Correlation between condylar anatomical measurement based on digital three-dimensional reconstruction and common symptoms of unilateral temporomandibular joint disorder
-
摘要:
目的 对颌面部CT病例资料进行三维重建和解剖学测量,回顾性分析颞下颌关节紊乱病(temporomandibular joint disorders, TMD)的常见临床症状与髁突形态的相关性。 方法 选取2020年6月—2021年9月就诊于蚌埠医学院附属蚌埠第三人民医院口腔科的156例患者,根据临床检查及主诉症状分为实验组(弹响组、疼痛组和张口受限组)和对照组(无TMD症状组)。患者于放射科拍摄颌面部CT,通过运行Mimics软件,获取三维重建后的下颌骨髁突形态,并进行解剖学测量。 结果 对照组的髁突内外径、前后径分别为(21.42±1.93)mm、(11.66±1.22)mm,髁突前后角度为(105.86±6.67)°;弹响组的髁突内外径、前后径以及髁突前后角度分别为(21.47±2.38)mm、(10.64±1.10)mm、(97.38±6.76)°;疼痛组的髁突内外径、前后径以及髁突前后角度分别为(21.25±1.04)mm、(12.17±0.81)mm、(104.00±6.73)°;张口受限组的髁突内外径、前后径以及髁突前后角度分别为(20.48±2.17)mm、(11.55±1.57)mm、(106.79±8.36)°。在有关节弹响的患者中,髁突前后径较对照组减少,髁突前后角度也相应变小;在伴发关节疼痛的患者中,髁突前后径较对照组增大;而张口受限组的髁突形态与对照组比较无明显差异。 结论 TMD患者的髁突解剖学测量具有一定的差异,可为TMD的辅助诊断提供参考。 Abstract:Objective To retrospectively analyzed the correlation between common clinical symptoms of temporomandibular joint disorders (TMD) and condyle morphology by performing 3D reconstruction and anatomical measurement. Methods A total of 156 patients who were treated in Department of Stomatology, Bengbu Third People ' s Hospital Affiliated to Bengbu Medical College from June 2020 to September 2021 were divided into experimental group (click group, pain group, and mouth opening limitation group) and control group (no TMD symptom group). The patients were all taken in the Department of Radiology for maxillofacial CT, and three-dimensional reconstruction was performed by Mimics software to obtain the mandibular condyle shape and anatomical measurement was carried out. Results Condylar interior-exterior diameter, condylar anteroposterior diameter, condylar anteroposterior angle in the non TMD symptom group were (21.42±1.93) mm, (11.66±1.22) mm, and (105.86±6.67)°, respectively. These three parameters were (21.47±2.38) mm, (10.64±1.10) mm, (97.38±6.76)° in the click group; (21.25±1.04) mm, (12.17±0.81) mm, (104.00±6.73)° in the pain group; (20.48±2.17) mm, (11.55±1.57) mm, (106.79±8.36)° in the mouth opening limitation group. In the patients with joint snapping, the anterior and posterior condylar diameter decreased, and the anterior and posterior condylar angle also decreased. In patients with joint pain, the anteroposterior diameter of the condyle was larger than that of the control group, while the condyle shape of the mouth opening restriction group had no significant difference from that of the control group. Conclusion Condylar anatomical measurements are different in TMD patients, suggesting that anatomical measurements may provide a assist for diagnosis of TMD. -
表 1 弹响组与对照组患者髁突测量值比较(x±s)
Table 1. Comparison of condyle measurement between click group and control group(x±s)
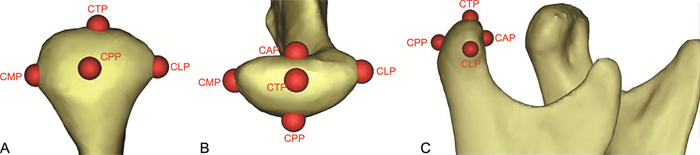
组别 例数 CMP-CLP(mm) CAP-CPP(mm) CAP-CPP/CMP-CLP ∠CAP-CTP-CPP(°) 对照组 39 21.42±1.93 11.66±1.22 1.84±0.35 105.86±6.67 弹响组 64 21.47±2.38 10.64±1.10 2.01±0.44 97.38±6.76 t值 0.101 4.383 1.022 6.225 P值 0.167 < 0.001 0.087 < 0.001 表 2 疼痛组与对照组患者髁突测量值比较(x±s)
Table 2. Comparison of condyle measurement between pain group and control group(x±s)
组别 例数 CMP-CLP(mm) CAP-CPP(mm) CAP-CPP/CMP-CLP ∠CAP-CTP-CPP(°) 对照组 39 21.42±1.93 11.66±1.22 1.84±0.35 105.86±6.67 疼痛组 34 21.25±1.04 12.17±0.81 1.75±0.33 104.00±6.73 t值 0.446 2.079 1.332 0.728 P值 0.644 0.036 0.063 0.469 表 3 张口受限组与对照组患者髁突测量值比较(x±s)
Table 3. Comparison of condyle measurement between mouth opening limitation group and control group(x±s)
组别 例数 CMP-CLP(mm) CAP-CPP(mm) CAP-CPP/CMP-CLP ∠CAP-CTP-CPP(°) 对照组 39 21.42±1.93 11.66±1.22 1.84±0.35 105.86±6.67 张口受限组 19 20.48±2.17 11.55±1.57 1.77±0.42 106.79±8.36 t值 1.675 0.293 0.257 0.456 P值 0.118 0.791 0.087 0.675 -
[1] 赵四可, 夏章容, 钟小康, 等. 基于干燥标本距下关节面的解剖学测量及临床意义[J]. 解剖学杂志, 2022, 45(1): 52-56. https://www.cnki.com.cn/Article/CJFDTOTAL-JPXZ202201010.htmZHAO S K, XIA Z R, ZHONG X K, et al. Anatomical measurement of subtalar articular surface in dried specimens and its clinical significance[J]. Chinese Journal of Anatomy, 2022, 45(1): 52-56. https://www.cnki.com.cn/Article/CJFDTOTAL-JPXZ202201010.htm [2] 任瑞阳, 苏崇莹, 熊晨燚, 等. 颅面部数字化三维影像重叠的稳定结构研究进展[J]. 中国实用口腔科杂志, 2022, 15(1): 113-117. https://www.cnki.com.cn/Article/CJFDTOTAL-ZSKQ202201022.htmREN R Y, SU C Y, XIONG C Y, et al. Research progress on stable structures of three-dimensional craniofacial digital image superimposition[J]. Chinese Journal of Practical Stomatology, 2022, 15(1): 113-117. https://www.cnki.com.cn/Article/CJFDTOTAL-ZSKQ202201022.htm [3] 张邀光, 房维. 颞下颌关节紊乱病诊断标准的研究进展[J]. 口腔医学研究, 2021, 37(12): 1069-1072. doi: 10.13701/j.cnki.kqyxyj.2021.12.002ZHANG Y G, FANG W. Progress of diagnostic criteria for temporomandibular disorders[J]. Journal of Oral Science Research, 2021, 37(12): 1069-1072. doi: 10.13701/j.cnki.kqyxyj.2021.12.002 [4] 傅开元, 胡敏, 余强, 等. 颞下颌关节紊乱病锥形束CT检查规范及诊断标准的专家共识[J]. 中华口腔医学杂志, 2020, 55(9): 613-616. doi: 10.3760/cma.j.cn112144-20200514-00267FU K Y, HU M, YU Q, et al. Experts consensus on cone-beam CT examination specification and diagnostic criteria of temporomandibular disorders[J]. Chinese Journal of Stomatology, 2020, 55(9): 613-616. doi: 10.3760/cma.j.cn112144-20200514-00267 [5] 何妍明, 王荷燕, 冯亚平, 等. 颞下颌关节盘MRI和锥形束CT图像配准的初步研究[J]. 中华口腔医学杂志, 2020, 55(10): 772-777. doi: 10.3760/cma.j.cn112144-20200605-00319HE Y M, WANG H Y, FENG Y P, et al. A preliminary study on the registration of MRI and cone beam CT images of temporomandibular joint disc[J]. Chinese Journal of Stomatology, 2020, 55(10): 772-777. doi: 10.3760/cma.j.cn112144-20200605-00319 [6] 齐鑫, 刘洋. 颞下颌关节紊乱病诊治指南中文版出版发行[J]. 中华老年口腔医学杂志, 2021, 19(4): 257. https://www.cnki.com.cn/Article/CJFDTOTAL-ZHKQ202104016.htmQI X, LIU Y. Manual of temporomandibular disorders[J]. Chinese Journal of Geriatric Dentistry, 2021, 19(4): 257. https://www.cnki.com.cn/Article/CJFDTOTAL-ZHKQ202104016.htm [7] 张颖, 冯梓峻, 黎星阳, 等. 基于CBCT下颞下颌关节造影的关节盘穿孔与髁突骨质改变相关性研究[J]. 口腔医学研究, 2020, 36(4): 333-336. https://www.cnki.com.cn/Article/CJFDTOTAL-KQYZ202004008.htmZHANG Y, FENG Z J, LI X Y, et al. Correlation between disc perforation and condylar bone changes based on temporomandibular joint arthrography by CBCT[J]. Journal of Oral Science Research, 2020, 36(4): 333-336. https://www.cnki.com.cn/Article/CJFDTOTAL-KQYZ202004008.htm [8] 赵茜, 孙娜, 张风河, 等. 颞下颌关节及其周围骨性结构的三维测量[J]. 山东大学学报(医学版), 2019, 57(1): 87-91. https://www.cnki.com.cn/Article/CJFDTOTAL-SDYB201901023.htmZHAO Q, SUN N, ZHANG F H, et al. Measurement of temporomandibular joint and surrounding accessory structures[J]. Journal of Shandong University (Health Sciences), 2019, 57(1): 87-91. https://www.cnki.com.cn/Article/CJFDTOTAL-SDYB201901023.htm [9] 王琰, 王靖虓, 郭倩倩, 等. 颞下颌关节盘不可复性前移位行锚固术后的临床疗效及影像学分析[J]. 中华全科医学, 2021, 19(7): 1125-1127, 1154. doi: 10.16766/j.cnki.issn.1674-4152.002001WANG Y, WANG J X, GUO Q Q, et al. Clinical effect and imaging analysis of disc anchor surgery for anterior disc displacement without reduction[J]. Chinese Journal of General Practice, 2021, 19(7): 1125-1127, 1154. doi: 10.16766/j.cnki.issn.1674-4152.002001 [10] COLONNA A, MANFREDINI D, LOMBARDO L, et al. Comparative analysis of jaw morphology and temporomandibular disorders: A three-dimension imaging study[J]. Cranio, 2020, 38(3): 158-167. [11] 周涛, 钱永, 刘韦淞, 等. CBCT在青少年双侧颞下颌关节测量中的应用价值探讨[J]. 口腔颌面修复学杂志, 2020, 21(5): 282-285, 290. https://www.cnki.com.cn/Article/CJFDTOTAL-KHXF202005006.htmZHOU T, QIAN Y, LIU W S, et al. Application value of CBCT in measurement of bilateral temporomandibular joint in adolescents[J]. Chinese Journal of Prosthodontics, 2020, 21(5): 282-285, 290. https://www.cnki.com.cn/Article/CJFDTOTAL-KHXF202005006.htm [12] SEMBRONIO S, TEL A, ROBIONY M. Protocol for fully digital and customized management of concomitant temporomandibular joint replacement and orthognathic surgery[J]. Int J Oral Maxillofac Surg, 2021, 50(2): 212-219. [13] ISKANDERANI D, ALSTERGREN P, EKBERG E C, et al. Web-based educational programme for temporomandibular joint assessment with cone-beam computed tomography[J]. J Oral Rehabil, 2020, 47(11): 1330-1336. [14] 傅开元, 胡敏, 余强, 等. 颞下颌关节常规MRI检查规范及关节盘移位诊断标准的专家共识[J]. 中华口腔医学杂志, 2020, 55(9): 608-612.FU K Y, HU M, YU Q, et al. Experts consensus on MRI examination specification and diagnostic criteria of temporomandibular joint disc displacement[J]. Chinese Journal of Stomatology, 2020, 55(9): 608-612. [15] 曾东林, 刘依, 张志光, 等. 关节造影锥形束CT影像检查在颞下颌关节紊乱病诊断中的应用[J]. 中华口腔医学杂志, 2020, 55(9): 634-638.ZENG D L, LIU Y, ZHANG Z G, et al. Application of arthrography with cone-beam CT imaging in the diagnosis of temporomandibular disorders[J]. Chinese Journal of Stomatology, 2020, 55(9): 634-638. [16] 李源, 刘木清, 刘博, 等. 基于锥形束CT影像的颞下颌关节髁突骨改建三维定量评价研究[J]. 中华口腔医学杂志, 2020, 55(9): 617-623.LI Y, LIU M Q, LIU B, et al. Three-dimensional quantitative evaluation of condylar bone remodeling of temporomandibular joint based on cone-beam CT imaging[J]. Chinese Journal of Stomatology, 2020, 55(9): 617-623. [17] ZHENG T, ZHAO Z. Imaging application and progress in the diagnosis of temporomandibular joint diseases[J]. Minerva Surg, 2021, 76(6): 604-606. [18] 郑吉驷, 焦子先, 白果, 等. 定制型颞下颌关节-下颌骨联合假体的临床初步应用[J]. 上海交通大学学报(医学版), 2020, 40(10): 1376-1381. https://www.cnki.com.cn/Article/CJFDTOTAL-SHEY202010018.htmZHENG J S, JIAO Z X, BAI G, et al. Clinical application of custom-made temporomandibular joint-mandible combined prosthesis[J]. Journal of Shanghai Jiaotong University (Medical Science), 2020, 40(10): 1376-1381. https://www.cnki.com.cn/Article/CJFDTOTAL-SHEY202010018.htm [19] 吴齐越, 庄艳琴, 吴明月. 青年学生上颌前牙区软硬组织厚度的锥形束CT测量分析[J]. 安徽医学, 2018, 39(4): 386-391. https://www.cnki.com.cn/Article/CJFDTOTAL-AHYX201804004.htmQU Q Y, ZHUANG Y Q, WU M Y. Measurement and analysis of thickness of soft and hard tissue in maxillary anterior teeth of young students by cone beam CT[J]. Anhui Medical Journal, 2018, 39(4): 386-391. https://www.cnki.com.cn/Article/CJFDTOTAL-AHYX201804004.htm [20] 翟孝庭, 黄东宗, 李鸿波, 等. 颞下颌关节紊乱病专病数据库的设计与初步构建[J]. 口腔颌面修复学杂志, 2021, 22(5): 354-360. https://www.cnki.com.cn/Article/CJFDTOTAL-KHXF202105011.htmZHAI X T, HUANG D Z, LI H B, et al. Design and construction of the special disease database for temporomandibular joint disorders[J]. Chinese Journal of Prosthodontics, 2021, 22(5): 354-360. https://www.cnki.com.cn/Article/CJFDTOTAL-KHXF202105011.htm [21] TRAN C, GHAHREMAN K, HUPPA C, et al. Management of temporomandibular disorders: A rapid review of systematic reviews and guidelines[J]. Int J Oral Maxillofac Surg, 2022, 51(9): 1211-1225. [22] 原玉娟, 冯云霞, 任娟, 等. 颞下颌关节紊乱病和咬合因素的相关研究[J]. 口腔医学研究, 2018, 34(3): 226-228. https://www.cnki.com.cn/Article/CJFDTOTAL-KQYZ201803004.htmYUAN Y J, FENG Y X, REN J, et al. Relationship between Temporomandibular Disorders and Occlusal Factors[J]. Journal of Oral Science Research, 2018, 34(3): 226-228. https://www.cnki.com.cn/Article/CJFDTOTAL-KQYZ201803004.htm [23] 李红光, 吴训, 彭慧钰, 等. 基于CBCT的单侧颞下颌关节骨关节炎临床表现与髁突骨质改变类型的相关性分析[J]. 现代口腔医学杂志, 2022, 36(3): 148-152. https://www.cnki.com.cn/Article/CJFDTOTAL-XDKY202203001.htmLI H G, WU X, PENG H Y, et al. Correlation analysis of the clinical manifestations and different types of condylar bone changes in unilateral temporomandibular joint osteoarthritis based on CBCT[J]. Journal of Modern Stomatology, 2022, 36(3): 148-152. https://www.cnki.com.cn/Article/CJFDTOTAL-XDKY202203001.htm [24] 王倩倩, 韩瑞, 丁翔, 等. 改良耳颞切口联合颌下切口在髁状突囊内骨折术中的应用研究[J]. 中华全科医学, 2020, 18(9): 1446-1448, 1461. doi: 10.16766/j.cnki.issn.1674-4152.001529WANG Q Q, HAN R, DING X, et al. Study on the application of modified auriculotemporal incision combined with submaxillary incision in intracapsular condylar fracture[J]. Chinese Journal of General Practice, 2020, 18(9): 1446-1448, 1461. doi: 10.16766/j.cnki.issn.1674-4152.001529 -





 下载:
下载: