Expression of interleukin-23 in carcinoma tissues and its relationship with clinical prognosis in patients with colorectal cancer
-
摘要:
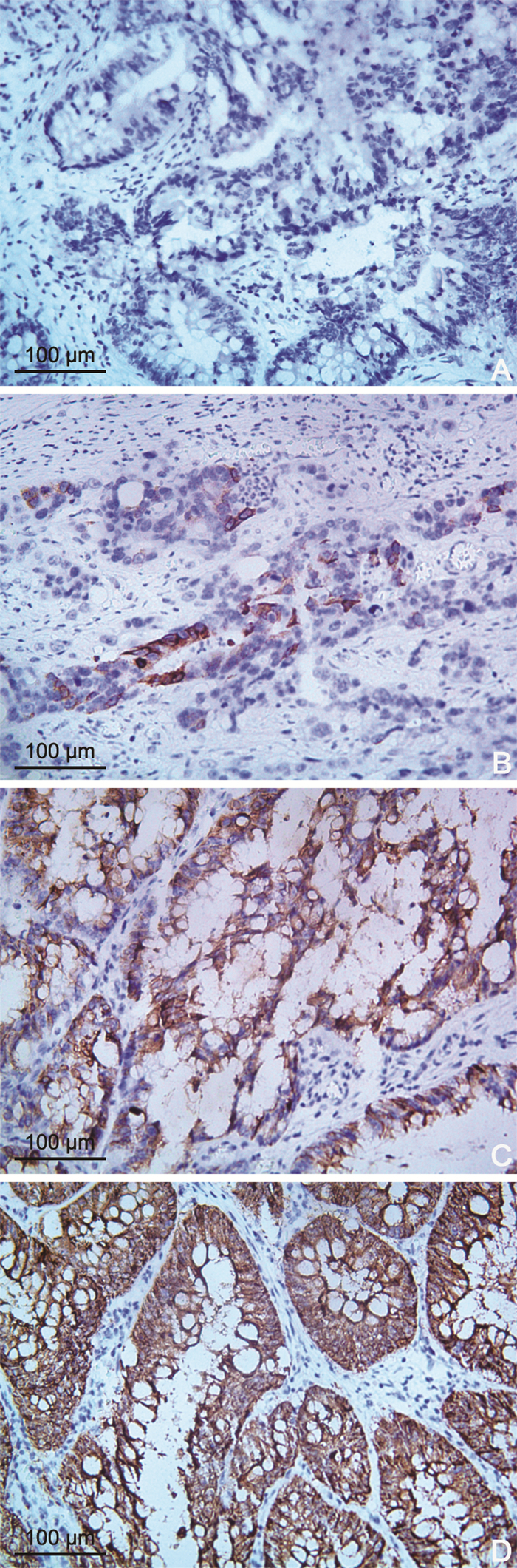
目的 探讨结直肠癌患者癌组织中IL-23表达水平与预后的关系。 方法 选取2015年1月1日—2016年12月31日于南阳市中心医院就诊的164例结直肠癌患者并采用免疫组化法检测癌组织中IL-23的表达,染色强度得分×阳性表达率得分为0~1分、2~3分、4~5分和≥6分时分别计为阴性、弱阳性、中度阳性和强阳性,将“中度和强度阳性”视为IL-23高表达,其余为IL-23低表达;纳入2019年1月1日—2019年12月31日南阳市中心医院70例结直肠癌患者(观察组)和35例健康者(对照组),比较血清中IL-23表达的差异。影响因素和诊断效能用Cox风险比例模型和受试者操作特征曲线分析。 结果 癌组织中IL-23高表达119例,低表达45例,主要表达于胞浆中。淋巴结转移(N1~N2)、TNM分期(Ⅲ期)和IL-23表达水平(高表达)是CRC患者预后的独立危险因素(均P < 0.01)。结直肠癌观察组血清中IL-23表达显著高于对照组(t=12.173,P < 0.001)。IL-23诊断结直肠癌的AUC为0.935(95% CI:0.888~0.981),截断值为36.195 ng/mL,诊断灵敏度和特异度为94.30%和80.00%。 结论 IL-23高表达与结直肠癌不良预后有关,可作为预测预后的一项血清学筛查标志物。 Abstract:Objective To investigate the association between interleukin-23 (IL-23) and colorectal cancer. Methods A total of 164 patients with colorectal cancer from January 1, 2015, to December 31, 2016, in Nanyang Central Hospital were enrolled. The expression of IL-23 in the carcinoma tissues of patients with colorectal cancer was detected by immunohistochemical methods. In accordance with the staining intensity score and positive cell count score, the 0-1, 2-3, 4-5 and ≥6 scores were defined as negative, weak positive, moderate positive and strong positive, respectively. The high and low expression of IL-23 in the carcinoma tissues of colorectal cancer in paraffin-embedded section were regarded as "moderate to strong positive" and "negative to positive", respectively. Another 70 patients with colorectal cancer and 35 normal individuals between January 1, 2019, and December 31, 2019, were enrolled as independent verification samples and the difference in the IL-23 expression in the serum of the two groups was compared. The influencing factors of postoperative recurrence in patients with colorectal cancer were analysed by Cox regression model and the clinical efficacy of serum IL-23 expression levels in the diagnosis of colorectal cancer was analysed by receiver operating characteristic (ROC) curve. Results In all colorectal cancer patients, there were 119 cases with high expression of IL-23 and the remaing with low expression of IL-23. The IL-23 were mostly expressed in the cytoplasm of cells. The lymph node metastasis (N1-N2), TNM stage (stage Ⅲ) and IL-23 expression (high expression) were independent risk factors affecting the prognosis of patients with CRC (P < 0.01).Compared with the control group, the serum expression level of IL-23 in the colorectal cancer experimental group was significantly increased (t=12.173, P < 0.001). ROC curve results showed that the AUC of IL-23 in the diagnosis of colorectal cancer was 0.935 (95% CI: 0.888-0.981). When the cut-off value was 36.195 ng/mL, the diagnostic sensitivity and specificity were 94.30% and 80.00%, respectively. Conclusion High expression of IL-23 is significantly associated with poor prognosis in patients with colorectal cancer. IL-23 could be used as a serological marker of CRC. -
Key words:
- Colorectal cancer /
- Interleukin-23 /
- Inflammation /
- Prognosis /
- ROC curve
-
表 1 结直肠癌患者癌组织中IL-23表达水平与临床-病理特征的关系(例)
Table 1. IL-23 expression in colorectal cancer patients with carcinoma tissue level relationship with the clinical, pathological features (cases)
项目 IL-23低表达组(n=45) IL-23高表达组(n=119) χ2值 P值 性别 2.726 0.099 男性 20 70 女性 25 49 年龄 0.355 0.551 ≥60岁 23 67 < 60岁 22 52 肿瘤部位 2.588 0.108 直肠 29 60 结肠 16 59 肿瘤大小 0.384 0.536 ≥5 cm 18 54 < 5 cm 27 65 肿瘤细胞分化程度 19.713 < 0.001 高分化 29 32 中~低分化 16 87 淋巴结转移 6.276 0.012 N0 26 43 N1~N2 19 76 TNM分期 10.579 0.001 Ⅰ~Ⅱ 37 65 Ⅲ 8 54 CEA 0.481 0.488 阳性 23 68 阴性 22 51 CA19-9 2.726 0.099 阳性 25 49 阴性 20 70 表 2 变量赋值方法
Table 2. Variable assignment method
变量 赋值方法 性别 男性=1;女性=0 年龄 ≥60岁=1; < 60岁=0 肿瘤部位 结肠=1;直肠=0 肿瘤大小 ≥5 cm=1; < 5 cm=0 肿瘤细胞分化程度 中~低分化=1;高分化=0 淋巴结转移 N1~N2=1;N0=0 TNM分期 Ⅲ期=1;Ⅰ~Ⅱ期=0 CEA CEA阳性=1CEA阴性=0 CA19-9 CA19-9阳性=1CA19-9阴性=0 IL-23 IL-23高表达=1;IL-23低表达=0 表 3 结直肠癌患者复发的多因素Cox比例风险回归模型分析
Table 3. Multivariate Cox proportional hazards regression model analysis of colorectal cancer recurrence
变量 B SE Wald χ2 HR值 95% CI P值 淋巴结转移(N1~N2) 0.697 0.254 7.530 2.007 1.367~5.119 < 0.001 TNM分期(Ⅲ期) 0.997 0.381 6.848 2.711 1.327~5.379 < 0.001 IL-23表达情况(高表达) 1.045 0.467 5.007 2.843 1.612~5.127 < 0.001 -
[1] ZHU J, TAN Z, HOLLIS-HANSEN K, et al. Epidemiological trends in colorectal cancer in China: An ecological study[J]. Dig Dis Sci, 2017, 62(1): 235-243. doi: 10.1007/s10620-016-4362-4 [2] DEKKER E, TANIS P J, VLEUGELS J L A, et al. Colorectal cancer[J]. Lancet, 2019, 394(10207): 1467-1480. doi: 10.1016/S0140-6736(19)32319-0 [3] GAO R, GAO Z, HUANG L, et al. Gut microbiota and colorectal cancer[J]. Eur J Clin Microbiol Infect Dis, 2017, 36(5): 757-769. doi: 10.1007/s10096-016-2881-8 [4] WROBEL P, AHMED S. Current status of immunotherapy in metastatic colorectal cancer[J]. Int J Colorectal Dis, 2019, 34(1): 13-25. doi: 10.1007/s00384-018-3202-8 [5] TUOMISTO A E, MÄKINEN M J, VÄYRYNEN J P. Systemic inflammation in colorectal cancer: Underlying factors, effects, and prognostic significance[J]. World J Gastroenterol, 2019, 25(31): 4383-4404. doi: 10.3748/wjg.v25.i31.4383 [6] SHAWKI S, ASHBURN J, SIGNS S A, et al. Colon cancer: Inflammation-associated cancer[J]. Surg Oncol Clin N Am, 2018, 27(2): 269-287. doi: 10.1016/j.soc.2017.11.003 [7] ZHU G, CHENG Z, LIN C, et al. MyD88 regulates LPS-induced NF-κB/MAPK cytokines and promotes inflammation and malignancy in colorectal cancer cells[J]. Cancer Genomics Proteomics, 2019, 16(6): 409-419. doi: 10.21873/cgp.20145 [8] SUZUKI Y, OKABAYASHI K, HASEGAWA H, et al. Comparison of preoperative inflammation-based prognostic scores in patients with colorectal cancer[J]. Ann Surg, 2018, 267(3): 527-531. doi: 10.1097/SLA.0000000000002115 [9] YAN J, SMYTH M J, TENG M W L. Interleukin (IL)-12 and IL-23 and their conflicting roles in cancer[J]. Cold Spring Harb Perspect Biol, 2018, 10(7): a028530. DOI: 10.1101/cshperspect.a028530. [10] WANG J J, LEI K F, HAN F. Tumor microenvironment: Recent advances in various cancer treatments[J]. Eur Rev Med Pharmacol Sci, 2018, 22(12): 3855-3864. [11] VITALE I, MANIC G, COUSSENS L M, et al. Macrophages and metabolism in the tumor microenvironment[J]. Cell Metab, 2019, 30(1): 36-50. doi: 10.1016/j.cmet.2019.06.001 [12] 牛玉苗, 严翔, 齐宏妍, 等. 肿瘤微环境中主要炎症细胞因子对PD-L1表达调控的研究进展[J]. 中国病理生理杂志, 2020, 36(9): 1704-1708. doi: 10.3969/j.issn.1000-4718.2020.09.024NIU Y M, YAN X, QI H Y, et al. Progress on regulation of PD-L1 expression by major inflammatory cytokines in tumor microenvironment[J]. Chinese Journal of Pathophysiology, 2020, 36(9): 1704-1708. doi: 10.3969/j.issn.1000-4718.2020.09.024 [13] SINGH N, BABY D, RAJGURU J P, et al. Inflammation and cancer[J]. Ann Afr Med, 2019, 18(3): 121-126. doi: 10.4103/aam.aam_56_18 [14] 张小聪, 陈小伍, 朱达坚. IL-23与结直肠癌发生及发展的研究进展[J]. 医学理论与实践, 2017, 30(23): 3475-3477. https://www.cnki.com.cn/Article/CJFDTOTAL-YXLL201723011.htmZHANG X C, CHEN X W, ZHU D J. Research progress of IL-23 and the genesis and development of colorectal cancer[J]. The Journal of Medical Theory and Practice, 2017, 30(23): 3475-3477. https://www.cnki.com.cn/Article/CJFDTOTAL-YXLL201723011.htm [15] TAMASSIA N, ARRUDA-SILVA F, WRIGHT H L, et al. Human neutrophils activated via TLR8 promote Th17 polarization through IL-23[J]. J Leukoc Biol, 2019, 105(6): 1155-1165. doi: 10.1002/JLB.MA0818-308R [16] HURTADO C G, WAN F, HOUSSEAU F, et al. Roles for interleukin 17 and adaptive immunity in pathogenesis of colorectal cancer[J]. Gastroenterology, 2018, 155(6): 1706-1715. doi: 10.1053/j.gastro.2018.08.056 [17] LIM K S, YONG Z W E, WANG H, et al. Inflammatory and mitogenic signals drive interleukin 23 subunit alpha (IL23A) secretion independent of IL12B in intestinal epithelial cells[J]. J Biol Chem, 2020, 295(19): 6387-6400. doi: 10.1074/jbc.RA120.012943 [18] CHEN J, ZHU Z, LI Q, et al. Neutrophils enhance cutaneous vascular dilation and permeability to aggravate psoriasis by releasing matrix metallopeptidase 9[J]. J Invest Dermatol, 2021, 141(4): 787-799. doi: 10.1016/j.jid.2020.07.028 [19] KHABBAZI S, HASSANSHAHI M, HASSANSHAHI A, et al. Opioids and matrix metalloproteinases: The influence of morphine on MMP-9 production and cancer progression[J]. Naunyn Schmiedebergs Arch Pharmacol, 2019, 392(2): 123-133. doi: 10.1007/s00210-019-01613-6 [20] ELESSAWI D F, ALKADY M M, IBRAHIM I M. Diagnostic and prognostic value of serum IL-23 in colorectal cancer[J]. Arab J Gastroenterol, 2019, 20(2): 65-68. doi: 10.1016/j.ajg.2019.05.002 [21] 赖志亨, 邹江. LINC00261和miR-522-3p在结直肠癌中的表达及其与患者预后的关系[J]. 国际检验医学杂志, 2021, 42(8): 991-995. doi: 10.3969/j.issn.1673-4130.2021.08.023LAI Z H ZOU J. Expression of LINC00261 and miR-522-3p and their relationship with prognosis in colorectal cancer patients[J]. International Journal of Laboratory Medicine, 2021, 42(8): 991-995. doi: 10.3969/j.issn.1673-4130.2021.08.023 [22] 潘丽, 孙国平. 结直肠癌根治术后复发危险因素分层分析[J]. 中华肿瘤防治杂志, 2018, 25(4): 270-274. https://www.cnki.com.cn/Article/CJFDTOTAL-QLZL201804009.htmPAN L, SUN G P. Risk stratification analysis of recurrence after radical resection of colorectal cancer[J]. Chinese Journal of Cancer Prevention and Treatment, 2018, 25(4): 270-274. https://www.cnki.com.cn/Article/CJFDTOTAL-QLZL201804009.htm -





 下载:
下载: