Prediction of lymph node metastasis in early cervical cancer by MRI combined with preoperative serological indices and pathological features
-
摘要:
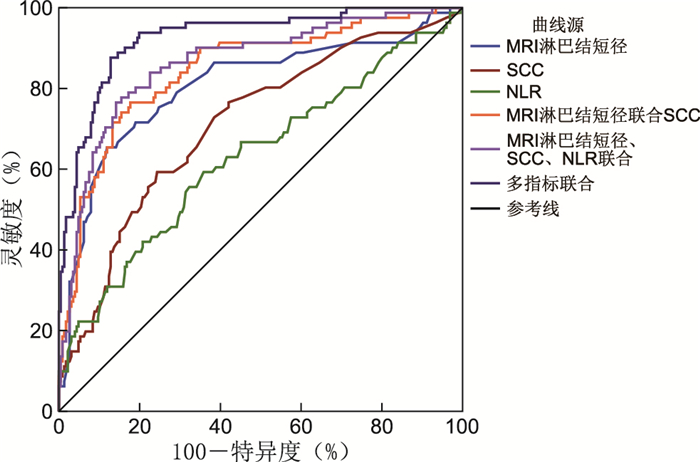
目的 探讨MRI与术前血清学指标鳞状细胞癌抗原(SCC-Ag)、中性粒细胞与淋巴细胞比值(NLR)及活检病理联合对早期宫颈癌淋巴结转移(LNM)的预测价值。 方法 选取2019年1月—2022年2月在蚌埠医学院第一附属医院行初次手术的宫颈癌患者307例,按术后病理是否存在淋巴结转移分为淋巴结转移组81例和未转移组226例,比较2组患者的MRI淋巴结短径、肿瘤直径、间质浸润深度、宫旁浸润和阴道受累,术前血清学指标以及病理特征。分析联合诊断对淋巴结转移的预测价值。 结果 Logistic回归分析显示MRI淋巴结短径大、MRI肿瘤直径大、MRI间质浸润深度>1/2肌层、MRI宫旁浸润、术前SCC-Ag水平升高和脉管浸润是宫颈癌淋巴结转移的独立危险因素(均P < 0.05)。MRI淋巴结短径、术前SCC-Ag水平、NLR诊断宫颈癌LNM的ROC曲线下面积分别为0.806、0.711、0.630,最佳截断值分别为8.50 mm、2.55 ng/mL、1.90,灵敏度分别为0.654、0.593、0.593,特异度分别为0.881、0.757、0.642;MRI淋巴结短径联合SCC-Ag诊断的ROC曲线下面积为0.846;MRI淋巴结短径、术前SCC-Ag水平、NLR三者联合诊断的ROC曲线下面积为0.863。多指标(术前SCC-Ag水平、MRI淋巴结短径、肿瘤直径、间质浸润深度、宫旁浸润以及脉管浸润)联合诊断宫颈癌LNM的ROC曲线下面积为0.926。 结论 影像学检查与血清学指标和临床病理特征联合可以提高对宫颈癌淋巴结转移的预测价值。 -
关键词:
- 宫颈癌 /
- 淋巴结转移 /
- 磁共振成像 /
- 鳞状细胞癌抗原 /
- 中性粒细胞与淋巴细胞比值
Abstract:Objective This study aims to investigate the predictive value of MRI combined with preoperative serological markers: squamous cell carcinoma antigen (SCC-Ag), neutrophil to lymphocyte ratio (NLR) and biopsy pathology in lymph node metastasis of early cervical cancer. Methods A total of 307 patients who underwent primary surgery in the First Affiliated Hospital of Bengbu Medical College from January 2019 to February 2022 were selected and divided into lymph node metastasis group (81 cases) and no lymph node metastasis group (226 cases) according to the presence or absence of lymph node metastasis after surgery. The MRI lymph node short diameter, tumour size, interstitial infiltration depth, parauterine and vaginal involvement, preoperative serological indices and pathological features of the 2 groups were compared. The predictive value of lymph node metastasis and the significance of combined diagnosis were analysed. Results Logistic regression analysis showed that large short diameter of MRI lymph nodes, large tumor diameter, depth of interstitial infiltration greater than 1/2 muscular layer, parametrial involvement, increased expression of SCC-Ag and positive vascular were independent risk factors for lymph node metastasis of cervical cancer (P < 0.05). The areas under the ROC curve of MRI lymph node diameter, SCC-Ag and NLR for the diagnosis of cervical cancer LNM were 0.806, 0.711 and 0.630, respectively. The optimal cut-off values were 8.50 mm, 2.55 ng/mL and 1.90, respectively. The sensitivity values were 0.654, 0.593 and 0.593, respectively, and the specificity values were 0.881, 0.757 and 0.642, respectively. The area under the ROC curve of MRI lymph node short diameter combined with SCC-Ag diagnosis was 0.846. The area under ROC curve for the combined diagnosis of MRI lymph node short diameter, SCC-Ag and NLR was 0.863. The area under ROC curve of multiple indicators (SCC-Ag, MRI lymph node short diameter, tumour size, interstitial infiltration depth, parauterine involvement, and vascular positive) for combined diagnosis of cervical cancer LNM was 0.926. Conclusion Imaging examination (MRI) combined with serological indicators and clinicopathological features can improve the predictive value of cervical cancer lymph node metastasis. -
表 1 影响淋巴结转移的单因素分析
Table 1. Univariate analysis of influence on factors affecting lymph node metastasis
项目 转移组(81例) 未转移组(226例) 统计量 P值 年龄(x±s,岁) 49.98±7.84 52.19±9.82 1.827a 0.069 分娩次数[M(P25, P75),次] 2(2, 3) 2(2, 3) -1.153b 0.249 病程[M(P25, P75),月] 3(1, 6) 3(1, 6) -0.335b 0.737 NLR[M(P25, P75)] 1.96(1.47, 2.72) 1.67(1.31, 2.10) -3.479b <0.001 MRI肿瘤直径[M(P25, P75), cm] 4.36(3.50, 5.15) 3.00(2.00, 3.60) -7.510b <0.001 MRI淋巴结短径[M(P25, P75), mm] 9.80(7.35, 11.35) 6.50(5.80, 7.30) -8.182b <0.001 术前SCC-Ag水平[M(P25, P75), ng/mL] 3.20(1.98, 5.45) 1.80(1.10, 2.50) -5.638b <0.001 肿瘤类型[例(%)] 0.069c 0.793 内生型 60(74.1) 164(72.6) 外生型 21(25.9) 62(27.4) MRI宫旁浸润[例(%)] 66.061c <0.001 是 35(43.2) 12(5.3) 否 46(56.8) 214(94.7) MRI阴道受累[例(%)] 24.380c <0.001 是 52(64.2) 74(32.7) 否 29(35.8) 152(67.3) 脉管浸润[例(%)] 67.721c <0.001 是 38(46.9) 15(6.6) 否 43(53.1) 211(93.4) MRI间质浸润深度[例(%)] 33.760c <0.001 < 1/2肌层 10(12.3) 111(49.1) ≥1/2肌层 71(87.7) 115(50.9) 临床分期[例(%)] 24.970c <0.001 ⅠA 1(1.2) 17(7.5) ⅠB 33(40.7) 146(64.6) ⅡA 47(58.0) 63(27.9) 肿瘤细胞分化程度[例(%)] 5.545c 0.062 Ⅰ 1(1.2) 18(8.0) Ⅱ 48(59.3) 137(60.6) Ⅲ 32(39.5) 71(31.4) 注:a为t值,b为Z值,c为χ2值。 表 2 影响淋巴结转移的多因素分析
Table 2. Analysis of multiple factors affecting lymph node metastasis
变量 B SE Wald χ2 P值 OR(95% CI) NLR 0.369 0.230 2.586 0.108 1.446(0.922~2.268) MRI肿瘤直径 0.412 0.176 5.497 0.019 1.510(1.070~2.131) 术前SCC-Ag水平 0.117 0.059 3.892 0.049 1.124(1.001~1.263) MRI宫旁浸润 1.067 0.529 4.076 0.044 2.908(1.032~8.195) MRI阴道受累 0.000 0.441 0.000 0.999 1.000(0.421~2.375) MRI间质浸润深度 1.102 0.514 4.602 0.032 3.010(1.100~8.236) 临床分期 0.001 0.406 0.000 0.998 1.001(0.452~2.219) MRI淋巴结短径 0.486 0.088 30.340 <0.001 1.626(1.367~1.932) 脉管浸润 1.988 0.465 18.301 <0.001 7.298(2.936~18.142) 注:变量赋值如下, NLR、MRI肿瘤直径、SCC-Ag、MRI淋巴结短径以实际值进行赋值; MRI提示可疑宫旁浸润=1,MRI未提示可疑宫旁浸润=0;MRI提示阴道受累=1,MRI未提示阴道受累=0;MRI间质浸润深度 < 1/2肌层=0, MRI间质浸润深度>1/2肌层=1;临床分期ⅠA=0,ⅠB=1,ⅡA=2;有脉管浸润=1,无脉管浸润=0。 表 3 各指标的敏感度、特异度、阳性预测值、阴性预测值
Table 3. Sensitivity, specificity, positive predictive value and negative predictive value of each index
指标 灵敏度 特异度 阳性预测值(%) 阴性预测值(%) 95% CI MRI淋巴结短径 0.654 0.881 66.3 87.7 0.744~0.868 术前SCC-Ag水平 0.593 0.757 46.6 83.8 0.644~0.778 NLR 0.593 0.642 37.2 81.5 0.556~0.705 MRI淋巴结短径联合SCC-Ag 0.765 0.823 60.8 90.7 0.794~0.898 MRI淋巴结短径、SCC-Ag联合NLR 0.778 0.850 64.3 91.4 0.814~0.912 多指标联合 0.877 0.872 71.0 95.2 0.893~0.960 -
[1] 张军. 宫颈癌治疗的现状及问题: 从临床指南到真实世界研究[J]. 中国全科医学, 2022, 25(3): 259-263. doi: 10.12114/j.issn.1007-9572.2021.02.105ZHANG J. Current status and challenges of cervical cancer treatment: from clinical guidelines to real-world study[J]. Chinese General Practice, 2022, 25(3): 259-263. doi: 10.12114/j.issn.1007-9572.2021.02.105 [2] 陈一蕊, 勾朝阳, 李新阳. 血清SCC-Ag、sE-cadherin、β-HCG在宫颈癌诊断中的应用价值[J]. 实用癌症杂志, 2022, 37(3): 376-379. doi: 10.3969/j.issn.1001-5930.2022.03.007CHEN Y R, GOU C Y, LI X Y. Value of Serum SCC-Ag, sE-cadherin and β-HCG in the diagnosis of cervical cancer[J]. The Practical Journal of Cancer, 2022, 37(3): 376-379. doi: 10.3969/j.issn.1001-5930.2022.03.007 [3] 胡玉峰, 程晓东. NLR、FAR、SCC-Ag对宫颈鳞状细胞癌患者术前淋巴结转移的预测价值[J]. 中国妇产科临床杂志, 2022, 23(3): 278-280. https://www.cnki.com.cn/Article/CJFDTOTAL-FKLC202203018.htmHU Y F, CHENG X D. Predictive value of NLR, FAR and SCC-Ag in preoperative lymph node metastasis of patients with cervical squamous cell carcinoma[J]. Chinese Journal of Clinical Obstetrics and Gynecology, 2022, 23(3): 278-280. https://www.cnki.com.cn/Article/CJFDTOTAL-FKLC202203018.htm [4] MASRI A, STEINMETZ L, ROBINSON W R. Women with cervical carcinoma in pre-and post-katrina new orleans: a comparative analysis[J]. Gynecol Oncol, 2020, 156(3): 31-32. [5] 周琦, 吴小华, 刘继红, 等. 宫颈癌诊断与治疗指南(第四版)[J]. 中国实用妇科与产科杂志, 2018, 34(6): 613-622. doi: 10.19538/j.fk2018060111ZHOU Q, WU X H, LIU J H, et al. Guidelines to the diagnosis and treatment of cervical cancer (4th edition)[J]. Chinese Journal of Practical Gynecology and Obstetrics, 2018, 34(6): 613-622. doi: 10.19538/j.fk2018060111 [6] COHEN P A, JHINGRAN A, OAKNIN A, et al. Cervical cancer[J]. Lancet, 2019, 393(10167): 169-182. doi: 10.1016/S0140-6736(18)32470-X [7] KAN Y Y, DONG D, ZHANG Y C, et al. Radiomic signature as a predictive factor for lymph node metastasis in early-stage cervical cancer[J]. J Magn Reson Imaging, 2019, 49(1): 304-310. doi: 10.1002/jmri.26209 [8] 周晖, 刘昀昀, 罗铭, 等. 《2021 NCCN子宫颈癌临床实践指南(第1版)》解读[J]. 中国实用妇科与产科杂志, 2020, 36(11): 1098-1104. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGSF202011015.htmZHOU H, LIU Y Y, LUO M, et al. Interpretation of the NCCN clinical practice guidelines for cervical cancer(2021. v1)[J]. Chinese Journal of Practical Gynecology and Obstetrics, 2020, 36(11): 1098-1104. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGSF202011015.htm [9] 洪士彬, 程杰军, 狄文. MRI在宫颈癌分期评估中的临床应用及研究进展[J]. 国际妇产科学杂志, 2021, 48(6): 634-638. https://www.cnki.com.cn/Article/CJFDTOTAL-GWVC202106008.htmHONG S B, CHENG J J, DI W. Advances and applications of MRI in Staging assessment of cervical cancer[J]. Journal of International Obstetrics and Gynecology, 2021, 48(6): 634-638. https://www.cnki.com.cn/Article/CJFDTOTAL-GWVC202106008.htm [10] TOMASSI M J, ABBAS M A, KLARISTENFELD D D. Expectant management surveillance for patients at risk for invasive squamous cell carcinoma of the anus: a large US health care system experience[J]. Int J Colorectal Dis, 2019, 34(1): 47-54. doi: 10.1007/s00384-018-3167-7 [11] 马梅, 晋茂生, 叶国柳. HPV分型、SCC-Ag与NLR联合对早期宫颈癌淋巴结转移的预测作用[J]. 中华全科医学, 2022, 20(4): 578-582. doi: 10.16766/j.cnki.issn.1674-4152.002404MA M, JIN M S, YE G L. Predictive effect of HPV typing, SCC-Ag and NLR on lymph node metastasis of early cervical cancer[J]. Chinese Journal of General Practice, 2022, 20(4): 578-582. doi: 10.16766/j.cnki.issn.1674-4152.002404 [12] LIU Z H, SHI H T. Prognostic role of squamous cell carcinoma antigen in cervical cancer: a meta-analysis[J]. Dis Markers, 2019, 2019: 6710352. DOI: 10.1155/2019/6710352. [13] 李丹, 徐小仙, 闫鼎鼎, 等. 早期宫颈鳞状细胞癌患者检测血清鳞状细胞癌抗原的临床意义[J]. 中华肿瘤杂志, 2019, 41(5): 357-362. https://www.cnki.com.cn/Article/CJFDTOTAL-ZFYB202123018.htmLI D, XU X X, YAN D D, et al. Clinical significance of serum squamous cell carcinoma antigen in patients with early cervical squamous cell carcinoma[J]. Chinese Journal of Oncology, 2019, 41(5): 357-362. https://www.cnki.com.cn/Article/CJFDTOTAL-ZFYB202123018.htm [14] 张冬雅, 郭红军. 18F-FDG PET-CT联合血清SCC-Ag检测对宫颈癌盆腔淋巴结转移的诊断价值[J]. 中国CT和MRI杂志, 2019, 17(3): 105-108, 153. https://www.cnki.com.cn/Article/CJFDTOTAL-CTMR201903032.htmZHANG D Y, GUO H J. Value of 18F-FDG PET-CT combined with serum SCC-Ag in diagnosing pelvic lymph node metastasis of cervical cancer[J]. Chinese Journal of CT and MRI, 2019, 17(3): 105-108, 153. https://www.cnki.com.cn/Article/CJFDTOTAL-CTMR201903032.htm [15] 秦琳, 吴玉梅, 王明, 等. 增强CT淋巴结短径及SCC-Ag在术前预测宫颈鳞癌淋巴结转移中的应用[J]. 中国医药导报, 2022, 19(5): 124-128. https://www.cnki.com.cn/Article/CJFDTOTAL-YYCY202205028.htmQIN L, WU Y M, WANG M, et al. Application of the shortest diameter of lymph nodes in enhanced CT and SCC-Ag predicting pre-operation lymph node metastasis in cervical squamous cell carcinoma[J]. China Medical Herald, 2022, 19(5): 124-128. https://www.cnki.com.cn/Article/CJFDTOTAL-YYCY202205028.htm [16] 张文静, 田红梅, 王冲, 等. NLR、PLR对结肠癌根治术后手术部位感染的预测价值[J]. 分子诊断与治疗杂志, 2022, 14(2): 245-248. https://www.cnki.com.cn/Article/CJFDTOTAL-YXYQ202202016.htmZHANG W J, TIAN H M, WANG C, et al. Predictive value of NLR and PLR for surgical site infection after radical resection of colon cancer[J]. Journal of Molecular Diagnostics and Therapy, 2022, 14(2): 245-248. https://www.cnki.com.cn/Article/CJFDTOTAL-YXYQ202202016.htm [17] ZHU M L, FENG M, HE F, et al. Pretreatment neutrophil-lymphocyte and platelet-lymphocyte ratio predict clinical outcome and prognosis for cervical Cancer[J]. Clin Chim Acta, 2018, 483: 296-302. [18] 梅冰洁, 张国楠. 中性粒细胞、血小板与淋巴细胞比值对中晚期宫颈癌患者预后的评估价值[J]. 现代妇产科进展, 2019, 28(12): 892-895. https://www.cnki.com.cn/Article/CJFDTOTAL-XDFC201912003.htmMEI B J, ZHANG G N. Prognostic value of neutrophil, platelet to lymphocyte ratio in patients with advanced cervical cancer[J]. Progress in Obstetrics and Gynecology, 2019, 28(12): 892-895. https://www.cnki.com.cn/Article/CJFDTOTAL-XDFC201912003.htm [19] 赵雅文, 董頔, 薛茜文, 等. 术前外周血中NLR、PLR、LMR与早期宫颈癌患者预后的相关性研究[J]. 新疆医科大学学报, 2020, 43(8): 997-1003. https://www.cnki.com.cn/Article/CJFDTOTAL-XJYY202008004.htmZHAO Y W, DONG D, XUE Q W, et al. Correlation between NLR, PLR and LMR in preoperative peripheral blood and prognosis of patients with early cervical cancer[J]. Journal of Xinjiang Medical University, 2020, 43(8): 997-1003. https://www.cnki.com.cn/Article/CJFDTOTAL-XJYY202008004.htm [20] 王金凤, 李琛, 黄康榕, 等. 术前中性粒细胞和淋巴细胞比值、单核细胞和淋巴细胞比值与宫颈癌患者临床病理特征的相关性[J]. 兰州大学学报(医学版), 2019, 45(5): 25-29. https://www.cnki.com.cn/Article/CJFDTOTAL-LZYX201905008.htmWANG J F, LI C, HUANG K R, et al. Correlation between preoperative neutrophil-to-lymphocyte ratio, monocyte-to-lymphocyte ratio and clinical pathologic features in patients with cervical cancer[J]. 兰州大学学报(医学版), 2019, 45(5): 25-29. https://www.cnki.com.cn/Article/CJFDTOTAL-LZYX201905008.htm [21] 乌云, 苏俊玲, 杜洁, 等. 宫颈癌临床病理特征与宫旁侵犯及盆腔淋巴结转移的关系研究[J]. 局解手术学杂志, 2019, 28(12): 969-972. https://www.cnki.com.cn/Article/CJFDTOTAL-JJXZ201912009.htmWU Y, SU J L, DU J, et al. Correlation study of clinicopathologic features with parametrial invasion and pelvic lymph node metastasis in cervical cancer patients[J]. Journal of Regional Anatomy and Operative Surgery, 2019, 28(12): 969-972. https://www.cnki.com.cn/Article/CJFDTOTAL-JJXZ201912009.htm [22] 蔡斌, 吴昊, 丰有吉, 等. 100例宫颈癌临床病理特征与宫旁侵犯和盆腔淋巴结转移的关系分析[J]. 实用妇产科杂志, 2015, 31(5): 366-368. https://www.cnki.com.cn/Article/CJFDTOTAL-SFCZ201505019.htmCAI B, WU H, FENG Y J, et al. Correlation between the clinical pathology characteristic and parametrial involvement or pelvic lymph node metastasis in 100 cases of cervical cancer[J]. Journal of Practical Obstetrics and Gynecology, 2015, 31(5): 366-368. https://www.cnki.com.cn/Article/CJFDTOTAL-SFCZ201505019.htm [23] 周晖, 王东雁, 罗铭, 等. 《FIGO 2018妇癌报告》: 子宫颈癌指南解读[J]. 中国实用妇科与产科杂志, 2019, 35(1): 95-103. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGSF202205014.htmZHOU H, WANG D Y, LUO M, et al. FIGO 2018 Women's Cancer Report: Interpretation of cervical cancer Guidelines[J]. Chinese Journal of Practical Gynecology and Obstetrics, 2019, 35(1): 95-103. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGSF202205014.htm -





 下载:
下载: