Clinical value of plasma adiponectin in the diagnosis of chronic heart failure
-
摘要:
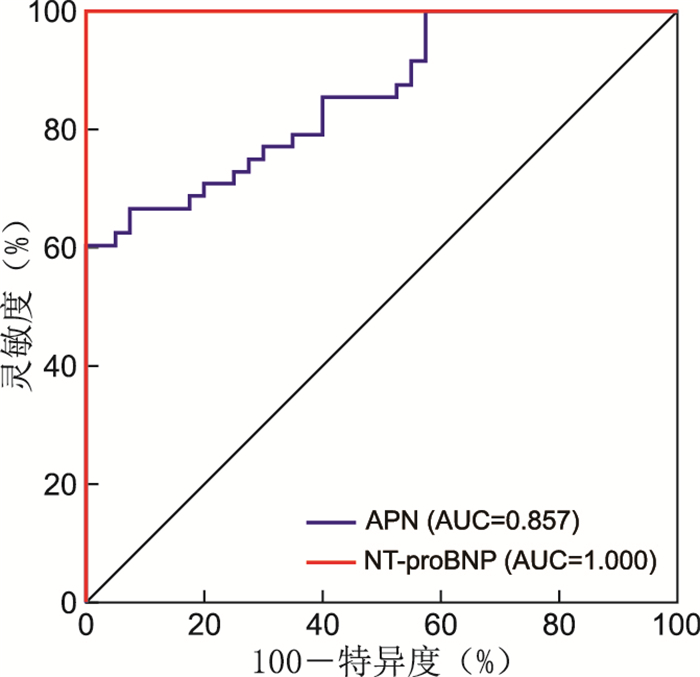
目的 探讨血浆脂联素(APN)对慢性心力衰竭(CHF)的临床诊断价值。 方法 纳入2018年5月—2019年5月在安徽省立医院确诊CHF的患者48例为CHF组及40例健康志愿者为对照组。比较2组血浆APN和氨基末端脑钠肽前体(NT-proBNP)水平,获取CHF组左室射血分数(LVEF), 分析CHF组血浆APN与NT-proBNP、LVEF的相关性。根据美国纽约心脏病协会(NYHA)心功能分级对CHF患者分组,比较不同亚组间血浆APN、NT-proBNP及LVEF。采集CHF组治疗前及治疗后3个月、6个月血浆APN、NT-proBNP及LVEF,分析APN对CHF的诊断价值。 结果 CHF组年龄为45~91(60.98±13.98)岁,男性34例,女性14例;对照组年龄为51~93(57.88±13.76)岁,男性28例,女性12例。CHF组血浆APN、NT-proBNP分别为(23.08±9.39)μg/mL、5 455.00(1 256.00, 8 552.25)pg/mL,高于对照组[(12.06±3.28)μg/mL、55.50(32.00, 78.50)pg/mL],差异有统计学意义(均P<0.05)。Pearson线性相关分析显示,CHF组血浆APN与NT-proBNP呈正相关,与LVEF呈负相关。APN、NT-proBNP随着心功能等级增加而升高,LVEF却明显降低。规范化心衰治疗后,血浆APN、NT-proBNP随着时间延长显著降低,LVEF却显著升高。 结论 CHF患者血浆APN与NT-proBNP水平呈正相关关系,与LVEF呈负相关关系,与NYHA心功能分级具有一致性,对CHF临床诊断具有一定的预测价值。 Abstract:Objective To investigate the clinical value of plasma adiponectin (APN) in the diagnosis of chronic heart failure (CHF). Methods A total of 48 patients with CHF diagnosed in Anhui Provincial Hospital from May 2018 to May 2019 were included as CHF group, and 40 healthy volunteers were included as control group. The levels of plasma APN and NT-proBNP in the two groups were compared, the left ventricular ejection fraction (LVEF) in CHF group was obtained, and the correlation between plasma APN, NT-proBNP and LVEF in CHF group was analyzed. CHF patients were divided into groups by cardiac function classification of New York Heart Association (NYHA), and plasma APN, NT-proBNP and LVEF were compared between subgroups. Plasma APN, NT-proBNP and LVEF were collected before and 3 and 6 months after treatment in CHF group, and the diagnostic value of APN in CHF was preliminarily analyzed. Results In the CHF group, the age was 45-91 (60.98±13.98) years, with 34 males and 14 females. In the control group, the age was 51-93 (57.88±13.76) years, with 28 males and 12 females. The plasma APN and NT-proBNP in the CHF group were (23.08±9.39) μg/mL, 5 455.00 (1 256.00, 8 552.25) pg/mL, respectively, which were higher than those in the control group [(12.06±3.28) μg/mL and 55.50 (32.00, 78.50) pg/mL], the differences were statistically significant (all P < 0.05). Pearson linear relationship analysis showed that the plasma APN was positively correlated with NT-pro BNP and negatively correlated with LVEF in the CHF group. The APN and NT-proBNP increased significantly with the increase of cardiac function grade, but LVEF decreased significantly. During the follow-up, the plasma APN and NT-proBNP decreased significantly with the improvement of the disease, but LVEF increased significantly. Conclusion The plasma APN is positively correlated with NT-proBNP and negatively correlated with LVEF in patients with CHF, which is consistent with NYHA cardiac function grade. It has certain predictive value for clinical diagnosis of CHF. -
表 1 治疗前CHF组和对照组患者临床资料比较
Table 1. Comparison of clinical data of patients in CHF group and control group before treatment
组别 例数 APN
(x±s, μg/mL)NT-proBNP
[M(P25, P75), pg/mL]TG
[M(P25, P75), mmol/L]HDL-C
(x±s, mmol/L)TC
(x±s, mmol/L)CHF组 48 23.08±9.39 5 455.00(1 256.00, 8 552.25) 1.14(0.85, 2.05) 0.91±0.33 3.96±1.12 对照组 40 12.06±3.28 55.50(32.00, 78.50) 1.34(0.88, 1.90) 0.93±0.24 4.01±0.95 统计量 7.072a 8.045b 0.528b 0.274a 0.261a P值 <0.001 <0.001 0.598 0.790 0.795 注:a为t值,b为Z值。 表 2 不同心功能分级CHF患者临床资料比较
Table 2. Comparison of clinical data of CHF patients with different cardiac function grades
组别 例数 性别
(男/女, 例)年龄
(x±s, 岁)APN
(x±s, μg/mL)NT-proBNP
[M(P25, P75), pg/mL]LVEF
(x±s, %)既往病史[例(%)] 高血压病 房颤 糖尿病 缺血性心肌病 Ⅱ级组 15 7/8 59.33±10.57 15.52±6.58 786.00(567.00, 1 253.00) 44.27±4.08 2(13.30) 4(26.70) 2(13.30) 3(20.00) Ⅲ级组 14 8/6 59.00±14.67 22.90±6.65 5 455.00(4 134.75, 5 692.25) 38.93±6.56 4(28.60) 6(42.90) 3(21.40) 4(28.60) Ⅳ级组 19 7/12 63.74±15.95 29.20±8.80 8 958.00(6 789.00, 13 789.00) 32.11±8.39 4(21.10) 7(36.80) 4(21.10) 5(26.30) 统计量 1.351a 0.604b 13.709b 38.105a 13.787b 1.020a 0.858a 0.421a 0.572a P值 0.509 0.551 <0.001 <0.001 <0.001 0.600 0.651 0.810 0.917 组别 例数 服用药物情况[例(%)] ACEI/ARB β受体阻滞剂 利尿剂 地高辛 胰岛素 调脂药 Ⅱ级组 15 10(66.70) 11(73.30) 14(93.30) 3(20.00) 2(13.30) 7(46.70) Ⅲ级组 14 12(85.70) 11(78.60) 13(92.90) 5(35.70) 2(14.30) 7(50.00) Ⅳ级组 19 17(89.50) 16(84.20) 18(94.70) 7(36.80) 4(21.10) 9(47.40) 统计量 2.962a 0.607a 0.056a 1.290a 0.440a 0.036a P值 0.227 0.738 0.972 0.525 0.802 0.982 注:a为χ2值,b为F值。ACEI/ARB为血管紧张素转化酶抑制剂/血管紧张素受体拮抗剂。 表 3 CHF患者治疗前后血浆APN、NT-proBNP及LVEF比较
Table 3. Comparison of plasma APN, NT-Pro BNP and LVEF in CHF patients before and after treatment
时间 APN
(x±s, μg/mL)NT-proBNP
[M(P25, P75), pg/mL]LVEF
(x±s, %)治疗前 23.08±9.39 5 455.00(1 256.00, 8 552.25) 37.90±8.40 3个月 17.72±6.09a 3 461.50(1 159.00, 4 673.00)a 42.17±7.03a 6个月 14.24±4.92ab 1 267.50(568.00, 2 196.25)ab 46.13±7.15ab 统计量 84.666c 73.358d 50.534c P值 <0.001 <0.001 <0.001 注:与治疗前比较, aP<0.05;与治疗后3个月比较, bP<0.05。c为F值,d为χ2值。 -
[1] 陈东, 苏浩, 徐健, 等. 左室心内膜起搏实现心脏再同步化治疗的临床研究[J]. 中华全科医学, 2019, 17(9): 1485-1490. doi: 10.16766/j.cnki.issn.1674-4152.000976CHEN D, SU H, XU J, et al. Clinical study of left ventricular endocardial pacing in cardiac resynchronization therapy[J]. Chinese Journal of General Practice, 2019, 17(9): 1485-1490. doi: 10.16766/j.cnki.issn.1674-4152.000976 [2] GE Z, BABER U, CLAESSEN B E, et al. The prevalence, predictors and outcomes of guideline-directed medical therapy in patients with acute myocardial infarction undergoing PCI, an analysis from the PROMETHEUS registry[J]. Catheter Cardiovasc Interv, 2019, 93(3): E112-E119. doi: 10.1002/ccd.27860 [3] HUUSKO J, KURKI S, TOPPILA I, et al. Heart failure in Finland: Clinical characteristics, mortality, and healthcare resource use[J]. ESC Heart Fail, 2019, 6(4): 603-612. doi: 10.1002/ehf2.12443 [4] GALLAGHER J, MCCORMACK D, ZHOU S W, et al. A systematic review of clinical prediction rules for the diagnosis of chronic heart failure[J]. ESC Heart Fail, 2019, 6(3): 499-508. doi: 10.1002/ehf2.12426 [5] MANTOVANI A, DANESE E, SALVAGNO G L, et al. Association between lower plasma adiponectin levels and higher plasma thrombin generation parameters in men with type 2 diabetes: Role of plasma triglycerides[J]. J Endocrinol Invest, 2021, 44(3): 547-555. doi: 10.1007/s40618-020-01340-3 [6] PUCHAŁOWICZ K, KŁODA K, DZIEDZIEJKO, et al. Association of adiponectin, leptin and resistin plasma concentrations with echocardiographic parameters in patients with coronary artery disease[J]. Diagnostics(Basel), 2021, 11(10): 1774. [7] TANAKA Y, KITA S, NISHIZAWA H, et al. Adiponectin promotes muscle regeneration through binding to T-cadherin[J]. Sci Rep, 2019, 9(1): 16. doi: 10.1038/s41598-018-37115-3 [8] BAYES-GENIS A, CEDIEL G, DOMINGO M, et al. Biomarkers in heart failure with preserved ejection fraction[J]. Card Fail Rev, 2022, 8: e20. doi: 10.15420/cfr.2021.37 [9] OH A, OKAZAKI R, SAM F, et al. Heart failure with preserved ejection fraction and adipose tissue: A story of two tales[J]. Front Cardiovasc Med, 2019, 6: 110-119. doi: 10.3389/fcvm.2019.00110 [10] GRUZDEVA O V, DYLEVA Y A, BELIK E V, et al. Relationship between epicardial and coronary adipose tissue and the expression of adiponectin, leptin, and interleukin 6 in patients with coronary artery disease[J]. J Pers Med, 2022, 12(2): 129-145. doi: 10.3390/jpm12020129 [11] LUO D L, CHEN P Y, YANG Z Y, et al. High plasma adiponectin is associated with increased pulmonary blood flow and reduced right ventricular function in patients with pulmonary hypertension[J]. BMC Pulm Med, 2020, 20(1): 204-212. doi: 10.1186/s12890-020-01233-4 [12] EMDIN M, AIMO A, VERGARO G, et al. sST2 predicts outcome in chronic heart failure beyond NT-proBNP and high-sensitivity troponin T[J]. J Am Coll Cardiol, 2018, 72(19): 2309-2320. doi: 10.1016/j.jacc.2018.08.2165 [13] JANUZZI J L, AHMAD T, MULDER H, et al. Natriuretic peptide response and outcomes in chronic heart failure with reduced ejection fraction[J]. J Am Coll Cardiol, 2019, 74(9): 1205-1217. doi: 10.1016/j.jacc.2019.06.055 [14] PAN Y S, LI D J, MA J, et al. NT-proBNP test with improved accuracy for the diagnosis of chronic heart failure[J]. Medicine, 2017, 96(51): e9181-e9187. doi: 10.1097/MD.0000000000009181 [15] STIENEN S, SALAH K, MOONS A H, et al. NT-proBNP (N-terminal pro-B-type natriuretic peptide)-guided therapy in acute decompensated heart failure: PRIMA Ⅱ randomized controlled trial (can NT-ProBNP-guided therapy during hospital admission for acute decompensated heart failure reduce mortality and readmissions?)[J]. Circulation, 2018, 137(16): 1671-1683. doi: 10.1161/CIRCULATIONAHA.117.029882 [16] HORBAL S R, HALL M E, DINH P C, et al. Associations of adiponectin and leptin with brain natriuretic peptide in African Americans: The Jackson heart study[J]. Cardiovasc Endocrinol Metab, 2020, 9(2): 49-55. doi: 10.1097/XCE.0000000000000198 [17] WANG H, GAO Y X, WU Y N, et al. Association between plasma adiponectin levels and left ventricular systolic dysfunction in sepsis patients[J]. J Crit Care, 2020, 60: 195-201. doi: 10.1016/j.jcrc.2020.06.020 [18] VAN BERENDONCKS A M, BECKERS P, HOYMANS V Y, et al. β-blockers modify the prognostic value of adiponectin in chronic heart failure[J]. Int J Cardio, 2011, 150(3): 296-300. doi: 10.1016/j.ijcard.2010.04.039 -





 下载:
下载: