Clinical study of individualized nutritional intervention in elderly patients with tumors
-
摘要:
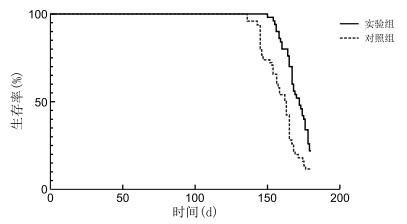
目的 探索个体化营养干预对老年肿瘤患者的营养、Karnofsky功能状态评分(KPS评分)、生活质量及寿命的影响。 方法 选取2016年1月—2019年12月于上海交通大学医学院附属新华医院崇明分院肿瘤科住院治疗的老年肿瘤患者100例,采用随机数字表法分为实验组和对照组,每组50例。对照组根据患者的病情、临床症状,参照美国国立综合癌症网络指南及诊疗常规,采取常规的支持治疗及姑息性抗肿瘤治疗,实验组在对照组的基础上增加个体化营养干预措施。个体化营养干预措施包含营养风险筛查及评估,根据筛查结果分别给予营养教育及膳食指导、口服营养补充营养、肠内营养及肠外营养干预。入组时、入组后2个月比较2组患者BMI指数、KPS评分、生活质量评分,入组后6个月时统计入组患者的生存期。 结果 干预后,2组患者的BMI、KPS评分比较差异有统计学意义(均P < 0.05), 实验组生活质量评分[(20.75±1.67)分]高于对照组[(18.23±3.19)分,P < 0.001]。实验组中位生存期为172.0 d,对照组中位生存期为162.5 d,2组比较差异有统计学意义(P < 0.001)。 结论 个体化营养干预可以延缓老年肿瘤患者的BMI下降、抑制KPS评分下降、限制生活质量下降,延长患者的寿命,值得在临床工作中推广。 -
关键词:
- 个体化营养干预 /
- 老年晚期肿瘤 /
- 体重指数 /
- 生活质量 /
- Karnofsky功能状态评分
Abstract:Objective To explore the effects of individualized nutrition intervention on nutrition, Karnofsky performance score (KPS), quality of life and life span in elderly cancer patients. Methods A total of 100 elderly cancer patients treated in the Department of Oncology, Chongming Branch of Xinhua Hospital Affiliated to Shanghai Jiao Tong University Medical College from January 2016 to December 2019 were selected and randomly divided into test group and control group, with 50 patients in each group. The control group adopted routine supportive treatment and palliative anti-tumor treatment according to the patient ' s condition and clinical symptoms with reference to the national comprehensive cancer network (NCCN) guidelines and the routine diagnosis and treatment. While, the test group carried out individualized nutritional intervention on the basis of the control group. Individualized nutrition intervention measures included nutrition risk screening and evaluation. According to the screening results, nutrition education and dietary guidance, oral nutrition and supplementary nutrition, enteral nutrition and parenteral nutrition intervention were given respectively. BMI, KPS and quality of life score of all patients were checked at the time of enrollment and 2 months after enrollment, and survival time of enrolled patients was calculated at 6 months after enrollment. Results After the intervention, the BMI and KPS scores of the two groups were statistically significant (all P < 0.05). The quality of life score of the test group [(20.75±1.67) points] was higher than that of the control group [(18.23±3.19) points, P < 0.001]. The median survival time was 172.0 days in the test group and 162.5 days in the control group, and the difference between the two groups was statistically significant (P < 0.001). Conclusion Individualized nutritional intervention can delay the decline of BMI, inhibit the decline of KPS score, limit the decline of quality of life and extend the life of elderly patients with tumors, which is worth promoting in clinical practice. -
表 1 2组老年晚期肿瘤患者BMI比较(x±s)
组别 例数 干预前 干预后 实验组 50 18.23±2.38 17.56±2.30 对照组 50 18.15±2.55 16.23±3.19a t值 0.162 2.391 P值 0.872 0.019 注:与同组干预前比较,aP < 0.01。 表 2 2组老年晚期肿瘤患者KPS评分比较(x±s,分)
组别 例数 干预前 干预后 实验组 50 79.40±13.00 74.20±11.80a 对照组 50 78.40±13.30 68.60±11.72a t值 0.380 2.381 P值 0.705 0.019 注:与同组干预前比较,aP < 0.01。 表 3 2组老年晚期肿瘤患者生活质量评分比较(x±s,分)
组别 例数 干预前 干预后 实验组 50 22.81±4.33 20.75±1.67a 对照组 50 23.12±2.95 18.23±3.19a t值 0.418 4.949 P值 0.677 < 0.001 注:与同组干预前比较,aP < 0.01。 -
[1] BRAY F, FERLAY J, SOERJOMATARAM I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries[J]. CA Cancer J Clin, 2018, 68(6): 394-424. doi: 10.3322/caac.21492 [2] 高崇崇, 李非. 我国老年恶性肿瘤发病特点及危险因素分析[J]. 老年医学与保健, 2018, 24(6): 729-731. doi: 10.3969/j.issn.1008-8296.2018.06.048 [3] 陈蕾, 冯苏梅. 恶性肿瘤患者营养评估与营养支持[J]. 临床医药文献电子杂志, 2018, 5(70): 27, 29. doi: 10.3877/j.issn.2095-8242.2018.70.018 [4] 宋康颉, 章琪, 何承龙, 等. 腹腔镜与开腹胃癌根治术后早期肠内营养的对比研究[J]. 肠外与肠内营养, 2018, 25(2): 81-85, 90. https://www.cnki.com.cn/Article/CJFDTOTAL-CWCN201802005.htm [5] 石汉平. 营养治疗是肿瘤的一线治疗[J]. 临床药物治疗杂志, 2019, 17(4): 20-25. https://www.cnki.com.cn/Article/CJFDTOTAL-LCYW201904005.htm [6] 国家统计局国务院第七次全国人口普查领导小组办公室. 第七次全国人口普查公报([1])(第四号)[N]. 中国信息报, 2021-05-12(002). [7] 黄河浪, 徐艳, 闫骥, 等. 中国老年病的流行特点及防控对策[J]. 中国老年学杂志, 2015, 35(1): 248-251. doi: 10.3969/j.issn.1005-9202.2015.01.128 [8] LOAN B T H, NAKAHARA S, THO B A, et al. Nutritional status and postoperative outcomes in patients with gastrointestinal cancer in Vietnam: A retrospective cohort study[J]. Nutrition, 2017, 48: 117-121. [9] MATSUURA S, SAKATA Y, TSURUOKA N, et al. Outcomes of patients undergoing endoscopic hemostasis for the upper gastrointestinal bleeding were not influenced by the timing of hospital emergency visits: A situation prevailing in Japan[J]. Digestion, 2018, 97(3): 260-266. doi: 10.1159/000485653 [10] MISLANG A R, DI DONATO S, HUBBARD J, et al. Nutritional management of older adults with gastrointestinal cancers: An International Society of Geriatric Oncology (SIOG) review paper[J]. J Geriatr Oncol, 2018, 9(4): 382-392. doi: 10.1016/j.jgo.2018.01.003 [11] 李双燕, 丁轶, 冯金象, 等. 消化道恶性肿瘤患者营养状况分析及生活质量相关性研究[J]. 实用癌症杂志, 2019, 34(2): 281-284. https://www.cnki.com.cn/Article/CJFDTOTAL-SYAZ201902029.htm [12] 于恺英, 刘俐惠, 石汉平. 肿瘤营养相关状况诊断标准[J]. 肿瘤代谢与营养电子杂志, 2020, 7(1): 1-6. https://www.cnki.com.cn/Article/CJFDTOTAL-ZLDX202001001.htm [13] 陈彩文, 蔡宏飞, 常亮, 等. 术前营养风险筛查对老年食管癌患者临床结局的影响[J]. 实用癌症杂志, 2017, 32(1): 102-105. https://www.cnki.com.cn/Article/CJFDTOTAL-SYAZ201701033.htm [14] SONG C H, CAO J J, ZHANG F, et al. Nutritional risk assessment by scored patient-generated subjective global assessment associated with demographic characteristics in 23, 904 common malignant tumors patients[J]. Nutr Cancer, 2019, 71(1): 50-60. [15] 刘佐军, 李若凡, 齐辉, 等. 精氨酸和谷氨酰胺对围术期结直肠肿瘤患者免疫功能和营养状况的影响[J]. 川北医学院学报, 2017, 32(2): 175-177. https://www.cnki.com.cn/Article/CJFDTOTAL-NOTH201702006.htm [16] 宋春花, 王昆华, 郭增清, 等. 中国常见恶性肿瘤患者营养状况调查[J]. 中国科学(生命科学), 2020, 50(12): 1437-1452. https://www.cnki.com.cn/Article/CJFDTOTAL-JCXK202012006.htm [17] 王凯峰, 莫丽钦, 陈艺丹, 等. 消化系统肿瘤营养治疗的问题及对策[J]. 肿瘤学杂志, 2019, 25(8): 752-757. https://www.cnki.com.cn/Article/CJFDTOTAL-XHON201908015.htm [18] ZIETARSKA M, KRAWCZYK-LIPIEC J, KRAJ L, et al. Chemotherapy-related toxicity, nutritional status and quality of life in precachectic oncologic patients with, or without, high protein nutritional support. A prospective, randomized study[J]. Nutrients, 2017, 9(10): 1108. [19] 陈云娥, 李璠, 张子怡, 等. 营养支持治疗对终末期恶性肿瘤患者临床结局影响的Meta分析[J]. 医学信息, 2019, 32(19): 63-67. https://www.cnki.com.cn/Article/CJFDTOTAL-YXXX201919019.htm [20] 王润, 黄立锋, 刘文胜. 七氟烷吸入麻醉与靶控输注丙泊酚对老年消化道肿瘤患者术后认知功能及血液流变学的影响[J]. 实用癌症杂志, 2019, 34(7): 1185-1187. https://www.cnki.com.cn/Article/CJFDTOTAL-SYAZ201907041.htm [21] 高蓓蓓, 辛玲, 卞伟峰, 等. 个性化饮食护理在老年进展期食管癌放疗中的应用[J]. 中华全科医学, 2020, 18(12): 2144-2148. https://www.cnki.com.cn/Article/CJFDTOTAL-SYQY202012044.htm [22] 吴苏宁, 寇晓霞, 仇金荣. 老年恶性肿瘤病人的营养状况与支持治疗[J]. 实用老年医学, 2020, 34(8): 763-766, 770. https://www.cnki.com.cn/Article/CJFDTOTAL-SYLA202008003.htm -





 下载:
下载: