Application of ultrasound imaging technology to evaluate the localisation of endotracheal intubation in critically ill premature infants
-
摘要:
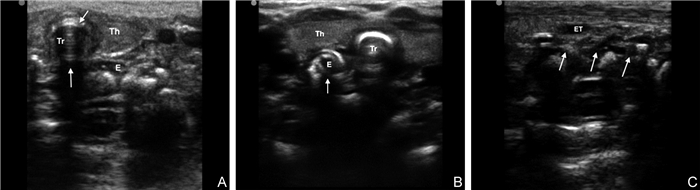
目的 探讨超声成像技术评估危重早产儿气管内插管定位的临床应用效果。 方法 选择2019年1月—2021年1月于南京医科大学第一附属医院新生儿监护病房住院并接受气管内插管术的103例早产儿为研究对象,以定位气管内插管方式的不同,分为超声定位组(50例)和以听诊肺部及胃泡判断气管导管在位的对照组(53例),导管固定后均采用胸部X线评估导管的位置。观察并分析超声组声像图特征,比较组间定位气管导管适宜率、误入食管率、误入主支气管(置管过深)率、脱管(置管过浅)率,评价2种方式定位导管的准确性。 结果 超声组定位导管适宜率(86.0% vs. 54.7%, P=0.001)高于对照组,误入主支气管率(6.0% vs. 20.8%, P=0.029)、脱管率(4.0% vs. 17.0%, P=0.033)低于对照组;以X线定位气管导管位置适宜为金标准,2组定位方式为筛查标准,发现超声组定位灵敏度(91.1% vs. 88.9%)、特异度(80.0% vs. 11.8%)、约登指数(71.1% vs. 6.5%)及Kappa一致性系数(0.561 vs. 0.008)均明显高于对照组。 结论 超声成像技术评估气管导管定位实时、有效,可准确判断导管位置及深度,减少放射性暴露累积,值得在危重早产儿中推广应用。 Abstract:Objective To evaluate the clinical application of ultrasound imaging technology in the localisation of endotracheal intubation in critically ill preterm infants. Methods A total of 103 critically ill premature infants who received endotracheal intubation in the neonatal intensive care unit of the First Affiliated Hospital of Nanjing Medical University from January 2019 to January 2021 were selected as the research object. By different methods of positioning endotracheal tube, they were divided into ultrasound group (50 cases) and control group (53 cases) by auscultation of lung and gastric vesicle. After the catheter was fixed, the catheter's position was evaluated by chest X-ray. The ultrasonographic characteristics of the ultrasound group were observed and analysed. Moreover, the suitability rate of endotracheal tube positioning and the rates of mistakenly entering the oesophagus and main bronchus (catheterisation too deep) and detubation (catheterisation too shallow) were compared between the two groups to evaluate the accuracy of endotracheal tube positioning by different methods. Results The suitability rate of catheter positioning in the ultrasound group was higher than that in the control group (86.0% vs. 54.7%, P=0.001). The rates of mistakenly entering the main bronchus (6.0% vs. 20.8%, P=0.029) and detubation (4.0% vs. 17.0%, P=0.033) were lower than those in the control group (P < 0.05). The suitability of X-ray localisation of endotracheal tube was taken as the gold standard, and the localisation mode of the two groups was considered as the screening standard. The Youden index (71.1% vs. 6.5%), sensitivity (91.1% vs. 88.9%), specificity (80.0% vs. 11.8%) and Kappa consistency coefficient (0.561 vs. 0.008) in the ultrasound group were significantly higher than those in the control group. Conclusion Ultrasound imaging technology can effectively evaluate the positioning of the endotracheal tube in real time. It can accurately judge the position and depth of the endotracheal tube and reduce the accumulation of radiation exposure. It is worthy to be popularised and applied in critically ill preterm infants. -
Key words:
- Ultrasonic imaging technology /
- Endotracheal intubation /
- Localisation /
- Premature infant
-
表 1 2组早产儿基线资料比较
Table 1. Comparison of baseline data between two groups of preterm infants
组别 例数 性别[例(%)] 剖宫产[例(%)] 胎龄(x±s,周) 体重(x±s,g) Apgar评分(x±s,分) 男 女 超声组 50 29(58.0) 21(42.0) 18(36.0) 30.4±2.1 1 569±539 5.5±2.0 对照组 53 34(64.2) 19(35.8) 22(41.5) 30.3±3.5 1 564±699 5.5±2.3 统计量 0.410a 0.329a 0.229b 0.039b 0.064b P值 0.522 0.566 0.819 0.969 0.949 注:a为χ2值,b为t值。 表 2 2组早产儿气管插管定位相关指标比较
Table 2. Comparison of tracheal intubation localization related indexes between the two groups
组别 例数 定位时间(x±s,s) 误入食管[例(%)] 误入主支气管[例(%)] 脱管[例(%)] 定位适宜[例(%)] 超声组 50 33.0±7.7 2(4.0) 3(6.0) 2(4.0) 43(86.0) 对照组 53 46.8±7.6 4(7.5) 11(20.8) 9(17.0) 29(54.7) 统计量 -9.130a 0.121b 4.769b 4.545b 11.968b P值 < 0.001 0.728 0.029 0.033 0.001 注:a为t值,b为χ2值。 表 3 2组评估气管插管定位效果评价
Table 3. The effect of tracheal intubation localization was evaluated in two groups
组别 例数 灵敏度(%) 特异度(%) 约登指数(%) 阳性似然比 阴性似然比 Kappa一致性系数 超声组 50 91.1 80.0 71.1 4.56 0.11 0.561a 对照组 53 88.9 11.8 6.5 1.01 0.94 0.008b 注:与金标准比较,aP < 0.001,bP=0.944。 -
[1] MITRA A, GAVE A, COOLAHAN K, et al. Confirmation of endotracheal tube placement using disposable fiberoptic bronchoscopy in the emergent setting[J]. World J Emerg Med, 2019, 10(4): 210-214. doi: 10.5847/wjem.j.1920-8642.2019.04.003 [2] 邵肖梅, 叶鸿瑁, 丘小汕. 实用新生儿学[M]. 5版. 北京: 人民卫生出版社, 2019: 1063-1064.SHAO X M, YE H M, QIU X S. Practical Neonatology[M]. 5th Ed. Beijing: People's Medical Publishing House, 2019: 1063-1064. [3] 刘敬, 曹海英, 程秀永. 新生儿肺脏疾病超声诊断学[M]. 郑州: 河南科学技术出版社, 2019: 239-242.LIU J, CAO H Y, CHENG X Y. Ultrasound diagnosis of neonatal pulmonary diseases[M]. Zhengzhou: Henan Science and Technology Press, 2019: 239-242. [4] 刘大为, 王小亭. 重症超声[M]. 北京: 人民卫生出版社, 2017: 272-278.LIU D W, WANG X T. Severe ultrasonic[M]. Beijing: People's Medical Publishing House, 2017: 272-278. [5] SHARMA D, TABATABAⅡ S A, FARAHBAKHSH N. Role of ultrasound in confirmation of endotracheal tube in neonates: A review[J]. J Matern Fetal Neonatal Med, 2019, 32(8): 1359-1367. doi: 10.1080/14767058.2017.1403581 [6] 陈旭, 章蔚, 夏敏, 等. 超声测量舌骨-会厌距离对喉镜显露困难的预测价值[J]. 临床麻醉学杂志, 2021, 37(6): 621-624. https://www.cnki.com.cn/Article/CJFDTOTAL-LCMZ202106014.htmCHEN X, ZANG W, XIA M, et al. Predictive value of the distance from hyoid to epiglottis measured by ultrasound in difficult laryngoscopy[J]. Journal of Clinical Anesthesiology, 2021, 37(6): 621-624. https://www.cnki.com.cn/Article/CJFDTOTAL-LCMZ202106014.htm [7] 章勤, 宋长春, 邹琪, 等. 改良经口气管插管固定法对ICU患者口面颈部器械性压力损伤的效果观察[J]. 中华全科医学, 2020, 18(8): 1421-1424. doi: 10.16766/j.cnki.issn.1674-4152.001522ZANG Q, SONG C C, ZOU Q. Observation on the clinical effect of modified oral endotracheal intubation method on ICU patients with instrumental pressure injury[J]. Chinese Journal of General Practice, 2020, 18(8): 1421-1424. doi: 10.16766/j.cnki.issn.1674-4152.001522 [8] RAMASWAMY V V, ABIRAMALATHA T, BANDYOPADHYAY T, et al. Digital tracheal intubation and finger palpation to confirm endotracheal tube tip position in neonates: A systematic review and meta-analysis[J]. Pediatr Pulmonol, 2021, 56(9): 2893-2902. doi: 10.1002/ppul.25551 [9] 刘娜, 李鹏, 王惠萍, 等. 床旁超声与移动DR在新生儿重症监护室的应用比较[J]. 中国临床医学影像杂志, 2019, 30(4): 281-285. https://www.cnki.com.cn/Article/CJFDTOTAL-LYYX201904015.htmLIU N, LI P, WANG H P. A comparison of application of bedside ultrasound and mobile digital radiography in neonatal intensive care unit[J]. Journal of China Clinic Medical Imaging, 2019, 30(4): 281-285. https://www.cnki.com.cn/Article/CJFDTOTAL-LYYX201904015.htm [10] 高山, 张永. 床边下腔静脉超声指标及中心静脉压对脓毒性休克患者容量反应性的预测价值[J]. 中华全科医学, 2021, 19(4): 581-585. doi: 10.16766/j.cnki.issn.1674-4152.001866GAO S, ZHANG Y. The predictive value of variation index of inferior vena cava measured by ultrasonography and central venous pressure in volume responsiveness in patients with septic shock[J]. Chinese Journal of General Practice, 2021, 19(4): 581-585. doi: 10.16766/j.cnki.issn.1674-4152.001866 [11] 左莉莉, 任义梅, 周洁, 等. 超声引导在极低/超低出生体重儿经外周中心静脉置管中的应用[J]. 中华新生儿科杂志, 2021, 36(5): 20-23.ZUO L L, REN Y M, ZHOU J, et al. Application of ultrasound-guided peripherally inserted central catheter in very/extremely low birth weight infants[J]. Chinese Journal of Neonatology, 2021, 36(5): 20-23. [12] 徐朴, 陈美银, 万宗明, 等. 超声定位引导在声门显露困难患者气管插管中的应用[J]. 川北医学院学报, 2020, 35(2): 301-304. https://www.cnki.com.cn/Article/CJFDTOTAL-NOTH202002032.htmXU P, CHEN M Y, WAN Z M, et al. Clinical study of ultrasound guided in locating endotracheal intubation in patients with difficult glottis exposure[J]. Journal of North Sichuan Medical College, 2020, 35(2): 301-304. https://www.cnki.com.cn/Article/CJFDTOTAL-NOTH202002032.htm [13] CHELLEN S, MIALL L. In neonates who have been successfully intubated can ultrasound be used to accurately confirm endotracheal tube tip position?[J]. Arch Dis Child, 2021. DOI: 10.1136/archdischild-2021-323146. [14] GUERDER M, MAURIN O, MERCKX A, et al. Diagnostic value of pleuralultrasound to refine endotracheal tube placement in pediatric intensive care unit[J]. Arch Pediatr, 2021, 28(8): 712-717. [15] SAHU A K, BHOI S, AGGARWAL P, et al. Endotracheal tube placement confirmation by ultrasonography: A systematic review and meta-analysis of more than 2500 patients[J]. J Emerg Med, 2020, 59(2): 254-264. [16] JOYCE M, TOZER J, VITTO M, et al. Ability of critical care medics to confirm endotracheal tube placement by ultrasound[J]. Prehosp Disaster Med, 2020, 35(6): 629-631. [17] 黄磊, 第加美, 邹宝, 等. 超声引导与盲穿行中心静脉置管的临床效果比较[J]. 中华全科医学, 2021, 19(6): 940-943. doi: 10.16766/j.cnki.issn.1674-4152.001955HUANG L, DI M J, ZOU B, et al. Retrospective analysis of ultrasound-guided and blind central vein catheterisation[J]. Chinese Journal of General Practice, 2021, 19(6): 940-943. doi: 10.16766/j.cnki.issn.1674-4152.001955 [18] 李秀燕, 方桂珍, 王兰芳, 等. 改良超声引导下桡动脉穿刺置管技术在ICU休克患者中的临床研究[J]. 中华全科医学, 2017, 15(5): 748-751, 837. doi: 10.16766/j.cnki.issn.1674-4152.2017.05.006LI X Y, FANG G Z, WANG L F, et al. Transradial catheterization guided by improved ultrasonic technology for shock patients in ICU[J]. Chinese Journal of General Practice, 2017, 15(5): 748-751, 837. doi: 10.16766/j.cnki.issn.1674-4152.2017.05.006 [19] DAGGUPATI H, MAURYA I, SINGH R D, et al. Development of a scoring system for predicting difficult intubation using ultrasonography[J]. Indian J Anaesth, 2020, 64(3): 187-192. [20] 苏相飞, 彭书峻, 杜素娟, 等. 超声测定小儿环状软骨横径用于带套囊气管导管型号选择的准确性[J]. 中华麻醉学杂志, 2017, 37(7): 784-787.SU X F, PENG S J, DU X J, et al. Accuracy of ultrasonographic measurement of transverse diameter of cricoid cartilage in selecting cuffed endotracheal tube size for pediatric patients[J]. Chinese Journal of Anesthesilolgy, 2017, 37(7): 784-787. -





 下载:
下载: