Study on the relationship between lymphocyte subsets, cytokines and immune efficacy in advanced non-small cell lung cancer
-
摘要:
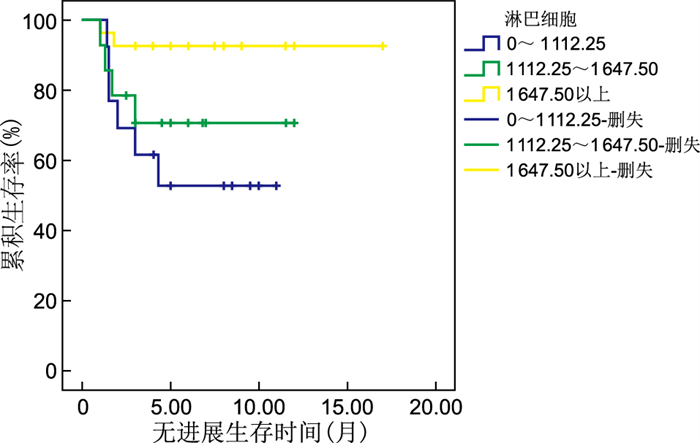
目的 免疫检查点抑制剂明显改变了非小细胞肺癌的治疗前景。PD-L1作为免疫治疗的生物标志物已广泛应用于临床,但仍存在部分缺陷,所以进一步研究血清相关标记物在临床中的预测效果是有必要的。 方法 回顾性收集河南省人民医院2019年1月—2021年6月收治的接受免疫治疗的晚期非小细胞肺癌患者48例,并于治疗前及治疗4周期后抽取空腹外周血,检测其细胞因子及淋巴细胞亚群水平。4周期后依据疗效[完全缓解(CR)、部分缓解(PR)、疾病稳定(SD)、疾病进展(PD)]将其分为控制组(CR+PR+SD,36例)和无效组(PD,12例)。比较2组间治疗后淋巴细胞亚群及细胞因子水平变化及与疗效的关系。 结果 免疫治疗4周期后控制组的淋巴细胞水平、总T淋巴细胞水平及CD4+ T淋巴细胞水平明显高于无效组[(1 648±564)μL vs. (1 098±581)μL;(1 121±388)μL vs. (651±368)μL;540(367, 799)μL vs. 245(125, 411)μL,均P<0.05]。其中T细胞计数水平与肿瘤进展呈负相关,且表达水平越高越能获得更好的无进展生存时间(PFS)。相反,细胞因子中IL-4及IL-6的高表达与肿瘤进展呈明显正相关,其表达水平越高PFS越差。 结论 淋巴细胞亚群及细胞因子的表达水平与晚期非小细胞肺癌患者的疗效密切相关,可作为晚期非小细胞肺癌免疫治疗疗效的预测因素。 Abstract:Objective Immuno-checkpoint inhibitors significantly change the treatment prospects for non-small cell lung cancer. PD-L1, as a biomarker of immunotherapy, is extensively used in clinical settings, but some defects remain in its application. This study aimed to further explore the predictive effect of serum-related markers in clinical practice. Methods We retrospectively collected 48 cases of advanced non-small cell lung cancer patients receiving immunotherapy in Henan Provincial People's Hospital from 2019 to June 2021. Fasting peripheral blood was taken before treatment and after 4 cycles of treatment to detect the levels of cytokines and lymphocyte subsets. After four cycles, according to the efficacy (complete response, CR; partial response, PR; stable disease, SD; progressive disease, PD), it was divided into a control group (CR+PR+SD) for a total of 36 cases and an ineffective group (PD) for 12 cases. The changes in level after treatment between the two groups and the relationship with efficacy were compared. Results After the four cycles of immunotherapy treatment, lymphocyte levels, total T lymphocyte levels, and CD4+ T lymphocyte levels in the control group were significantly higher than those in the ineffective group [(1 648±564) μL vs. (1 098±581) μL; (1 121±388) μL vs. (651±368) μL; 540(367, 799) μL vs. 245(125, 411) μL, all P < 0.05]. The count level of T cells was significantly negatively correlated with tumor progression, and a higher T cell expression level corresponded with better progression-free survival (PFS). Conversely, the high expression of IL-4 and IL-6 was significantly positively correlated with tumor progression, and PFS was worse. Conclusion The lymphocyte subgroups and expression levels of cytokines are closely related to the efficacy of patients with advanced non-small cell lung cancer. They can be used as predictors of the efficacy of immunotherapy for advanced non-small cell lung cancer. -
Key words:
- Advanced non-small cell lung cancer /
- Immunotherapy /
- Lymphocyte subset /
- Cytokines
-
表 1 控制组和无效组晚期非小细胞肺癌患者一般情况比较(例)
Table 1. Comparison of general condition of patients with advanced non-small cell lung cancer between control group and non-response group (cases)
组别 例数 性别 吸烟史 病理 免疫治疗 联合化疗 PD-L1a 男性 女性 有 无 腺癌 鳞癌 一线 非一线 是 否 <50% ≥50% 未知 控制组 36 27 9 21 15 21 15 20 16 34 2 12 5 19 无效组 12 10 2 9 3 8 4 2 10 11 1 6 2 4 χ2值 0.039 0.474 0.029 4.028 <0.001 P值 0.843 0.491 0.865 0.045 0.999 注:a为因PD-L1存在较多未知数据,故未行统计学比较。 表 2 控制组和无效组晚期非小细胞肺癌患者治疗前后淋巴细胞亚群比较
Table 2. Comparison of lymphocyte subsets in patients with advanced non-small cell lung cancer before and after treatment between control group and non-response group
组别 例数 CD19+[M(P25, P75),%] CD3+(x±s,%) CD3+CD4+(x±s,%) CD3+CD8+(x±s,%) 治疗前 治疗后 治疗前 治疗后 治疗前 治疗后 治疗前 治疗后 控制组 36 7.82(6.17, 9.90) 5.44(3.14, 9.71)b 62.45±11.71 69.25±11.84b 35.18±10.22 36.59±11.46 25.37±8.48 29.62±10.90 无效组 12 4.95(4.20, 7.32) 8.49(2.16, 11.56) 63.54±13.16 59.21±11.14 33.36±10.63 24.75±7.28 27.77±10.19 31.52±12.88 统计量 -1.790a -0.538a 0.213c 2.399c 0.413c 3.084c 0.568c 0.470c P值 0.073 0.590 0.833 0.021 0.683 0.004 0.584 0.640 组别 例数 CD4+/CD8+[M(P25, P75)] CD3-CD16+/56+[M(P25, P75),%] 淋巴细胞(x±s,μL) 总T淋巴细胞(x±s,μL) 治疗前 治疗后 治疗前 治疗后 治疗前 治疗后 治疗前 治疗后 控制组 36 1.48(0.99, 1.92) 1.23(0.75, 1.72) 22.74(11.64, 35.27) 23.17(13.92, 28.72) 1 784±633 1 648±564 1 133±446 1 121±388 无效组 12 1.18(1.15, 1.87) 0.89(0.44, 1.82) 32.96(19.01, 38.99) 33.79(20.55, 35.50) 1 286±443 1 098±581 804±295 651±368 统计量 -0.189a -1.201a -0.520a -1.747a 1.937c 2.703c 1.822c 3.525c P值 0.850 0.230 0.603 0.081 0.063 0.010 0.079 0.003 组别 例数 CD4+ T淋巴细胞[M(P25, P75),μL] CD8+T淋巴细胞[M(P25, P75),μL] B淋巴细胞[M(P25, P75),μL] NK细胞[M(P25, P75),μL] 治疗前 治疗后 治疗前 治疗后 治疗前 治疗后 治疗前 治疗后 控制组 36 582(439, 831) 540(367, 799) 417(292, 624) 472(292, 621) 139(97, 200) 79(58, 130) 408(181, 645) 318(183, 550) 无效组 12 374(266, 507) 245(125, 411) 319(235, 432) 266(174, 484) 87(45, 101) 50(35, 90) 383(145, 543) 288(132, 606) 统计量 -1.890a -3.180a -1.583a -1.911a -2.552a -1.611a -0.472a -0.232a P值 0.059 0.001 0.113 0.056 0.011 0.107 0.637 0.816 注:a为Z值;与同组治疗前比较,bP<0.05;c为t值。 表 3 淋巴细胞亚群及细胞因子与肿瘤进展的相关性分析
Table 3. Correlation analysis of lymphocyte subsets and cytokines with tumor progression
指标 r值 P值 CD3+CD4+ -0.286 0.038 淋巴细胞计数 -0.456 0.001 总T淋巴细胞计数 -0.497 <0.001 CD4+T细胞计数 -0.415 0.002 IL-4 0.607 0.008 IL-6 0.577 0.012 -
[1] SIEGEL R L, MILLER K D, FUCHS H E, et al. Cancer statistics, 2021[J]. CA Can J Clin, 2021, 71(1): 7-33. doi: 10.3322/caac.21654 [2] 谈艳芳, 刘利洪, 孙家祥. NSE、SCC-Ag、CEA、CYFRA21-1联合凝血指标检测在肺癌诊断中的应用价值[J]. 癌症进展, 2019, 17(16): 1960-1962. https://www.cnki.com.cn/Article/CJFDTOTAL-AZJZ201916026.htmTAN Y F, LIUL H, SUN J X. Application value of NSE, SCC-AG, CEA, CYFRA21-1 combined with coagulation index detection in the diagnosis of lung cancer[J]. Oncology Progress, 2019, 17(16): 1960-1962. https://www.cnki.com.cn/Article/CJFDTOTAL-AZJZ201916026.htm [3] 杨宇明, 段贵新, 王安生. lncRNA HOTAIR及肿瘤标志物联合检测与肺癌病理分期的相关性研究[J]. 中华全科医学, 2020, 18(10): 1652-1655. doi: 10.16766/j.cnki.issn.1674-4152.001584YANG Y M, DUAN G X, WANG A S. Correlation between lncRNA HOTAIR and tumor markers and pathological stage of lung cancer[J]. Chinese Journal of General Practice, 2020, 18(10): 1652-1655. doi: 10.16766/j.cnki.issn.1674-4152.001584 [4] ROSENTHAL R, CADIEUX E L, SALGADO R, et al. Neoantigen-directed immune escape in lung cancer evolution[J]. Nature, 2019, 567(7749): 479-485. doi: 10.1038/s41586-019-1032-7 [5] HAVEL J J, CHOWELL D. The evolving landscape of biomarkers for checkpoint inhibitor immunotherapy[J]. Nat Rev Can, 2019, 19(3): 133-150. doi: 10.1038/s41568-019-0116-x [6] 陈冠璇, 宋现让. 肺癌PD-1/PD-L1免疫检查点治疗疗效预测标志物[J]. 中国肺癌杂志, 2018, 21(9): 697-702. https://www.cnki.com.cn/Article/CJFDTOTAL-FAIZ201809012.htmCHAN G X, SONG X R. Predictive markers for treating efficacy of PD-1/PD-L1 inhibitors in patients with lung cancer[J]. Chinese Journal of Lung Cancer, 2018, 21(9): 697-702. https://www.cnki.com.cn/Article/CJFDTOTAL-FAIZ201809012.htm [7] 申宇嘉, 傅小龙. 非小细胞肺癌发生、发展过程中免疫微环境变化及其临床意义[J]. 中国癌症杂志, 2021, 31(11): 1115-1125. doi: 10.19401/j.cnki.1007-3639.2021.11.011SHAN Y J, FU X L. Research progress of immune contexture in tumorigenesis, progression and prognostic relevance of non-small cell lung cancer[J]. China Oncology, 2021, 31(11): 1115-1125. doi: 10.19401/j.cnki.1007-3639.2021.11.011 [8] LI X C, LYU Q S, FENG Y H, et al. Interleukin-33, a potential cytokine expressed in tumor microenvironment involves in antitumor immunotherapy through facilitates CD8 T cells[J]. J Interferon Cytokine Res, 2018, 38(11): 491-499. doi: 10.1089/jir.2018.0069 [9] MYERS J A, MILLER J S. Exploring the NK cell platform for cancer immunotherapy[J]. Nat Rev Clin Oncol, 2021, 182(2): 85-100. [10] VAN MONTFOOT N, BORST L, KORRER M J, et al. NKG2A blockade potentiates CD8 T cell immunity induced by cancer vaccines[J]. Cell, 2018, 175(7): 1744-1755. doi: 10.1016/j.cell.2018.10.028 [11] ZHANG W C, PAN Y L, GOU P H, et al. Effect of xanthohumol on Th1/Th2 balance in a breast cancer mouse model[J]. Oncol Rep, 2018, 39(1): 280-288. [12] LIN W, NIU Z Y, ZHANG H L, et al. Imbalance of Th1/Th2 and Th17/Treg during the development of uterine cervical cancer[J]. Int J Clin Exp Pathol, 2019, 12(9): 3604-3612. [13] 李文军, 范桂虹, 杨明, 等. 不同分期肺癌患者血清外周血Th1、Th2细胞因子、IL-18水平变化及其预后研究[J]. 实用医院临床杂志, 2018, 15(5): 187-189. https://www.cnki.com.cn/Article/CJFDTOTAL-YYLC201805060.htmLI W J, FAN G H, YANG M, et al. Changes of serum Th1 and Th2 cytokines and IL-18 levels in patients with lung cancer at different stages and their correlation with prognosis[J]. Practical Journal of Clinical Medicine, 2018, 15(5): 187-189. https://www.cnki.com.cn/Article/CJFDTOTAL-YYLC201805060.htm [14] 崔东, 许广辉, 贾忠伟, 等. NLR、VEGF、IL-6、TNF-α水平与非小细胞肺癌预后的相关性[J]. 现代肿瘤医学, 2019, 27(14): 2514-2518. https://www.cnki.com.cn/Article/CJFDTOTAL-SXZL201914021.htmCUI D, XU G H, JIA Z W, et al. Correlation between the levels of NLR, VEGF, IL-6, TNF-α, and the prognosis of NSCLC[J]. Journal of Modern Oncology, 2019, 27(14): 2514-2518. https://www.cnki.com.cn/Article/CJFDTOTAL-SXZL201914021.htm [15] JIA Y J, LI X F, ZHAO C, et al. Impact of serum vascular endothelial growth factor and interleukin-6 on treatment response to epidermal growth factor receptor tyrosine kinase inhibitors in patients with non-small-cell lung cancer[J]. Lung Can, 2018, 125(1): 22-28. [16] 武道荣, 闫雪波, 方磊, 等. qSOFA评分联合IL-6 PCT CRP对ICU感染性休克患者病情及预后的评估价值[J]. 安徽医学, 2021, 42(8): 850-854. https://www.cnki.com.cn/Article/CJFDTOTAL-AHYX202108006.htmWU D R, YAN X B, FANG L, et al. The evaluation value of qSOFA score combined with serum IL-6, PCT and CRP levels for judgment and prognosis of ICU patients with septic shock[J]. Anhui Medical Journal, 2021, 42(8): 850-854. https://www.cnki.com.cn/Article/CJFDTOTAL-AHYX202108006.htm [17] 吴晋楠, 陈建荣, 陈金亮, 等. 肺癌肿瘤微环境中白细胞介素的研究进展[J]. 临床肺科杂志, 2019, 24(12): 2280-2283. https://www.cnki.com.cn/Article/CJFDTOTAL-LCFK201912034.htmWU J N, CHEN J R, CHEN J L, et al. Research progress of interleukins in tumor microenvironment of lung cancer[J]. Journal of Clinical Pulmonary Medicine, 2019, 24(12): 2280-2283. https://www.cnki.com.cn/Article/CJFDTOTAL-LCFK201912034.htm [18] 高斌成. 非小细胞肺癌外周血CD3+、CD4+等T淋巴细胞亚群水平及意义[J]. 临床肺科杂志, 2018, 23(1): 138-141. https://www.cnki.com.cn/Article/CJFDTOTAL-LCFK201801038.htmGAO B C. Expression and significance of CD3+, CD4+ T lymphocyte subsets in patients with non-small cell lung cancer[J]. Journal of Clinical Pulmonary Medicine, 2018, 23(1): 138-141. https://www.cnki.com.cn/Article/CJFDTOTAL-LCFK201801038.htm [19] 林晓骥, 孙妮, 周晓海, 等. PD-1在弥漫性大B细胞淋巴瘤患者外周血CD4+T细胞和CD8+T细胞上的表达和临床意义[J]. 中国卫生检验杂志, 2018, 28(5): 556-558. https://www.cnki.com.cn/Article/CJFDTOTAL-ZWJZ201805014.htmLIN X Y, SUN N, ZHOU X H, et al. Expression and clinical significance of PD-1 on CD4+ and CD+ T cells from the peripheral blood of patients with diffuse large B-cell lymphoma[J]. Chinese Journal of Health Laboratory Technology, 2018, 28(5): 556-558. https://www.cnki.com.cn/Article/CJFDTOTAL-ZWJZ201805014.htm [20] 王芸, 王郁阳, 姜曼, 等. 帕博利珠单抗对晚期非小细胞肺癌患者T淋巴细胞亚群的影响及疗效观测[J]. 中国肺癌杂志, 2021, 24(3): 182-187. https://www.cnki.com.cn/Article/CJFDTOTAL-FAIZ202103005.htmWANG Y, WANG Y Y, JIANG M, et al. Effect of pembrolizumab on T lymphocyte subsets in patients with advanced non-small cell lung cancer and its therapeutic effect[J]. Chinese Journal of Lung Cancer, 2021, 24(3): 182-187. https://www.cnki.com.cn/Article/CJFDTOTAL-FAIZ202103005.htm -





 下载:
下载: