The correlation between the dynamic analysis of uterine artery ultrasound parameters during pregnancy and the risk of preeclampsia
-
摘要:
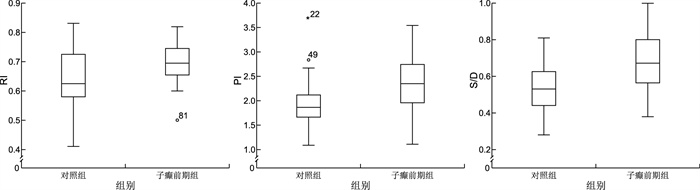
目的 动态分析孕期患者子宫动脉超声参数及其与子痫前期发生风险的相关性。 方法 纳入2020年1月—2021年10月湖州市妇幼保健院接受子宫动脉超声检查的60例子痫前期患者为子痫前期组,另纳入同期接受子宫动脉超声检查的60例未发生子痫前期的孕妇为对照组。动态分析2组患者孕期子宫动脉超声参数及其与孕期孕妇子痫前期的相关性。 结果 2组孕妇随孕期的延长RI值、PI值、S/D值均降低,且对照组RI值、PI值、S/D值均低于子痫前期组(均P<0.05);Pearson相关系数分析显示,孕11~16周及孕20~24周RI值、PI值、S/D值与孕妇子痫前期风险呈正相关(r=0.602、0.774、0.638;r=0.809、0.833、0.608,均P<0.05);多因素logistic回归分析显示,孕11~16周及孕20~24周高RI值、高PI值、高S/D是孕期孕妇子痫前期的危险因素(OR=2.463、1.239、1.599;OR=1.643、1.568、1.741,均P < 0.05);ROC曲线分析显示,孕11~16周子宫动脉超声参数预测价值(AUC为0.965)高于孕20~24周子宫动脉超声参数(AUC为0.885,P<0.05)。 结论 随着孕期的延长孕妇子宫动脉RI、PI、S/D指标逐渐降低,与孕妇子痫前期发生风险呈正相关,并可作为孕妇子痫前期发生风险的预测指标。 Abstract:Objective To dynamically analyse the ultrasound parameters of uterine arteries and their correlation with the risk of preeclampsia in pregnant patients. Methods A total of 60 cases of preeclampsia patients who received uterine artery ultrasonography in Huzhou Maternity and Children ' s Health Hospital from January 2020 to October 2021 were included in the preeclampsia group, and 60 patients who received uterine artery ultrasonography during the same period without preeclampsia were included as the control group. The ultrasound parameters of the uterine artery during pregnancy and their correlation with preeclampsia during pregnancy were dynamically analysed. Results The RI value, PI value and S/D value of pregnant women in both groups decreased with the prolongation of pregnancy, and the RI value, PI value and S/D value of the control group were lower than those of the preeclampsia group (all P < 0.05). Pearson correlation coefficient analysis showed that the RI value, PI value and S/D value at 11-16 weeks of pregnancy and 20-24 weeks of pregnancy were positively correlated with the risk of preeclampsia (r=0.602, 0.774, 0.638; r=0.809, 0.833, 0.608, all P < 0.05). Multivariate logistic regression analysis showed that high RI value, high PI value and high S/D value at 11-16 weeks of pregnancy and 20-24 weeks of pregnancy were the risk factors of preeclampsia in pregnant women (OR=2.463, 1.239, 1.599; OR=1.643, 1.568, 1.741, all P < 0.05). ROC curve analysis showed that the predictive value of uterine artery ultrasound parameters at 11-16 weeks of gestation (AUC was 0.965) was higher than the uterine artery ultrasound parameters at 20-24 weeks of gestation (AUC was 0.885, P < 0.05). Conclusion The RI, PI and S/D index of the uterine artery in pregnant women decrease with the prolongation of pregnancy, which is positively correlated with the risk of preeclampsia in pregnant women, and can be used as a predictor of the risk of preeclampsia in pregnant women. -
Key words:
- Pregnancy /
- Uterine artery /
- Ultrasound /
- Dynamic analysis /
- Preeclampsia
-
表 1 2组孕妇临床资料比较
Table 1. Comparison of clinical data between two groups of pregnant women
项目 对照组(n=60) 子痫前期组(n=60) 统计量 P值 年龄(x±s,岁) 24.57±5.60 26.61±5.98 1.929a 0.056 吸烟[例(%)] 2(3.33) 3(5.00) <0.001b 0.999 饮酒[例(%)] 3(5.00) 4(6.67) <0.001b 0.999 BMI(x±s) 25.53±3.28 24.69±3.05 1.453a 0.149 受孕方法[例(%)] 1.034b 0.309 自然受孕 57(95.00) 59(98.33) 人工受孕 3(5.00) 1(1.67) 经产妇[例(%)] 27(45.00) 25(41.67) 0.136a 0.713 胎次(x±s,次) 1.47±0.31 1.42±0.28 0.927a 0.356 RI(11~16周)值(x±s) 0.64±0.09 0.70±0.06 3.842a < 0.001 PI(11~16周)值(x±s) 1.93±0.42 2.34±0.50 4.895a < 0.001 S/D(11~16周)值(x±s) 0.54±0.13 0.68±0.15 5.279a < 0.001 RI(20~24周)值(x±s) 0.56±0.12 0.62±0.14 2.402a 0.018 PI(20~24周)值(x±s) 1.30±0.16 1.62±0.37 6.126a < 0.001 S/D(20~24周)值(x±s) 0.46±0.21 0.57±0.20 3.011a 0.003 HR(x±s,次/min) 85.58±6.80 87.26±8.86 1.165a 0.246 MAP(x±s,mm Hg) 86.34±10.25 88.75±10.30 1.285a 0.201 注:a为t值, b为χ2值。1 mm Hg=0.133 kPa。 表 2 不同孕周子宫动脉超声参数与子痫前期风险的相关性
Table 2. Correlation between uterine artery ultrasound parameters at different gestational weeks and the risk of preeclampsia
项目 11~16周 20~24周 r值 95% CI P值 r值 95% CI P值 RI值 0.602 0.496~0.703 < 0.001 0.809 0.758~0.856 < 0.001 PI值 0.774 0.714~0.830 < 0.001 0.833 0.778~0.886 < 0.001 S/D值 0.638 0.545~0.723 < 0.001 0.608 0.503~0.699 < 0.001 表 3 相关变量赋值表
Table 3. Related variable assignment table
变量 赋值方法 是否发生子痫前期 是=1,否=0 RI(11~16周)值 以实际值赋值 PI(11~16周)值 以实际值赋值 S/D(11~16周)值 以实际值赋值 RI(20~24周)值 以实际值赋值 PI(20~24周)值 以实际值赋值 S/D(20~24周)值 以实际值赋值 表 4 孕期子痫前期风险的影响因素分析
Table 4. Analysis of factors influencing the risk of preeclampsia during pregnancy
变量 B SE Wald χ2 P值 OR值 95% CI RI(11~16周)值 0.901 0.389 5.383 0.020 2.463 2.150~2.775 PI(11~16周)值 0.214 0.068 10.065 0.002 1.239 1.085~1.415 S/D(11~16周)值 0.469 0.213 4.832 0.028 1.599 1.052~2.030 RI(20~24周)值 0.497 0.234 4.492 0.034 1.643 1.638~2.601 PI(20~24周)值 0.450 0.127 12.615 <0.001 1.568 1.223~1.810 S/D(20~24周)值 0.554 0.165 11.225 0.001 1.741 1.259~2.007 -
[1] 陈娅, 张英. 子痫前期再发对病情和妊娠结局的影响[J]. 中华全科医学, 2019, 17(2): 209-211, 287. doi: 10.16766/j.cnki.issn.1674-4152.000641CHEN Y, ZHANG Y. Impact of recurrent preeclampsia on clinical manifestations and pregnancy outcomes[J]. Chinese Journal of General Practice, 2019, 17(2): 209-211, 287. doi: 10.16766/j.cnki.issn.1674-4152.000641 [2] 黄琳, 陈敦金, 陈兢思. 子痫前期的预防新进展[J]. 中国医师杂志, 2020, 22(7): 972-976.HUANG L, CHEN D J, CHEN J S. New progress in prevention of preeclampsia[J]. Journal of Chinese Physician, 2020, 22(7): 972-976. [3] 邓晨晨, 陶峰, 陈红波. 子宫动脉多普勒超声预测子痫前期的研究现状[J]. 中华全科医学, 2020, 18(6): 1002-1005. doi: 10.16766/j.cnki.issn.1674-4152.001413DENG C C, TAO F, CHEN H B. Prediction of uterine artery doppler for preeclampsia[J]. Chinese Journal of General Practice, 2020, 18(6): 1002-1005. doi: 10.16766/j.cnki.issn.1674-4152.001413 [4] KALAFAT E, LAORETI A, KHALILl A, et al. Ophthalmic artery doppler for prediction of pre-eclampsia: Systematic review and meta-analysis[J]. Ultrasound Obstet Gynecol, 2018, 51(6): 731-737. doi: 10.1002/uog.19002 [5] SERRA B, MENDOZA M, SCAZZOCCHIO E, et al. A new model for screening for early-onset preeclampsia[J]. Am J Obstet Gynecol, 2020, 222(6): 608. e1-608. e18. DOI: 10.1016/j.ajog.2020.01.020. [6] 杨孜, 张为远. 妊娠期高血压疾病诊治指南(2015)[J]. 中华围产医学杂志, 2016, 19(3): 161-169. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGSF201510002.htmYANG Z, ZHANG W Y. Guidelines for diagnosis and treatment of hypertensive diseases during pregnancy (2015)[J]. Chinese Journal of Perinatal Medicine, 2016, 19(3): 161-169. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGSF201510002.htm [7] HWUANG E, VIDORRRETA M, SCHWARTZ N, et al. Assessment of uterine artery geometry and hemodynamics in human pregnancy with 4d flow mri and its correlation with doppler ultrasound[J]. J Magn Reson Imaging, 2019, 49(1): 59-68. doi: 10.1002/jmri.26229 [8] PLASENCIA W, MAIZ N, POON L, et al. Uterine artery Doppler at 11+0 to 13+6 weeks and 21+0 to 24+6 weeks in the prediction of pre-eclampsia[J]. Ultrasound Obstet Gynecol, 2008, 32(2): 138-146. doi: 10.1002/uog.5402 [9] WANG W, WANG Y Y, YUAN T, et al. Nomogram-based prediction of pre-eclampsia in the first trimester of gestation[J]. Pregnancy Hypertens, 2020, 21(1): 145-151. [10] ADEKANMI A J, ROBERTS A, AKONMOLADUN J A, et al. Uterine and umbilical artery doppler in women with pre-eclampsia and their pregnancy outcomes[J]. Niger Postgrad Med J, 2019, 26(2): 106-112. [11] MULA R, MLERER E, ALBAIGES G, et al. Strategies for the prediction of late preeclampsia[J]. J Matern Fetal Neonatal Med, 2019, 32(22): 3729-3733. [12] DI PASQUO E, GHI T, DALL'ASTA A, et al. Maternal cardiac parameters can help in differentiating the clinical profile of preeclampsia and in predicting progression from mild to severe forms[J]. Am J Obstet Gynecol, 2019, 221(6): 633. e1-633. e9. DOI: 10.1016/j.ajog.2019.06.029. [13] MASINI G, TORDINI C, PIETROSABTE A, et al. Prediction of pregnancy complications by second-trimester uterine artery Doppler assessment in monochorionic twins[J]. J Clin Ultrasound, 2019, 47(7): 399-404. [14] GUY G P, LING H Z, GARCIA P, et al. Maternal cardiac function at 35-37 weeks ' gestation: Prediction of pre-eclampsia and gestational hypertension[J]. Ultrasound Obstet Gynecol, 2017, 49(1): 61-66. [15] CLARK A R, JAMES J L, STEVENSON G N, et al. Understanding abnormal uterine artery Doppler waveforms: A novel computational model to explore potential causes within the utero-placental vasculature[J]. Placenta, 2018, 66(1): 74-81. [16] ADEKANMI A J, ROBERTS A, AKINMOLADUN J A, et al. Uterine and umbilical artery doppler in women with pre-eclampsia and their pregnancy outcomes[J]. Niger Postgrad Med J, 2019, 26(2): 106-112. [17] TORABI S, SHEIKH M, FATTAHI MASROUR F, et al. Uterine artery Doppler ultrasound in second pregnancy with previous elective cesarean section[J]. J Matern Fetal Neonatal Med, 2019, 32(13): 2221-2227. [18] TAYLOR T J, QUINTON A E, DE VRIES B S, et al. Uterine artery pulsatility ondex assessment at <11 weeks ' gestation: A prospective study[J]. Fetal Diagn Ther, 2020, 47(2): 129-137. -





 下载:
下载: