022 5.896 0.015 0.949 0.910~0.990 功能改善 -2.546 0.754 11.386 0.001 0.078 0.018~0.344 -
[1] LEMS W F, PACCOU J, ZHANG J, et al. Vertebral fracture: Epidemiology, impact and use of dxa vertebral fracture assessment in fracture liaison services[J]. Osteoporos Int, 2021, 32(3): 399-411. doi: 10.1007/s00198-020-05804-3 [2] ZHANG C, YE Z M, LIN P, et al. Lateral fracture-dislocation of the calcaneus: Case reports and a systematic review[J]. Orthop Surg, 2021, 13(3): 682-691. doi: 10.1111/os.12913 [3] LI Z H, WU X B, ZHOU H C, et al. Cost-utility analysis of extensile lateral approach versus sinus tarsi approach in sanders type Ⅱ/Ⅲ calcaneus fractures[J]. J Orthop Surg Res, 2020, 15(1): 430. doi: 10.1186/s13018-020-01963-5 [4] 黄朱宋, 陈翔, 蓝锦福, 等. 跗骨窦切口微型钢板联合空心钉内固定与L形切口钢板内固定治疗跟骨骨折的疗效比较[J]. 中国骨与关节损伤杂志, 2020, 35(2): 205-207. https://www.cnki.com.cn/Article/CJFDTOTAL-GGJS202002037.htmHUANG Z S, CHEN X, LAN F J, et al. Comparison of the efficacy of tarsal sinus incision micro plate combined with hollow nail internal fixation and L-shaped incision plate internal fixation in the treatment of calcaneal fractures[J]. Chinese Journal of Bone and Joint Injury, 2020, 35(2): 205-207. https://www.cnki.com.cn/Article/CJFDTOTAL-GGJS202002037.htm [5] 周亮, 徐宏宇, 周海东. 跗骨窦切口微型钢板结合空心钉内固定治疗跟骨骨折[J]. 临床骨科杂志, 2020, 23(6): 891-894. doi: 10.3969/j.issn.1008-0287.2020.06.046ZHOU L, XU H Y, ZHOU H D. Treatment of calcaneal fracture with mini-plate and cannulated screw internal fixation with tarsal sinus incision[J]. Journal of Clinical Orthopaedics, 2020, 23(6): 891-894. doi: 10.3969/j.issn.1008-0287.2020.06.046 [6] 李瑞, 曲鑫, 王玲. 跟骨骨折经皮复位固定术后渐进性康复与护理[J]. 实用临床医药杂志, 2020, 24(13): 71-74. https://www.cnki.com.cn/Article/CJFDTOTAL-XYZL202013022.htmLI R, QU X, WANG L. Progressive rehabilitation and nursing for calcaneal fractures after percutaneous reduction and fixation[J]. Journal of Clinical Medicine in Practice, 2020, 24(13): 71-74. https://www.cnki.com.cn/Article/CJFDTOTAL-XYZL202013022.htm [7] 梁耘. 两种不同缝合方法对跟骨骨折术患者愈合情况、伤口血运及并发症的影响[J]. 实用医院临床杂志, 2019, 16(5): 163-166. https://www.cnki.com.cn/Article/CJFDTOTAL-YYLC201905049.htmLIANG Y. The effects of two different suture methods on healing, wound blood supply and complications of patients undergoing calcaneal fracture surgery[J]. Practical Journal of Clinical Medicine, 2019, 16(5): 163-166. https://www.cnki.com.cn/Article/CJFDTOTAL-YYLC201905049.htm [8] GALLUZZO M, GRECO F, PIETRAGALLA M, et al. Calcaneal fractures: Radiological and CT evaluation and classification systems[J]. Acta Biomed, 2018, 89(1-S): 138-150. [9] RODEMUND C, KRENN R, KIHM C, et al. minimally invasive surgery for intra-articular calcaneus fractures: A 9-year, single-center, retrospective study of a standardized technique using a 2-point distractor[J]. BMC Musculoskelet Disord, 2020, 21(1): 753. doi: 10.1186/s12891-020-03762-9 [10] PENG Y, LIU J H, ZHANG G Z, et al. Reduction and functional outcome of open reduction plate fixation versus minimally invasive reduction with percutaneous screw fixation for displaced calcaneus fracture: A retrospective study[J]. J Orthop Surg Res, 2019, 14(1): 124. doi: 10.1186/s13018-019-1162-5 [11] 王彦志, 邢兆国, 贾东昭, 等. 跗骨窦切口微型板结合空心钉轴向固定治疗跟骨骨折疗效观察[J]. 现代中西医结合杂志, 2019, 28(28): 3124-3126, 3162. doi: 10.3969/j.issn.1008-8849.2019.28.011WANG Y Z, XING Z G, JIA D Z, et al. Observation on the curative effect of tarsal sinus incision micro plate combined with hollow nail axial fixation for calcaneal fracture[J]. Modern Journal of Integrated Traditional Chinese and Western Medicine, 2019, 28(28): 3124-3126, 3162. doi: 10.3969/j.issn.1008-8849.2019.28.011 [12] 谢建新, 郑小飞, 路磊, 等. 跗骨窦切口经皮撬拨空心钉内固定治疗SANDERS Ⅱ型跟骨骨折[J]. 临床骨科杂志, 2018, 21(5): 116-117, 120. https://www.cnki.com.cn/Article/CJFDTOTAL-LCGK201805048.htmXIE J X, ZHENG X F, LU L, et al. Percutaneous poking cannulated screw fixation and minimally invasive in treatment of Sanders type Ⅱ calcaneal fracture via calcaneal sinus incision[J]. Journal of Clinical Orthopaedics, 2018, 21(5): 116-117, 120. https://www.cnki.com.cn/Article/CJFDTOTAL-LCGK201805048.htm [13] 洪伟武, 苏海涛, 彭嘉杰, 等. 经跗骨窦切口与传统L形切口治疗跟骨骨折: 系统评价与META分析[J]. 中国组织工程研究, 2020, 24(18): 2939-2944. doi: 10.3969/j.issn.2095-4344.2637HONG W W, SU H T, PENG J J, et al. Transtarsal sinus incision and traditional L-shaped incision for calcaneal fractures: a systematic evaluation and meta-analysis[J]. Chinese Journal of Tissue Engineering Research, 2020, 24(18): 2939-2944. doi: 10.3969/j.issn.2095-4344.2637 [14] 潘永雄, 洪劲松, 付小勇, 等. 经跗骨窦切口与经外侧L型切口治疗跟骨骨折在内侧壁与跟骨力线的比较研究[J]. 中华创伤骨科杂志, 2018, 20(12): 1095-1100. doi: 10.3760/cma.j.issn.1671-7600.2018.12.015PAN Y X, HONG J S, FU X Y, et al. Comparison of sinus tarsi and lateral L-shaped approaches in medial wall reduction and calcaneal alignment in treatment of calcaneal fractures[J]. Chinese Journal of Orthopaedic Trauma, 2018, 20(12): 1095-1100. doi: 10.3760/cma.j.issn.1671-7600.2018.12.015 [15] 廉养杰. 跗骨窦切口空心螺钉内固定治疗对SANDERS Ⅲ型跟骨骨折患者BOHLER角、GISSANE角、跟骨高度与宽度的影响[J]. 实用临床医药杂志, 2019, 23(2): 14-17. https://www.cnki.com.cn/Article/CJFDTOTAL-XYZL201902005.htmLIAN Y J. Effects of hollow screw internal fixation of tarsal sinus incision on the Bohler angle, Gissane angle, calcaneus height and width in patients with Sanders type Ⅲ calcaneal fractures[J]. Journal of Clinical Medicine in Practice, 2019, 23(2): 14-17. https://www.cnki.com.cn/Article/CJFDTOTAL-XYZL201902005.htm [16] PFLVGER P, ZYSKOWSKI M, GREVE F, et al. Patient-reported outcome following operative and conservative treatment of calcaneal fractures: A retrospective analysis of 79 patients at short-to midterm follow-up[J]. Front Surg, 2021, 8: 620964. doi: 10.3389/fsurg.2021.620964 [17] 朱岩, 朱杰, 周光新, 等. 一期手术治疗63例CIERNY-MADER Ⅱ型及Ⅲ型慢性跟骨骨髓炎的单中心临床诊疗分析[J]. 中华全科医学, 2021, 19(10): 1654-1657, 1684. doi: 10.16766/j.cnki.issn.1674-4152.002134ZHU Y, ZHU J, ZHOU G X, et al. One-stage surgical treatment for Cierny-Mader type Ⅱ and Ⅲ chronic calcaneus osteomyelitis: Single-centre experience of 63 cases[J]. Chinese Journal of General Practice, 2021, 19(10): 1654-1657, 1684. doi: 10.16766/j.cnki.issn.1674-4152.002134 [18] 爱新觉罗启承, 李昶, 范永宏, 等. "八"字双切口钢板内固定治疗跟骨骨折常见并发症及影响因素分析[J]. 中国医药导报, 2019, 16(18): 69-72. https://www.cnki.com.cn/Article/CJFDTOTAL-YYCY201918018.htmAISINGIORO Q C, LI C, FAN Y H, et al. Analysis of common complications and influencing factors of "eightshaped" double incision steel plate internal fixation in the treatment of calcaneal fracture[J]. China Medical Herald, 2019, 16(18): 69-72. https://www.cnki.com.cn/Article/CJFDTOTAL-YYCY201918018.htm [19] RAMMELT S, SANGEORZAN B J, SWORDS M P. Calcaneal fractures - should we or should we not operate?[J]. Indian J Orthop, 2018, 52(3): 220-230. [20] SCHINDLER C, SCHIRM A, ZDRAVKOVIC V, et al. Outcomes of intra-articular calcaneal fractures: Surgical treatment of 114 consecutive cases at a maximum care trauma center[J]. BMC Musculoskelet Disord, 2021, 22(1): 234. -





 下载:
下载: