Relationship between Arg389Gly gene polymorphism and improved ventricular remodelling and clinical prognosis in patients with chronic heart failure
-
摘要:
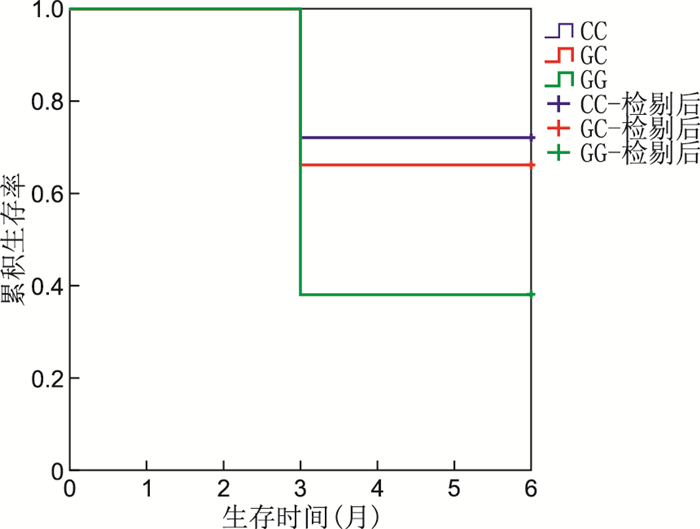
目的 探讨β1肾上腺素受体Arg389Gly基因多态性与慢性心力衰竭患者心功能变化情况及临床预后的关系。 方法 选取2020年4月—2021年5月蚌埠医学院第一附属医院的慢性心力衰竭患者120例,根据Arg389Gly基因型将患者分成CC组(43例)、GC组(56例)、GG组(21例)3组。收集患者入院时的临床资料,出院后通过门诊或电话对其进行6个月的随访,分析3组患者药物治疗前后心功能变化情况及临床预后。 结果 Arg389Gly基因型频率分别为35.8%(CC)、46.7%(GC)、17.5%(GG);随访6个月后,3组患者在氨基末端脑钠肽前体(NT-proBNP)降幅、左心室射血分数(LVEF)升幅及左心室舒张末期内径(LVDD)、左心室收缩末期内径(LVDS)降幅上的差异均有统计学意义(均P<0.05),且CC组的改善情况显著优于GG组(P<0.017);3组患者的可溶性生长刺激表达基因2蛋白(sST2)降幅在随访至6个月时其差异有统计学意义(P=0.006),且CC组优于GG组(P=0.014)。在随访过程中出现了心源性死亡、因心力衰竭再入院、恶性心律失常事件的患者共44例,log-rank检验提示3组患者终点事件发生率的差异有统计学意义(P=0.026),Kaplan-Meier曲线提示CC组终点事件的发生率低于GG组。 结论 Arg389Gly基因多态性与慢性心力衰竭患者的心功能变化及临床预后有关。 -
关键词:
- 心力衰竭 /
- Arg389Gly基因 /
- 基因多态性 /
- 心室重塑 /
- 预后
Abstract:Objective To investigate the relationship between β1 adrenergic receptor Arg389Gly gene polymorphism and cardiac function changes and clinical prognosis in patients with chronic heart failure. Methods A total of 120 patients with chronic heart failure who were admitted in the First Affiliated Hospital of Bengbu Medical College from April 2020 to May 2021 were selected. Based on the Arg389Gly genotype, patients were divided into CC (43 cases), GC (56 cases) and GG (21 cases) groups. Clinical data were collected at admission, and patients were followed up for 6 months by outpatient or telephone after discharge and the changes of cardiac function and clinical prognosis of patients in 3 groups before and after drug treatment were analyzed. Results The frequency of the Arg389Gly genotype was in the following order: CC (35.8%), GC (46.7%) and GG (17.5%). After 6 months of follow-up, there were statistically significant differences in N-terminal pro-brain natriuretic peptide (NT-proBNP) decrease, left ventricular ejection fraction (LVEF) increase, left ventricular end diastolic dimension (LVDD) and left ventricular end-systolic diameter (LVDS) decrease among the three groups (all P < 0.05), and the improvement of CC group was significantly better than that of GG group (P < 0.017). The decrease of soluble growth stimulation expression gene 2 protein (sST2) in the three groups was statistically significant at 6 months follow-up (P=0.006), and the CC group was better than the GG group (P=0.014). During follow-up, a total of 44 patients had cardiac death, readmission caused by heart failure and malignant arrhythmia events. Log-rank test indicated that the incidence of endpoint events in the three groups was statistically significant (P=0.026). Kaplan-Meier curve indicated that the incidence of endpoint events in the CC group was lower than that in the GG group. Conclusion Arg389Gly gene polymorphism is associated with cardiac function changes and clinical prognosis in patients with chronic heart failure. -
Key words:
- Heart failure /
- Arg389Gly gene /
- Gene polymorphism /
- Ventricular remodelling /
- Prognosis
-
表 1 3组CHF患者临床一般资料比较
Table 1. Comparison of general clinical data in three groups of patients with CHF
组别 例数 年龄
(x±s,岁)性别
(男/女,例)缺血性心肌病(例) 高血压性心肌病(例) 扩张型心肌病(例) NYHA分级(例) 心脏彩超 静息心率
[M(P25, P75),次/min]Ⅱ级 Ⅲ级 Ⅳ级 LVEF(x±s,%) LVDD(x±s,mm) LVDS(x±s,mm) CC组 43 64.28±11.54 24/19 22 18 3 11 22 10 38.05±8.41 62.44±5.31 51.76±7.90 72.00(65.00, 82.00) GC组 56 66.20±15.29 33/23 37 13 6 16 27 13 38.32±8.89 61.95±6.54 52.27±7.83 70.00(62.00, 83.50) GG组 21 64.14±9.23 7/14 8 9 4 6 9 6 37.48±9.60 61.29±2.65 53.14±6.51 78.00(66.00, 84.50) 统计量 0.334a 0.690b 5.440b 4.844b 2.217b 0.496b 0.070a 0.306a 0.229a 0.751c P值 0.716 0.708 0.099 0.089 0.330 0.974 0.932 0.737 0.796 0.687 组别 例数 收缩压
(x±s,mm Hg)舒张压
[M(P25, P75),mm Hg]肌酐
[M(P25, P75),mm Hg]空腹血糖
[M(P25, P75),mmol/L]总胆固醇
[M(P25, P75),mmol/L]甘油三酯
[M(P25, P75),mmol/L]NT-proBNP
[M(P25, P75),pg/mL]sST2
[M(P25, P75),ng/mL]CC组 43 138.88±22.26 76.00(68.00, 87.00) 69.00(57.00, 90.00) 5.49(5.01, 6.45) 3.58(3.10, 4.83) 1.40(0.99, 2.12) 3 990.00(2 210.00,5 822.00) 122.53(77.54,167.76) GC组 56 133.30±22.39 78.50(70.00, 89.50) 70.00(63.00, 90.00) 6.28(5.04, 7.32) 3.50(3.19, 3.98) 1.13(0.89, 1.39) 4 665.00(2 111.75,7 885.00) 128.45(87.14,163.37) GG组 21 127.52±22.42 76.00(65.00, 84.50) 71.00(64.50, 78.00) 5.79(4.91, 7.66) 3.87(3.30, 4.87) 1.27(0.97, 1.79) 5 830.00(3 065.00,8 852.50) 124.67(87.06,162.57) 统计量 1.926a 2.663c 0.206c 2.736c 3.417c 5.929c 1.759c 0.090c P值 0.150 0.264 0.902 0.255 0.181 0.052 0.415 0.956 注:a为F值,b为χ2值,c为H值。1 mm Hg=0.133 kPa。LVEF为左心室射血分数(left ventricular ejection fraction);LVDD为左心室舒张末期内径(left ventricular end diastolic dimension);LVDS为左心室收缩末期内径(left ventricular end-systolic diameter)。 表 2 3组CHF患者随访6个月患者使用美托洛尔缓释片滴定剂量的比较(x±s,mg)
Table 2. Comparison of titrated doses of metoprolol sustained-release tablets in 3 groups of CHF patients followed up for 6 months (x±s)
组别 例数 出院时 3个月 6个月 F值 P值 CC组 43 28.72±13.28 48.09±19.92a 61.07±15.88ab 29.929 <0.001 GC组 56 29.21±17.80 40.39±19.85a 53.26±22.43ab 20.047 <0.001 GG组 21 27.14±12.54 37.94±14.44 50.34±18.37ab 12.079 <0.001 F值 0.136 2.788 2.826 P值 0.873 0.066 0.063 注:与同组出院时比较, aP < 0.05;与同组3个月比较, bP < 0.05。 表 3 3组CHF患者随访6个月使用沙库巴曲缬沙坦滴定剂量的比较(x±s,mg)
Table 3. Comparison of titrated doses of Sakobattriovalsartan in 3 groups of CHF patients followed up for 6 months (x±s, mg)
组别 例数 出院时 3个月 6个月 F值 P值 CC组 43 101.74±76.06 150.00±56.69 168.60±38.61 4.870 0.009 GC组 56 93.75±46.28 143.30±60.21a 157.59±57.34a 35.554 <0.001 GG组 21 92.86±38.84 140.68±33.05 150.00±40.31a 6.553 0.003 F值 0.282 0.273 1.273 P值 0.755 0.762 0.284 注: 与同组出院时比较, aP < 0.05。 表 4 3组CHF患者随访6个月后心脏彩超指标及NT-proBNP变化比较[M(P25, P75)]
Table 4. Comparison of cardiac color ultrasound index and NT-proBNP in 3 groups of patients with CHF after 6 months of follow-up [M(P25, P75)]
组别 例数 LVEF升幅(%) LVDD降幅(mm) LVDS降幅(mm) 3个月 6个月 3个月 6个月 3个月 6个月 CC组 43 4.00(2.00, 6.00) 7.00(5.00, 9.00) 4.00(1.00, 7.50) 5.00(4.00, 7.00) 4.00(1.50, 8.00) 5.00(3.00, 8.00) GC组 56 2.00(-3.00, 6.00) 4.00(-2.00, 8.00)a 2.00(-3.00, 7.50) 5.00(2.00, 6.00) 3.00(-1.50, 6.00) 3.00(1.00, 4.50)a GG组 21 -1.00(-4.00, 5.00)a 5.00(-3.00, 6.50)a 0.00(-2.00, 3.00)a 2.00(-4.50, 7.00)a 0.00(-3.00, 4.00)a 3.00(1.50, 4.50)a H值 9.871 15.540 9.072 7.919 7.811 17.961 P值 0.007 <0.001 0.011 0.019 0.020 <0.001 组别 例数 NT-proBNP降幅(pg/mL) sST2降幅(ng/mL) 3个月 6个月 3个月 6个月 CC组 43 1 015.00(338.00,1 554.00) 1 505.00(406.00,2 940.00) 32.92(-23.32,79.72) 40.29(12.00, 99.59) GC组 56 276.00(-504.50,1 310.50) 191.40 (-256.15,1 210.00)a 15.05(-35.32,54.72) 11.24(-16.77,62.07) GG组 21 -295.00(-2 083.00,1 380.00)a -85.90(-415.00,779.00)a 25.00(-35.88,51.21) 20.00(-23.12,34.02)a H值 10.915 13.398 1.341 10.250 P值 0.004 0.001 0.511 0.006 注:与CC组比较,aP<0.017。 -
[1] YANCY C W, JESSUP M, BOZKURT B, et al. 2017 ACC/AHA/HFSA focused update of the 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America[J]. Circulation, 2017, 136(6): 137-161. [2] DOIMO S, PAVAN D. Novelties in therapy of chronic heart failure[J]. Heart Fail Clin, 2021, 17(2): 255-262. doi: 10.1016/j.hfc.2021.01.006 [3] OLIVER E, MAYOR F J R, D'OCON P. Beta-blockers: historical perspective and mechanisms of action[J]. Rev Esp Cardiol, 2019, 72(10): 853-862. doi: 10.1016/j.recesp.2019.02.023 [4] 中华医学会心血管病学分会心力衰竭学组, 中国医师协会心力衰竭专业委员会, 中华心血管病杂志编辑委员会. 中国心力衰竭诊断和治疗指南2018[J]. 中华心血管病杂志, 2018, 46(10): 760-789. doi: 10.3760/cma.j.issn.0253-3758.2018.10.004Heart failure Group, Chinese Society of Cardiology, Chinese Medical Doctor Association Heart Failure Professional Committee, Editorial Board of the Chinese Journal of Cardiovascular Diseases. Chinese Guidelines for the Diagnosis and Treatment of Heart Failure 2018[J]. 中华心血管病杂志, 2018, 46(10): 760-789. doi: 10.3760/cma.j.issn.0253-3758.2018.10.004 [5] MCCRINK K A, BRILL A, JAFFERJEE M, et al. β1-adrenoceptor Arg389Gly polymorphism confers differential β-arrestin-binding tropism in cardiac myocytes[J]. Pharmacogenomics, 2016, 17(15): 1611-1620. doi: 10.2217/pgs-2016-0094 [6] ROSSIGNOL P, HERNANDEZ A F, SOLOMON S D, et al. Heart failure drug treatment[J]. The Lancet, 2019, 393(10175): 1034-1044. doi: 10.1016/S0140-6736(18)31808-7 [7] 潘春奇, 菅颖, 倪斌, 等. 沙库巴曲缬沙坦对射血分数降低的缺血性心肌病患者心肌损伤和炎症因子的影响[J]. 中华全科医学, 2020, 18(11): 1848-1850. doi: 10.16766/j.cnki.issn.1674-4152.001635PAN C Q, JIAN Y, NI B, et al. The effect of sacubitril/valsartan on myocardial injury and inflammatory factors in ischemic cardiomyopathy with reduced ejection fraction[J]. Chinese Journal of General Practice, 2020, 18(11): 1848-1850. doi: 10.16766/j.cnki.issn.1674-4152.001635 [8] GAO X, WANG H, CHEN H. Impact of CYP2D6 and ADRB1 polymorphisms on heart rate of post-PCI patients treated with metoprolol[J]. Pharmacogenomics, 2017, 11. DOI: 10.2217/pgs-2017-0203. [9] THOMAS C D, JOHNSON J A. Pharmacogenetic factors affecting β-blocker metabolism and response[J]. Expert Opin Drug Metab Toxicol, 2020, 16(10): 953-964. doi: 10.1080/17425255.2020.1803279 [10] BENCIVENGA L, LICCARDO D, NAPOLITANO C, et al. β-Adrenergic receptor signaling and heart failure: from bench to bedside[J]. Heart Fail Clin, 2019, 15(3): 409-419. doi: 10.1016/j.hfc.2019.02.009 [11] PETROW V S, SMIRNOVA E A. The role of ADRB1 genes polymorphism in examined patients with chronic rheumatic heart disease[J]. Probl Sotsialnoi Gig Zdravookhranenniiai Istor Med, 2019, 27(6): 962-966. [12] CORLETTO A, FROHLICH H, TAGER T, et al. Beta blockers and chronic heart failure patients: prognostic impact of a dose targeted beta blocker therapy vs. heart rate targeted strategy[J]. Clin Res Cardiol, 2018, 107(11): 1040-1049. doi: 10.1007/s00392-018-1277-4 [13] PARIKH K S, FIUZAT M, DAVIS G, et al. Dose response of β-bockers in adrenergic receptor polymorphism genotypes[J]. Circ Genom Precis Med, 2018, 11(8): e002210. DOI: 10.1161/CIRCGEN.117.002210. [14] TAYLOR M R, SUN A Y, DAVIS G, et al. Race, common genetic variation, and therapeutic response disparities in heart failure[J]. JACC Heart Fail, 2014, 2(6): 561-572. doi: 10.1016/j.jchf.2014.06.010 [15] ABOUEZZEDDINE O F, MCKIE P M, DUNLAY S M, et al. Suppression of tumorigenicity 2 in heart failure with preserved ejection fraction[J]. J Am Heart Assoc, 2017, 6(9): e002231. DOI: 10.1161/JAHA.117.002231. [16] AJAM T, AJAM S, DEVARAJ S, et al. Effect on mortality of higher versus lower β-blocker dose in patients with heart failure[J]. Am Cardiol, 2018, 122(6): 994-998. doi: 10.1016/j.amjcard.2018.05.038 -





 下载:
下载: