Effect of NLR and PLR from pre-radiotherapy on prognosis of locally advanced nasopharyngeal carcinoma patients
-
摘要:
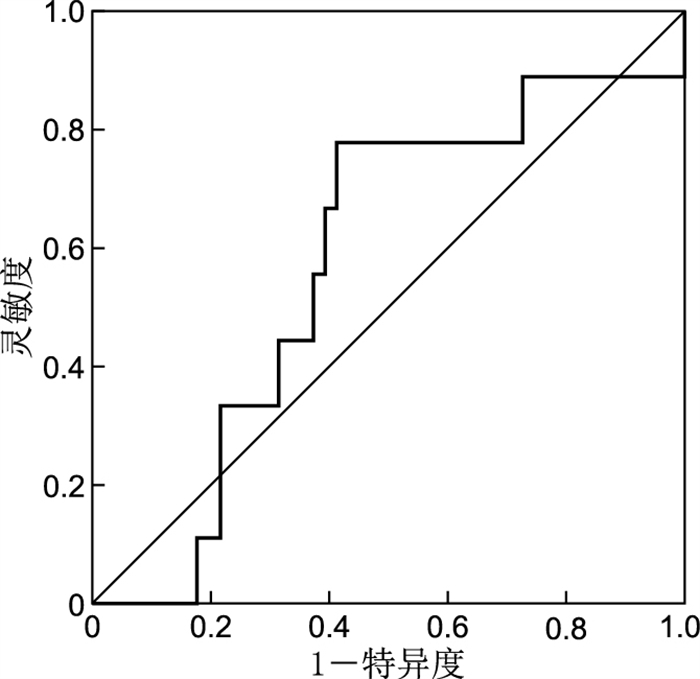
目的 探讨放疗前血液中性粒细胞与淋巴细胞比值(neutrophil-to-lymphocyte ratio,NLR)及血小板与淋巴细胞比值(platelet-lymphocyte ratio,PLR)与局部晚期鼻咽癌放疗患者预后的相关性。 方法 回顾性分析2016年1月—2018年12月在中国科学技术大学附属第一医院头颈放疗科行放化疗的60例局部晚期鼻咽癌患者临床资料及随访资料,采用ROC曲线确定NLR和PLR的最佳截断值,并据此分为高水平组和低水平组。采用χ2检验或Fisher精确检验比较组间差异,使用Kaplan-Meier法绘制生存曲线,采用Cox回归模型进行多因素分析。 结果 依据ROC曲线,放疗前NLR和PLR的最佳截取值分别为1.99、154.94。在单因素分析中N分期、临床分期、放疗前NLR及PLR与患者预后相关(均P<0.05);放疗前低NLR组的生存时间为(62.26±1.88)个月,优于放疗前高NLR组[(51.17±3.94)个月,P=0.048];相较于放疗前高PLR组,放疗前低PLR组生存时间更长(P=0.014);而Cox多因素分析中临床分期、N分期、放疗前PLR水平是影响局部晚期鼻咽癌患者生存的独立预后因素(均P<0.05)。 结论 放疗前PLR水平可作为局部晚期鼻咽癌放疗患者独立预后预测因子,推荐其作为辅助手段参与患者预后评估。 -
关键词:
- 局部晚期鼻咽癌 /
- 中性粒细胞与淋巴细胞比值 /
- 血小板与淋巴细胞比值 /
- 预后
Abstract:Objective To explore the correlation between neutrophil-to-lymphocyte ratio (NLR) and platelet-lymphocyte ratio (PLR) and the prognosis of patients with locally advanced nasopharyngeal carcinoma undergoing radiotherapy. Methods We retrospectively analysed the clinical data and follow-up data of 60 patients with locally advanced nasopharyngeal carcinoma who underwent radiotherapy and chemotherapy from January 2016 to December 2018. An ROC curve was used to determine NLR and PLR. According to the best cutoff value, patients were divided into high-and low-level groups. Chi-square or Fisher exact test was used to compare the differences between groups. Kaplan-Meier method was used to draw survival curve. Cox regression model was used for univariate and multivariate analysis. Results According to the ROC curve, the best cutoff values of NLR and PLR before radiotherapy were 1.99 and 154.94, respectively. In univariate analysis, N stage, clinical stage, pre-radiotherapy NLR and PLR were related to patient prognosis (all P < 0.05). The average survival time of the low pre-radiotherapy NLR group was (62.26±1.88) months, which was better than that of the high NLR group of (51.17±3.94) months (P=0.048). Compared with the high pre-radiotherapy PLR group, the average survival time of the low PLR group was longer (P=0.014). Cox multivariate analysis showed that clinical stage, N stage, and pre-radiotherapy PLR level were independent prognostic factors for patient survival (all P < 0.05). Conclusion PLR before radiotherapy could be used as an independent prognostic predictor for patients with locally advanced nasopharyngeal carcinoma undergoing radiotherapy. It is recommended as an auxiliary method for evaluating the prognosis of patients. -
表 1 放疗前NLR与局部晚期鼻咽癌患者临床特征的关系
Table 1. Relationship between NLR and clinical characteristics of patients with locally advanced nasopharyngeal carcinoma before radiotherapy
组别 例数 性别[例(%)] 年龄(x±s, 岁) T分期[例(%)] N分期[例(%)] 临床分期[例(%)] EB-PCR[例(%)] 男性 女性 T2 T3~4 N0~N2 N3 Ⅲ期 Ⅳa+Ⅳb期 阴性 阳性 高NLR组 29 23(79.3) 6(20.7) 52.07±11.17 2(6.9) 27(93.1) 26(89.7) 3(10.3) 14(48.3) 15(51.7) 18(62.1) 11(37.9) 低NLR组 31 21(67.7) 10(32.3) 48.36±10.93 7(22.6) 24(77.4) 25(80.6) 6(19.4) 20(64.5) 11(35.5) 22(71.0) 9(29.0) 统计量 1.025a 0.065b 3.547a 0.954a 1.609a 0.534a P值 0.311 0.800 0.199 0.474 0.157 0.324 注:a为χ2值,b为t值。 表 2 放疗前PLR与局部晚期鼻咽癌患者临床特征的关系
Table 2. Relationship between PLR and clinical features in patients with locally advanced nasopharyngeal carcinoma before radiotherapy
组别 例数 性别[例(%)] 年龄(x±s, 岁) T分期[例(%)] N分期[例(%)] 临床分期[例(%)] EB-PCR[例(%)] 男性 女性 T2 T3~4 N0~N2 N3 Ⅲ期 Ⅳa+Ⅳb期 阴性 阳性 高PLR组 10 6(60.0) 4(40.0) 53.90±8.67 2(20.0) 8(80.0) 8(80.0) 2(20.0) 3(30.0) 7(70.0) 8(80.0) 2(20.0) 低PLR组 50 38(76.0) 12(24.0) 49.40±11.48 7(14.0) 43(86.0) 43(86.0) 7(14.0) 31(62.0) 19(38.0) 32(64.0) 18(36.0) 统计量 1.091a 0.655b 2.290a 0.235a 3.475a 0.960a P值 0.433 0.422 0.254 0.637 0.085 0.471 注:a为χ2值,b为t值。 表 3 影响局部晚期鼻咽癌患者预后的单因素分析
Table 3. Univariate analysis of prognosis in patients with locally advanced nasopharyngeal carcinoma
项目 例数 生存时间(x±s, 月) 5年生存率(%) Wald χ2 P值 性别 0.188 0.664 男性 44 56.36±2.55 86.4 女性 16 56.38±4.52 81.3 年龄 1.307 0.253 < 50岁 30 60.53±2.45 90.0 ≥50岁 30 53.13±3.64 80.0 T分期 0.165 0.685 T2 9 55.11±3.67 88.9 T3~4 51 57.14±2.58 84.3 N分期 8.288 0.004 N0~N2 51 60.31±2.00 90.2 N3 9 40.78±8.12 55.6 临床分期 5.138 0.023 Ⅲ期 34 62.24±1.90 94.1 Ⅳa+Ⅳb期 26 50.15±4.22 73.1 EB-PCR 0.527 0.468 阴性 40 56.15±2.46 87.5 阳性 20 55.35±4.39 80.0 放疗前NLR 3.912 0.048 低NLR组 31 62.26±1.88 93.5 高NLR组 29 51.17±3.94 75.9 放疗前PLR 5.985 0.014 低 10 60.20±2.13 90.0 高 50 36.10±5.21 60.0 表 4 影响局部晚期鼻咽癌患者预后的多因素Cox回归分析
Table 4. Multivariate Cox regression analysis of prognostic factors in patients with locally advanced nasopharyngeal carcinoma
变量 B SE Wald χ2 P值 HR 95% CI 临床分期 -1.458 0.668 4.770 0.029 0.233 0.063~0.861 N分期 -1.252 0.621 4.066 0.044 0.286 0.085~0.966 放疗前NLR -1.453 0.802 3.279 0.070 0.234 0.049~1.127 放疗前PLR -1.680 0.617 7.048 0.006 0.186 0.056~0.625 注:各变量赋值方法,临床分期,Ⅲ期=1,Ⅳa+Ⅳb期=2;N分期,N0~N2期=1,N3期=2;NLR、PLR均以实际值赋值。 -
[1] YANG L P, GAO J, ZHOU Y, et al. Prognostic value of the albumin-to-alkaline phosphatase ratio before chemoradiotherapy in patients with nonmetastatic nasopharyngeal carcinoma[J]. Chemotherapy, 2021, 66(1-2): 40-46. doi: 10.1159/000513058 [2] SUN X S, LIANG Y J, LIU S L, et al. Subdivision of nasopharyngeal carcinoma patients with bone-only metastasis at diagnosis for prediction of survival and treatment guidance[J]. Cancer Res Treat, 2019, 51(4): 1259-1268. doi: 10.4143/crt.2018.652 [3] LIU S L, SUN X S, LU Z J, et al. Nomogram predicting the benefits of adding concurrent chemotherapy to intensity-modulated radiotherapy after induction chemotherapy in Stages Ⅱ-Ⅳb nasopharyngeal carcinoma[J]. Front Oncol, 2020, 9(10): 539321. DOI: 10.3389/fonc.2020.539321. [4] QIU W Z, KE L R, XIA W X, et al. A retrospective study of 606 cases of nasopharyngeal carcinoma with or without oropharyngeal candidiasis during radiotherapy[J]. PLoS One, 2017, 12(8): e0182963. DOI: 10.1371/journal.pone.0182963. [5] XIANG Z J, HU T, WANG Y, et al. Neutrophil-lymphocyte ratio (NLR) was associated with prognosis and immunomodulatory in patients with pancreatic ductal adenocarcinoma (PDAC)[J]. Biosci Rep, 2020, 40(6): BSR20201190. DOI: 10.1042/BSR20201190. [6] 刘建辉, 罗妍, 陈晓, 等. 放疗前中性粒细胞/淋巴细胞血小板/淋巴细胞预后营养指数及CA199与胰腺腺癌放疗后预后关系的分析[J]. 中国肿瘤临床, 2017, 44(6): 289-293. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGZL201706011.htmLIU J H, LUO Y, CHEN X, et al. Pre-radiation neutrophil to lymphocyte ratio, platelet to lymphocyte ratio, prognostic nutritional index, and CA19-9 as prognostic factors in pancreatic cancer patients treated with radiotherapy[J]. Chinese Journal of Clinical Oncology, 2017, 44(6): 289-293. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGZL201706011.htm [7] 汪庚明, 周燕, 孙谦, 等. 局部晚期下咽癌患者放疗前NLR与PLR对预后的意义[J]. 中华全科医学, 2021, 19(5): 763-766. doi: 10.16766/j.cnki.issn.1674-4152.001911WANG G M, ZHOU Y, SUN Q, et al. Prognostic value of pretreatment neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio in patients with locally advanced hypopharyngeal cancer treated with radiation[J]. Chinese Journal of General Practice, 2021, 19(5): 763-766. doi: 10.16766/j.cnki.issn.1674-4152.001911 [8] 郭苗, 刘玮, 李伟. FIB、NLR、PLR联合检测在非小细胞肺癌早期诊断及预后评估中的价值[J]. 海南医学, 2020, 31(15): 1954-1957. https://www.cnki.com.cn/Article/CJFDTOTAL-HAIN202015014.htmGUO M, LIU W, LI W. Value of combined detection with FIB, NLR, and PLR in the early diagnosis and prognosis evaluation of non-small cell lung cancer[J]. Hainan Medical Journal, 2020, 31(15): 1954-1957. https://www.cnki.com.cn/Article/CJFDTOTAL-HAIN202015014.htm [9] 杨洁, 王晨, 徐庆春, 等. 结直肠癌患者术前NLR、PLR、PDW与其预后的关系[J]. 山东医药, 2018, 58(24): 61-63. https://www.cnki.com.cn/Article/CJFDTOTAL-SDYY201824018.htmYANG J, WANG C, XU Q C, et al. Relationship between preoperative NLR, PLR, PDW and prognosis in patients with colorectal cancer[J]. Shandong Medical Journal, 2018, 58(24): 61-63. https://www.cnki.com.cn/Article/CJFDTOTAL-SDYY201824018.htm [10] XIA Z F, HU D F, XIONG H C, et al. Benefit of chemotherapy in stage Ⅲ nasopharyngeal carcinoma: Analysis of the surveillance, epidemiology, and end results database[J]. Oral Oncol, 2021, 117: 105284. DOI: 10.1016/j.oraloncology.2021.105284. [11] LI X, GAO Y, XU Z, et al. Identification of prognostic genes in adrenocortical carcinoma microenviron-ment based on bioinformatic methods[J]. Cancer Med, 2020, 9(3): 1161-1172. doi: 10.1002/cam4.2774 [12] WANG D, BAI N, HU X, et al. Preoperative inflammatory markers of NLR and PLR as indicators of poor prognosis in resectable HCC[J]. PeerJ, 2019, 7: e7132. DOI: 10.7717/peerj.7132. [13] GUO W Y, LU X, LIU Q P, et al. Prognostic value of neutrophil-to-lymphocyte ratio and plateletto-lymphocyte ratio for breast cancer patients: An updated meta-analysis of 17079 individuals[J]. Cancer Med, 2019, 8(9): 4135-4148. doi: 10.1002/cam4.2281 [14] LIU C X, LI X L. Stage-dependent changes in albumin, NLR, PLR, and AFR are correlated with shorter survival in patients with gastric cancer[J]. Clin Lab, 2019, 65(9): e31532095. DOI: 10.7754/Clin.Lab.2019.190132. [15] CHEN C J, YANG H T, CAI D, et al. Preoperative peripheral blood neutrophil-to-lymphocyte ratios (NLR)and platelet-to-lymphocyte ratio (PLR) related nomograms predict the survival of patients with limited-stage small-cell lung cancer[J]. Transl Lung Cancer Res, 2021, 10(2): 866-877. doi: 10.21037/tlcr-20-997 [16] MECHTELD C, RADU MH, SHAHAB K H. Neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR) as possible prognostic markers for patients undergoing resection of adrenocortical carcinoma[J]. World J Surg, 2021, 45(3): 754-764. [17] 金龙, 付神波, 于娇. 治疗前PLR和NLR对鼻咽癌患者预后的影响[J]. 肿瘤防治研究, 2017, 44(7): 476-480. https://www.cnki.com.cn/Article/CJFDTOTAL-ZLFY201707006.htmJIN L, FU S B, YU J. Effect of NLR and PLR from pre-treatment on prognosis of nasopharyngeal carcinoma patients[J]. Cancer Research on Prevention and Treatment, 2017, 44(7): 476-480. https://www.cnki.com.cn/Article/CJFDTOTAL-ZLFY201707006.htm [18] 张东成, 汪浩. NLR/PA、NLR/Alb和NLR在食管鳞癌根治性放疗近期疗效预测中的价值[J]. 山东医药, 2020, 60(25): 66-68. https://www.cnki.com.cn/Article/CJFDTOTAL-SDYY202025018.htmZHANG D C, WANG H. Value of NLR/PA, NLR/Alb and NLR in predicting short-term response to radical radiotherapy for esophageal squamous cell carcinoma[J]. Shandong Medical Journal, 2020, 60(25): 66-68. https://www.cnki.com.cn/Article/CJFDTOTAL-SDYY202025018.htm [19] SILVA R N F, DALLARMI L B, ARAUJO A K C, et al. Immunohisto-chemical analysis of neutrophils, interleukin-17, matrix metal-loproteinase-9, and new formed vessels in oral squamous cellcarcinoma[J]. J Oral Pathol Med, 2018, 47(9): 856-863. [20] LI Z L, QU Y, YANG Y, et al. Prognostic value of the neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio and systemic immune-inflammation index in patients with laryngeal squamous cell carcinoma[J]. Clin Otolaryngol, 2021, 46(2): 395-405. [21] LU A Y, LI H F, ZHENG Y M, et al. Prognostic significance of neutrophil to lymphocyte ratio, lymphocyte to monocyte ratio, and platelet to lymphocyte ratio in patients with nasopharyngeal carcinoma[J]. Biomed Res Int, 2017, 2017: 3047802. DOI: 10.1155/2017/3047802. -





 下载:
下载: