Factors associated with taking antihypertensive traditional Chinese medicine only among community-dwelling middle-aged and elderly adults
-
摘要:
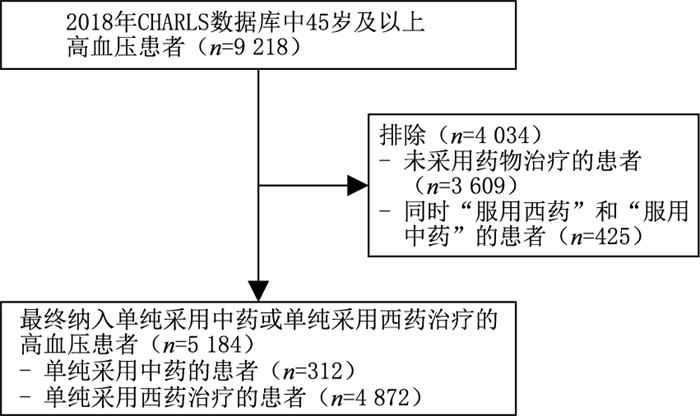
目的 分析我国社区中老年高血压用药群体单纯采用中药治疗的影响因素。 方法 利用CHARLS(2018)数据库,以正在接受单纯中药或单纯西药治疗的社区45岁及以上高血压患者为研究对象,采用多因素logistic回归分析,对单纯采用中药治疗的相关因素进行分析。 结果 研究共纳入5 184名单纯采用中药或西药治疗的高血压患者,其中312人仅接受中药治疗,4 872人仅接受西药治疗。使用其他医疗保险患者单纯采用中药治疗是无医疗保险患者的0.347倍;> 000~7 000经济发展区域患者单纯采用中药治疗是000以上经济发展区域患者的3.197倍;BMI显示肥胖患者单纯采用中药治疗是BMI正常患者的0.629倍;自报健康状况很不好的患者单纯采用中药治疗是自报健康状况很好患者的0.331倍;患有3种以上其他慢性病患者单纯采用中药治疗是无高血压之外其他慢性病患者的0.167倍;正在接受其他疾病中药治疗的患者是未接受其他疾病中药治疗患者单纯采用中药的7.271倍。 结论 位于中低经济发展区域、BMI正常、自报健康状况良好、无高血压之外其他慢性病以及正在接受其他中药治疗的患者与其他类型的患者相比,更倾向单纯采用中药治疗高血压。今后,需进一步前瞻性地观察中药和西药2组用药者心脑血管终点事件结局改善的差异,为高血压中药治疗提供更高级别质量的证据。 Abstract:Objective To investigate the factors associated with antihypertensive traditional Chinese medicine (TCM) intake only among community-dwelling middle-aged and elderly adults in China. Methods The analysis was based on the national representative China Health and Retirement Longitudinal Study (CHARLS) in 2018. Community-dwelling adults aged 45 years old or above and who were either taking TCM or western modern medicine (WMM) only were included. Multivariate logistic regression analysis was used to examine the factors associated with taking TCM only for hypertension. Results A total of 5 184 patients with hypertension were included, including 312 TCM and 4 872 WMM users. The odds of patients with other types of medical insurances and who used TCM alone was 0.347 times that of patients without medical insurance. The odds of patients in economic development areas of > 000-7 000 and who used TCM alone was 3.197 times that of patients in economic development areas above 000. The odds of obese patients were 0.629 times more than the patients with normal body mass index and who used TCM alone. The odds of patients with self-reported very poor health status and who used TCM alone was 0.331 times that of patients who self-reported very good health status. The odds of patients with more than three types of chronic diseases were 0.167 times more than those with hypertension and used TCM alone. The odds of patients who received TCM for other diseases was 7.271 times that of patients used TCM alone and who were not receiving TCM for other diseases. Conclusions Patients in the middle or deprived economic development region, with very good self-reported health status, without other diagnosed chronic disease and under TCM treatment for other diseases are more likely to take TCM for hypertension compared with other patients. In the future, it is necessary to further prospectively observe the difference in the improvement of cardiovascular and cerebrovascular end point outcomes between the two groups of TCM and WMM, so as to provide higher quality evidence for the treatment of hypertension with TCM. -
表 1 纳入的5 184名社区45岁及以上高血压用药患者基本信息分布情况[例(%)]
Table 1. Basic characteristics of the included 5184 community participants at the age of 45 or above with hypertension by medication treatment types[cases(%)]
项目 单纯采用中药(n=312) 单纯采用西药(n=4 872) 年龄 45~54岁 54(17.3) 769(15.8) 55~64岁 93(29.8) 1 507(30.9) 65~74岁 102(32.7) 1 697(34.8) 75~84岁 54(17.3) 752(15.4) 85岁及以上 9(2.9) 147(3.0) 性别 男性 172(55.1) 2 199(45.1) 女性 140(44.9) 2 673(54.9) 户籍a 乡村 182(58.3) 2 789(57.2) 城镇 130(41.7) 2 074(42.6) 教育程度 小学及以下 216(69.2) 3 345(68.7) 中学或中专 91(29.2) 1 427(29.3) 大专及以上 5(1.6) 100(2.1) 医疗保险 无 14(4.5) 112(2.3) 城镇职工医疗保险 50(16.0) 757(15.5) 城镇居民医疗保险 24(7.7) 227(4.7) 新型农村合作医疗保险 186(59.6) 3 006(61.7) 其他医疗保险 38(12.2) 770(15.8) 经济发展区域a >$12 000 28(9.0) 858(17.6) >$10 000~12 000 58(18.6) 955(19.6) >$7 000~10 000 158(50.6) 2 294(47.1) >$6 000~7 000 39(12.5) 397(8.1) ≤$6 000 29(9.3) 359(7.4) BMIa < 18.5(低体重) 9(2.9) 153(3.1) 18.5~23.9(正常) 98(31.4) 1 281(26.3) 24.0~27.9(超重) 81(26.0) 1 496(30.7) ≥28.0(肥胖) 42(13.5) 848(17.4) 自报健康状况a 很好 30(9.6) 297(6.1) 好 20(6.4) 377(7.7) 一般 144(46.2) 2 086(42.8) 不好 68(21.8) 1 298(26.6) 很不好 20(6.4) 398(8.2) 患高血压之外的其他慢性病数量 无 81(26.0) 1 110(22.8) 1~3种 197(63.1) 3 012(61.8) 3种以上 34(10.9) 750(15.4) 正在接受其他疾病的中药治疗 否 143(45.8) 3 876(79.6) 是 169(54.2) 996(20.4) 血压测量频次 ≤3个月1次 273(87.5) 3 952(81.1) >3个月1次 39(12.5) 920(18.9) 注:a观测的变量包括缺失值。 表 2 高血压中老年用药患者单纯采用中药治疗影响因素的多因素二项logistic回归分析
Table 2. Multivariate logistic regression analyses of only under traditional Chinese medicine treatment among middle-aged and older patients who are under antihypertensive drug treatment
变量 B SE Wald χ2 P值 OR(95% CI) 性别(女性) -0.284 0.149 3.627 0.057 0.753(0.563~1.008) 医疗保险 城镇职工医疗保险 -0.625 0.433 2.079 0.149 0.535(0.229~1.252) 城镇居民医疗保险 0.058 0.478 0.015 0.902 1.060(0.415~2.707) 新型农村合作医疗保险 -0.567 0.391 2.109 0.146 0.567(0.264~1.219) 其他医疗保险 -1.058 0.442 5.742 0.017 0.347(0.146~0.825) 经济发展区域 >$10 000~12 000 0.763 0.300 6.441 0.011 2.144(1.190~3.863) >$7 000~10 000 0.658 0.274 5.779 0.016 1.930(1.129~3.298) >$6 000~7 000 1.162 0.325 12.811 < 0.001 3.197(1.692~6.041) ≤$6 000 0.706 0.348 4.126 0.042 2.026(1.025~4.003) BMI < 18.5(低体重) -0.396 0.420 0.890 0.345 0.673(0.296~1.532) 24.0~27.9(超重) -0.437 0.168 6.772 0.009 0.646(0.465~0.898) ≥28.0(肥胖) -0.464 0.204 5.174 0.023 0.629(0.422~0.938) 自报健康状况 好 -0.812 0.345 5.537 0.019 0.444(0.225~0.873) 一般 -0.589 0.241 5.982 0.015 0.555(0.346~0.889) 不好 -0.955 0.278 11.754 0.001 0.385(0.223~0.665) 很不好 -1.106 0.372 8.807 0.003 0.331(0.160~0.687) 患高血压之外其他慢性疾病的数量 1~3种 -0.835 0.210 15.875 < 0.001 0.434(0.288~0.654) 3种以上 -1.790 0.331 29.225 < 0.001 0.167(0.087~0.320) 正在接受其他疾病的中药治疗 1.984 0.185 115.402 < 0.001 7.271(5.063~10.441) 血压测量频次>3个月1次 -0.350 0.203 2.961 0.085 0.705(0.474~1.050) 注:性别以“男性”为参照,医疗保险以“无”为参照,经济发展区域以“$12 000以上”为参照,BMI以“18.5~23.9(正常)”为参照,自报健康状况以“很好”为参照,患高血压之外其他慢性疾病的数量以“无”为参照,正在接受其他疾病的中药治疗以“否”为参照,血压测量频次以“≤3个月1次”为参照。Logistic回归模型板正的因素如下,性别、医疗保险类型、经济发展区域、BMI、自报健康状况、患高血压之外其他慢性疾病的数量、是否正在接受其他疾病的中药治疗以及血压测量频次。 -
[1] TSCHANZ C M P, CUSHMAN W C, HARRELL C T E, et al. Synopsis of the 2020 U.S. Department of Veterans Affairs/U.S. Department of Defense Clinical Practice Guideline: The diagnosis and management of hypertension in the primary care setting[J]. Ann Intern Med, 2020, 173(11): 904-913. doi: 10.7326/M20-3798 [2] LU J P, LU Y, WANG X C, et al. Prevalence, awareness, treatment, and control of hypertension in China: Data from 1·7 million adults in a population-based screening study (China PEACE Million Persons Project)[J]. Lancet, 2017, 390(10112): 2549-2558. doi: 10.1016/S0140-6736(17)32478-9 [3] BAKRIS G, ALI W, PARATI G. ACC/AHA versus ESC/ESH on hypertension guidelines: JACC guideline comparison[J]. J Am Coll Cardiol, 2019, 73(23): 3018-3026. doi: 10.1016/j.jacc.2019.03.507 [4] 国家心血管病中心国家基本公共卫生服务项目基层高血压管理办公室, 国家基层高血压管理专家委员会. 国家基层高血压防治管理指南2020版[J]. 中国循环杂志, 2021, 36(3): 209-220. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGXH202103001.htmThe National Essential Public Health Service Program Office for Management of Hypertension in Primary Health Care. National Clinical Practice Guidelines on the Management of Hypertension in Primary Health Care in China (2020)[J]. Chinese Circulation Journal, 2021, 36(3): 209-220. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGXH202103001.htm [5] 刘芬, 何毅芳, 谢凡慈, 等. 高血压病患者中医体质特点与心血管疾病危险因素的关联分析[J]. 医学理论与实践, 2021, 34(2): 222-224. https://www.cnki.com.cn/Article/CJFDTOTAL-YXLL202102020.htmLIU F, HE Y F, XIE F C, et al. Correlation analysis between TCM constitution characteristics and cardiovascular disease risk factors in hypertensive patients[J]. Medical Theory and Practice, 2021, 34(2): 222-224. https://www.cnki.com.cn/Article/CJFDTOTAL-YXLL202102020.htm [6] 赵倩倩, 李媛媛, 陈聪, 等. 中医药治疗原发性高血压的作用机制研究现状与展望[J]. 中华中医药杂志, 2020, 35(4): 1914-1916. https://www.cnki.com.cn/Article/CJFDTOTAL-BXYY202004080.htmZHAO Q Q, LI Y Y, CHEN C, et al. Current situation and prospect of the research on the mechanism of TCM in treating essential hypertension[J]. China Journal of Traditional Chinese Medicine and Pharmacy, 2020, 35(4): 1914-1916. https://www.cnki.com.cn/Article/CJFDTOTAL-BXYY202004080.htm [7] 黄传应, 杨荣, 廖晓阳. 家庭社会支持对高血压治疗依从性影响的研究进展[J]. 中华全科医学, 2021, 19(3): 466-470. doi: 10.16766/j.cnki.issn.1674-4152.001837HUANG C Y, YANG R, LIAO X Y. Effects of family social support on treatment compliance of patients with hypertension[J]. Chinese Journal of General Practice, 2021, 19(3): 466-470. doi: 10.16766/j.cnki.issn.1674-4152.001837 [8] ZHAO Y H, HU Y S, SMITH J P, et al. Cohort profile: The China health and retirement longitudinal study (CHARLS)[J]. Int J Epidemiol, 2014, 43(1): 61-68. doi: 10.1093/ije/dys203 [9] VON ELM E, ALTMAN D G, EGGER M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies[J]. PLoS Med, 2007, 4(10): e296. DOI: 10.1371/journal.pmed.0040296. [10] 中国高血压防治指南修订委员会. 中国高血压防治指南(2018年修订版)[J]. 中国心血管杂志, 2019, 24(1): 24-56. doi: 10.3969/j.issn.1007-5410.2019.01.002Writing Group of 2018 Chinese Guidelines for the Management of Hypertension. 2018 Chinese guidelines for the management of hypertension[J]. Chin J Cardiovasc Med, 2019, 24(1): 24-56. doi: 10.3969/j.issn.1007-5410.2019.01.002 [11] ZHAO Y, ATUN R, OLDENBURG B, et al. Physical multimorbidity, health service use, and catastrophic health expenditure by socioeconomic groups in China: An analysis of population-based panel data[J]. Lancet Glob Health, 2020, 8(6): e840-e849. DOI: 10.1016/S2214-109X(20)30127-3. [12] WANG Z W, CHEN Z, ZHANG L F, et al. Status of hypertension in China: Results from the China hypertension survey, 2012-2015[J]. Circulation, 2018, 137(22): 2344-2356. doi: 10.1161/CIRCULATIONAHA.117.032380 [13] 郑晨霞, 沈建平. 中医药治疗高血压研究进展[J]. 中医研究, 2021, 34(2): 57-60. https://www.cnki.com.cn/Article/CJFDTOTAL-ZYYJ202102020.htmZHENG C X, SHEN J P. Research progress in TCM treatment of hypertension[J]. Traditional Chinese Medicine Research, 2021, 34(2): 57-60. https://www.cnki.com.cn/Article/CJFDTOTAL-ZYYJ202102020.htm [14] WANG Y X, PENG X X, NIE X L, et al. Burden of hypertension in China over the past decades: Systematic analysis of prevalence, treatment and control of hypertension[J]. Eur J Prev Cardiol, 2016, 23(8): 792-800. [15] HAO P P, JIANG F, CHENG J, et al. Traditional Chinese medicine for cardiovascular disease: Evidence and potential mechanisms[J]. J Am Coll Cardiol, 2017, 69(24): 2952-2966. [16] ZHANG D Y, CHENG Y B, GUO Q H, et al. Treatment of masked hypertension with a Chinese herbal formula: A randomized, placebocontrolledtrial[J]. Circulation, 2020, 142(19): 1821-1830. [17] 王娅, 刘艳飞, 王哲, 等. 2015-2019年中药治疗原发性高血压的系统评价再评价[J]. 中国循证医学杂志, 2019, 19(12): 1460-1469. https://www.cnki.com.cn/Article/CJFDTOTAL-ZZXZ201912013.htmWANG Y, LIU Y F, WANG Z, et al. Traditional Chinese medicine treatment for essential hypertension from 2015 to 2019: an overview of systematic reviews[J]. Chinese Journal of Evidence-based Medicine, 2019, 19(12): 1460-1469. https://www.cnki.com.cn/Article/CJFDTOTAL-ZZXZ201912013.htm [18] 周晓丽, 刘曼玲, 焦艳会. 多种慢性病管理模式在社区老年高血压患者中的综合应用与评价[J]. 中华全科医学, 2020, 18(3): 449-453. doi: 10.16766/j.cnki.issn.1674-4152.001270ZHAOU X L, LIU M L, JIAO Y H. Comprehensive application and evaluation of multiple chronic disease management models in elderly patients with hypertension in community[J]. Chinese Journal of General Practice, 2020, 18(3): 449-453. doi: 10.16766/j.cnki.issn.1674-4152.001270 [19] 张晓娟, 李子锋, 张珺, 等. 常规护理联合多种中医护理技术干预肝阳上亢型高血压合并失眠效果的网状Meta分析[J]. 循证护理, 2020, 6(12): 1285-1291. https://www.cnki.com.cn/Article/CJFDTOTAL-XZHL202012004.htmZHANG X J, LI Z F, ZHANG J, et al. Network Meta-analysis of routine nursing combined with multiple traditional Chinese medicine nursing technology in hypertension patients with hyperactivity of liver-Yang combined with insomnia[J]. Chinese Evidence-based Nursing, 2020, 6(12): 1285-1291. https://www.cnki.com.cn/Article/CJFDTOTAL-XZHL202012004.htm -





 下载:
下载: