Research on quantitative or semi-quantitative assessment of placental function in pationts with hypertension of pregnancy by dual-mode ultrasound
-
摘要:
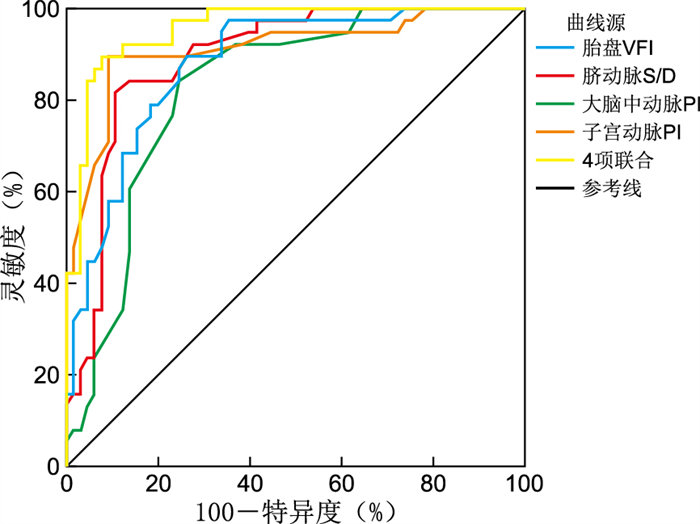
目的 探讨双模态超声定量或半定量评价妊娠高血压患者胎盘功能的价值。 方法 选取宿州市立医院2018年1月—2021年6月接诊的163例孕妇,孕周为30~41周,其中103例为妊娠高血压疾病患者(重度子痫前期38例、子痫前期65例),60例为正常妊娠孕妇。采用三维能量多普勒超声监测胎盘血流充盈,获取胎盘能量直方图[胎盘血管指数(VI)、血流指数(FI)、血管血流指数(VFI)],采用频谱多普勒超声监测胎儿脐动脉、大脑中动脉、孕妇子宫动脉频谱[搏动指数(PI)、阻力指数(RI)、收缩期/舒张期血流比值(S/D)]。 结果 随着病情进展,妊娠高血压疾病患者的三维能量胎盘血流充盈直方图数据(VI、FI、VFI)降低,差异均有统计学意义(均P<0.05);胎儿脐动脉血流频谱(PI、RI、S/D)增高,差异均有统计学意义(均P<0.05);胎儿大脑中动脉血流频谱(PI、RI、S/D)降低,差异均有统计学意义(均P<0.05);孕妇子宫动脉血流频谱(PI、RI、S/D)增高,差异均有统计学意义(均P<0.05)。ROC曲线分析显示,胎儿脐动脉S/D、大脑中动脉PI、孕妇子宫动脉频谱PI和直方图数据VFI对子痫前期/重度子痫前期具有较高的诊断价值(AUC=0.893、0.827、0.912、0.880,均P<0.05),且4项联合检测诊断价值最高(AUC=0.957,P<0.05);得出截断值,孕30周后当脐动脉S/D高于3.010,大脑中动脉PI低于1.575,子宫动脉PI高于1.215,胎盘VFI低于4.755时诊断妊娠高血压疾病胎盘功能受损有较高的灵敏度及特异度。 结论 双模态超声成像可以定量或半定量分析胎盘血流灌注变化,为临床评估妊娠高血压疾病患者的胎盘功能提供指导意见。 Abstract:Objective To explore the value of dual-modal ultrasound in quantitative or semi-quantitative evaluation of placental function in patients with hypertension of pregnancy. Methods A total of 163 pregnant women admitted to Suzhou Municipal Hospital from January 2018 to June 2021 were selected, and their gestational weeks were 30-41 weeks. Among them, 103 were patients with hypertension in pregnancy (38 cases of severe preeclampsia, 65 cases of preeclampsia), and 60 were normal pregnant women. The placental blood flow filling was monitored by three-dimensional power Doppler ultrasound, and placental energy histograms (VI, FI, VFI) were obtained. The fetal umbilical artery, middle cerebral artery, maternal uterine artery spectrum (PI, RI, S/D) were monitored by spectral Doppler ultrasound. Results With the disease progresses, three-dimensional power placental blood flow filling histogram data (VI, FI, VFI) of patients with hypertension of pregnancy decreased (P < 0.05), the fetal umbilical artery blood flow spectrum (PI, RI, S/D) increased (P < 0.05), the fetal middle cerebral artery blood flow spectrum (PI, RI, S/D) decreased (P < 0.05), and the pregnant women' s uterine artery blood flow spectrum (PI, RI, S/D) increased (P < 0.05). The ROC curve analysis found that monitor fetal umbilical artery S/D, middle cerebral artery PI, maternal uterine artery spectrum PI and energy histograms VFI had high diagnostic value for severe preeclampsia/preeclampsia (AUC=0.893, 0.827, 0.912, 0.880, all P < 0.05), and the diagnostic value of combined detection of the four was the highest (AUC=0.957, P < 0.05). After 30 weeks of gestation, when umbilical artery S/D was higher than 3.010, middle cerebral artery PI was lower than 1.575, uterine artery PI was higher than 1.215, placental VFI was lower than 4.755, there was a high sensitivity and specificity in the diagnosis of impaired placental function in gestational hypertension. Conclusion Dual-modal ultrasound imaging can quantitatively or semi-quantitatively analyze the changes of placental blood perfusion, and provide guidance for clinical evaluation of placental function in patients with hypertension of pregnancy. -
表 1 3组胎儿脐动脉PI、RI、S/D参数比较(x±s)
Table 1. Comparison of PI, RI and S/D parameters of fetal umbilical artery in three groups
组别 例数 PI RI S/D 对照组 60 0.75±0.02 0.56±0.02 2.41±0.27 子痫前期 65 0.84±0.05ab 0.62±0.03ab 2.75±0.27ab 重度子痫前期 38 0.87±0.04a 0.66±0.04a 3.20±0.24a F值 106.588 122.770 101.654 P值 <0.001 <0.001 <0.001 注:与对照组比较,aP < 0.001;与重度子痫前期组比较,bP < 0.001。 表 2 3组孕妇子宫动脉PI、RI、S/D参数比较(x±s)
Table 2. Comparison of uterine artery PI, RI and S/D parameters between the three groups(x±s)
组别 例数 PI RI S/D 对照组 60 0.83±0.12 0.45±0.03 4.44±0.26 子痫前期 65 1.13±0.06ab 0.51±0.02ab 5.27±0.25ab 重度子痫前期 38 1.28±0.09a 0.57±0.02a 5.77±0.40a F值 290.239 199.115 246.112 P值 <0.001 <0.001 <0.001 注:与对照组比较,aP < 0.001;与重度子痫前期组比较,bP < 0.001。 表 3 3组胎儿大脑中动脉PI、RI、S/D参数比较(x±s)
Table 3. Comparison of PI, RI and S/D parameters of fetal middle cerebral artery between the three groups(x±s)
组别 例数 PI RI S/D 对照组 60 1.65±0.02 0.82±0.03 5.62±0.34 子痫前期 65 1.59±0.04ab 0.78±0.03ab 5.40±0.39ab 重度子痫前期 38 1.53±0.03a 0.74±0.02a 5.07±0.37a F值 116.498 71.763 25.893 P值 <0.001 <0.001 <0.001 注:与对照组比较,aP < 0.001;与重度子痫前期组比较,bP < 0.001。 表 4 3组孕妇直方图VI、FI、VFI参数比较(x±s)
Table 4. Parameter comparison of VI, FI and VFI of three groups of histograms(x±s)
组别 例数 VI FI VFI 对照组 60 18.66±2.08 38.19±2.49 7.94±0.51 子痫前期 65 14.31±2.04ab 36.33±1.65ab 5.01±0.32ab 重度子痫前期 38 11.27±1.40a 34.48±1.42a 4.53±0.22a F值 181.407 42.262 1 231.937 P值 <0.001 <0.001 <0.001 注:与对照组比较,aP < 0.001;与重度子痫前期组比较,bP < 0.001。 表 5 脐动脉S/D、大脑中动脉PI、子宫动脉PI、胎盘VFI参数及其联合检测诊断价值分析
Table 5. Umbilical artery S/D, middle cerebral artery PI, uterine artery PI, placental VFI parameters and their combined diagnostic value analysis
指标 Cut-off值 灵敏度(%) 特异度(%) 约登指数 AUC 脐动脉S/D 3.010 81.6 89.2 0.708 0.893 大脑中动脉PI 1.575 75.4 84.2 0.596 0.827 子宫动脉PI 1.215 89.5 90.8 0.803 0.912 胎盘VFI 4.755 73.8 89.5 0.633 0.880 4项联合 89.5 92.3 0.818 0.957 -
[1] 林杨, 闵红, 周浩泉, 等. 早产儿颅内出血的影响因素分析[J]. 中华全科医学, 2021, 19(8): 1326-1329. doi: 10.16766/j.cnki.issn.1674-4152.002052LIN Y, MIN H, ZHOU H Q, et al. Influencing factors analysis of intracranial hemorrhage in premature infants[J]. Chinese Journal of General Practice, 2021, 19(8): 1326-1329. doi: 10.16766/j.cnki.issn.1674-4152.002052 [2] 王晰. 妊娠高血压综合征的临床分析[J]. 中国实用医药, 2018, 13(34): 84-85. https://www.cnki.com.cn/Article/CJFDTOTAL-ZSSA201834043.htmWANG X. Clinical analysis of pregnancy hypertension syndrome[J]. China Practical Medicine, 2018, 13(34): 84-85. https://www.cnki.com.cn/Article/CJFDTOTAL-ZSSA201834043.htm [3] 谢幸, 孔北华, 段涛. 妇产科学[M]. 9版. 北京: 人民卫生出版社, 2018: 66.XIE X, KONG B H, DUAN T. Gynecology and Obstetrics[M]. 9th Ed. Beijing: People's Medical Publishing House, 2018: 66. [4] 毕石磊, 张丽姿, 杜丽丽, 等. 早发型与晚发型子痫前期的临床特点及母儿结局分析[J]. 中华产科急救电子杂志, 2021, 10(2): 96-100. doi: 10.3877/cma.j.issn.2095-3259.2021.02.007BI S L, ZHANG L Z, DU L L, et al. The clinical characteristics and maternal and neonatal outcomes of early and late onset preeclampsia[J]. Chinese Journal of Obstetric Emergency(Electronic Edition), 2021, 10(2): 96-100. doi: 10.3877/cma.j.issn.2095-3259.2021.02.007 [5] 闻磊, 袁平. 探讨定量三维能量多普勒超声在评估妊高症产妇药物治疗效果中的应用价值[J]. 齐齐哈尔医学院学报, 2020, 41(5): 567-570. doi: 10.3969/j.issn.1002-1256.2020.05.013WEN L, YUAN P. The value of quantitative three-dimensional power Doppler ultrasound in assessing the efficacy of drugtreatment for puerpera with pregnancy-induced hypertension[J]. Journal of Qiqihar Medical University, 2020, 41(5): 567-570. doi: 10.3969/j.issn.1002-1256.2020.05.013 [6] 伍嘉琳, 黎巧儿, 张红环, 等. 中孕期利用三维能量多普勒测量胎盘体积及血流预测晚孕期妊高症的价值探讨[J]. 包头医学院学报, 2019, 35(6): 42-44. https://www.cnki.com.cn/Article/CJFDTOTAL-BTYX201906016.htmWU J L, LI Q E, ZHANG H H, et al. Clinical value of placental volume and vascularization with three-dimensional power Doppler ultrasound at the second trimester in prediction of late-onset pregnancy-induced hypertension[J]. Journal of Baotou Medical College, 2019, 35(6): 42-44. https://www.cnki.com.cn/Article/CJFDTOTAL-BTYX201906016.htm [7] 陈艳霞, 史妙丽, 杨璞, 等. 三维能量多普勒超声对晚孕期胎盘植入的临床价值及符合率分析[J]. 影像研究与医学应用, 2021, 5(11): 93-94. doi: 10.3969/j.issn.2096-3807.2021.11.045CHEN Y X, SHI M L, YANG P, et al. Clinical value and compliance of three-dimensional energy Doppler ultrasound in placenta implantation during late pregnancy[J]. Journal of Imaging Research and Medical Applications, 2021, 5(11): 93-94. doi: 10.3969/j.issn.2096-3807.2021.11.045 [8] CARADEUX J, MARTINEZ-PORTILLA R J, BASUKI T R, et al. Risk of fetal death in growth-restricted fetuses with umbilical and/or ductus venosus absent or reversed end-diastolic velocities before 34 weeks of gestation: A systematic review and meta-analysis[J]. Am J Obstet Gynecol, 2018, 218(2): 774-782. doi: 10.1016/j.ajog.2017.11.566 [9] 张婷婷, 金镇. 脐动脉血流异常的诊治现状[J]. 中国医药科学, 2021, 11(11): 51-54, 105. doi: 10.3969/j.issn.2095-0616.2021.11.014ZHANG T T, JIN Z. Status quo of diagnosis and treatment of abnormal umbilical artery blood flow[J]. China Medicine And Pharmacy, 2021, 11(11): 51-54, 105. doi: 10.3969/j.issn.2095-0616.2021.11.014 [10] 刘和时, 朱永胜. 血管多普勒超声预测不良妊娠结局[J]. 中国医学影像技术, 2021, 37(1): 147-150. https://www.cnki.com.cn/Article/CJFDTOTAL-ZYXX202101041.htmLIU H S, ZHU Y S. Vascular Doppler ultrasound in predicting adverse pregnancy outcome[J]. Chinese Journal of Medical Imaging Technology, 2021, 37(1): 147-150. https://www.cnki.com.cn/Article/CJFDTOTAL-ZYXX202101041.htm [11] 孟菲, 杨柳, 杨娜, 等. 大脑中动脉与静脉导管血流指数联合随机尿蛋白/肌酐比值预测妊娠高血压孕妇胎儿宫内缺氧的价值[J]. 中国医药, 2020, 15(11): 1761-1764. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGYG202011026.htmMENG F, YANG L, YANG N, et al. The value of middle cerebral artery and ductus venosus blood flow index combined with random urine albumin/creatinine ratio on predicting fetus intrauterine hypoxia in pregnant woman with gestational hypertension[J]. China Medicine, 2020, 15(11): 1761-1764. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGYG202011026.htm [12] 蔡婷婷, 徐亚芬, 刘明松. 彩超预测妊娠期高血压疾病胎儿宫内窘迫的价值[J]. 中国妇幼健康研究, 2021, 32(6): 900-904. https://www.cnki.com.cn/Article/CJFDTOTAL-SANE202106025.htmCAI T T, XU Y F, LIU M S. Value of color Doppler ultrasonography in predicting intrauterine fetal distress in hypertensive disorder complicating pregnancy[J]. Chinese Journal of Woman and Child Health Research, 2021, 32(6): 900-904. https://www.cnki.com.cn/Article/CJFDTOTAL-SANE202106025.htm [13] 严宝妹, 蔡款, 刘韬, 等. 妊娠早期子宫动脉血流动力学参数对抗磷脂综合征患者妊娠结局的预测价值[J]. 中国超声医学杂志, 2022, 38(5): 554-557. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGCY202205020.htmYAN B M, CAI K, LIU T, et al. Value of Early Pregnancy Uterine Artery Doppler Hemodynamic Parameters in Predicting Pregnancy Outcome in Patients with Antiphospholipid Syndrome[J]. Chinese Journal of Ultrasound in Medicine, 2022, 38(5): 554-557. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGCY202205020.htm [14] 罗晓婷, 晁玥, 尚小轶, 等. 孕早、中、晚期子宫动脉频谱对预测妊娠高血压的价值[J]. 贵州医药, 2019, 43(7): 1084-1086. https://www.cnki.com.cn/Article/CJFDTOTAL-GZYI201907029.htmLUO X T, CHAO D, SHANG X Y, et al. Value of uterine artery spectrum in predicting pregnancy-induced hypertension in early, middle and late trimesters[J]. Guizhou Medical Journal, 2019, 43(7): 1084-1086. https://www.cnki.com.cn/Article/CJFDTOTAL-GZYI201907029.htm [15] 莫莉, 田菁菁. 多普勒超声对高危妊娠子宫-胎儿-胎盘循环的监测价值分析[J]. 中国实用医药, 2021, 16(21): 49-52. https://www.cnki.com.cn/Article/CJFDTOTAL-ZSSA202121018.htmMO L, TIAN J J. Value analysis of Doppler ultrasonography in monitoring uterine-fetal-placental circulation in high-risk pregnancy[J]. China Practical Medicine, 2021, 16(21): 49-52. https://www.cnki.com.cn/Article/CJFDTOTAL-ZSSA202121018.htm [16] KULIDA L V, MALYSHEVA M V, PERETYATKO L P, et al. Morphopathology of myocardial hypoxic-ischemic injuries in newborn at 22-27 weeks ' gestation[J]. Arkhiv Patologii, 2021, 83(4): 29. [17] 郭旭, 孙安毅. 子宫动脉超声多普勒血流监测在妊娠晚期高血压疾病的应用效果[J]. 中国医疗器械信息, 2020, 26(23): 73-74, 138. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGQX202023033.htmGUO X, SUN A Y. The Application Effect of Uterine Artery Doppler Ultrasound Blood Flow Monitoring on Hypertension in the Third Trimester of Pregnancy[J]. China Medical Device Information, 2020, 26(23): 73-74, 138. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGQX202023033.htm [18] 张丽梅. 孕期子宫动脉血流多普勒超声监测在高危妊娠中的应用[J]. 中外医疗, 2020, 39(30): 189-191. https://www.cnki.com.cn/Article/CJFDTOTAL-HZZZ202030073.htmZHANG L M. Application of Doppler Ultrasound Monitoring of Uterine Artery Blood Flow in High-risk Pregnancies[J]. China & Foreign Medical Treatment, 2020, 39(30): 189-191. https://www.cnki.com.cn/Article/CJFDTOTAL-HZZZ202030073.htm -





 下载:
下载: