Efficacy of serum sTREM-1 combined with SIRS score in the diagnosis of sepsis in burn patients
-
摘要:
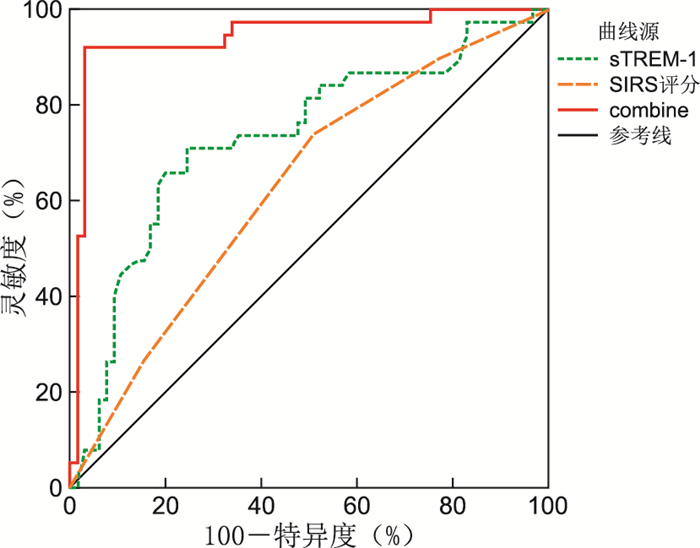
目的 探讨烧伤患者血清可溶性髓样细胞触发受体1(sTREM-1)及全身炎症反应综合征(SIRS)评分的变化,以及两指标对烧伤患者并发脓毒症的诊断价值。 方法 选择2019年3月—2020年10月山东省立第三医院收治的193例烧伤患者,其中局部感染65例(局部感染组),合并脓毒症38例(脓毒症组),单纯烧伤90例(单纯烧伤组)。检测血清sTREM-1水平,进行SIRS评分,采用受试者工作特征曲线(ROC)分析sTREM-1联合SIRS评分诊断烧伤并发脓毒症的价值。 结果 脓毒症组血清sTREM-1水平[(169.83±31.54)ng/mL、(124.05±24.09)ng/mL、(72.18±11.58)ng/mL],SIRS评分[3.5(2.0, 4.0)分、1.5(1.0, 2.0)分、0.5(0, 1.0)分]高于局部感染组和单纯烧伤组(P<0.05),局部感染组血清sTREM-1水平、SIRS评分高于单纯烧伤组(P<0.05)。Logistic回归分析结果显示,高水平sTREM-1(OR=2.003,95% CI:1.945~2.135)是烧伤患者合并脓毒症的危险因素(P<0.05)。ROC分析结果显示sTREM-1、SIRS评分、联合sTREM-1和SIRS评分诊断烧伤患者合并脓毒症的曲线下面积(AUC)分别为0.731、0.629、0.943,联合诊断高于单独sTREM-1、SIRS评分(P<0.05)。 结论 sTREM-1、SIRS评分在烧伤患者并发脓毒症诊断方面具有一定的价值,联合两项指标可提高诊断效能。 -
关键词:
- 烧伤 /
- 脓毒症 /
- 可溶性髓样细胞触发受体1 /
- 全身炎症反应综合征评分
Abstract:Objective To explore the changes of serum soluble medullary cell trigger receptor 1 (sTREM-1) and systemic inflammatory response syndrome (SIRS) scores in burn patients, and the diagnostic value of the two indexes in burn patients complicated with sepsis. Methods A total of 193 burn patients admitted to Shandong Provincial Third Hospital from March 2019 to October 2020 were selected, including 65 cases of local infection (local infection group), 38 cases of sepsis (sepsis group), and 90 cases of simple burn (simple burns group). Serum sTREM-1 level was detected and SIRS score was performed. The value of sTREM-1 combined with SIRS score in diagnosing burn complicated sepsis was analyzed by receiver operating characteristic curve (ROC). Results Serum sTREM-1 level [(169.83±31.54) ng/mL, (124.05±24.09) ng/mL, (72.18±11.58) ng/mL] and SIRS score [3.5 (2.0, 4.0) vs, 1.5(1.0, 2.0), 0.5(0, 1.0)] in the sepsis group were higher than those in the local infection group and the Simple burns group (P < 0.05), and serum sTREM-1 level and SIRS score in the local infection group were higher than those in the simple burns group (P < 0.05). Logistic regression analysis showed that high sTREM-1 level (OR=2.003, 95% CI: 1.945-2.135) was a risk factor for sepsis in burn patients (P < 0.05). ROC analysis showed that the AUC of sTREM-1, SIRS score, combined sTREM-1 and SIRS score in the diagnosis of burn patients with sepsis were 0.731, 0.629 and 0.943, respectively, and the combined diagnosis was higher than that of sTREM-1 and SIRS score alone (P < 0.05). Conclusion sTREM-1 and SIRS score have certain value in the diagnosis of sepsis in burn patients, and the combination of the two indexes can improve the diagnostic efficiency. -
表 1 3组烧伤患者基线资料比较
Table 1. Comparison of baseline data of burn patients in 3 groups
组别 例数 年龄(x±s,岁) 性别[例(%)] 烧伤至就诊时间(x±s,h) 致伤原因[例(%)] 男性 女性 电损伤 热压伤 化学烧伤 火焰烧伤 单纯烧伤组 90 48.15±12.31 53(58.89) 37(41.11) 1.65±0.36 42(46.67) 19(21.11) 8(8.89) 21(23.33) 局部感染组 65 48.73±11.96 39(60.00) 26(40.00) 2.05±0.42c 29(44.62) 14(21.54) 3(4.62) 19(29.23) 脓毒症组 38 49.62±12.17 25(65.79) 13(34.21) 3.11±0.59c 16(42.11) 9(23.68) 2(5.26) 11(28.95) 统计量 0.198a 0.549b 151.670a 1.998b P值 0.821 0.760 <0.001 0.920 组别 例数 烧伤部位[例(%)] 烧伤面积(x±s,%) 烧伤指数(x±s) 头面部 四肢 躯干 单纯烧伤组 90 12(13.33) 52(57.78) 26(28.89) 15.35±4.15 19.25±5.26 局部感染组 65 7(10.77) 31(47.69) 27(41.54) 24.65±6.46c 29.26±9.98c 脓毒症组 38 6(15.79) 18(47.37) 14(36.84) 41.24±12.11c 45.19±9.75c 统计量 3.243b 177.788a 140.018a P值 0.518 <0.001 <0.001 注:a为F值,b为χ2值;与单纯烧伤组比较,cP<0.05。 表 2 3组烧伤患者血清sTREM-1水平、SIRS评分比较
Table 2. Comparison of serum sTREM-1 level and SIRS score in three groups of burn patients
组别 例数 sTREM-1(x±s,ng/mL) SIRS评分[M(P25, P75),分] 单纯烧伤组 90 72.18±11.58 0.5(0, 1.0) 局部感染组 65 124.05±24.09a 1.5(1.0, 2.0)a 脓毒症组 38 169.83±31.54ab 3.5(2.0, 4.0)ab 统计量 306.790c 26.487d P值 <0.001 <0.001 注:与单纯烧伤组比较,aP<0.05;与局部感染组比较,bP<0.05;c为F值,d为Z值。 表 3 烧伤患者并发脓毒症的logistic回归分析
Table 3. Logistic regression analysis of burn patients complicated with sepsis
因素 β SE Wald χ2 P值 OR(95% CI) 烧伤至就诊时间 0.265 0.193 1.885 0.606 1.303(0.924~1.407) 烧伤面积 0.312 0.269 1.345 0.913 1.366(0.952~1.456) 烧伤指数 0.632 0.217 8.482 0.003 1.881(1.724~1.937) sTREM-1 0.695 0.236 8.673 0.001 2.003(1.945~2.135) 表 4 各指标诊断烧伤患者并发脓毒症的效能
Table 4. Efficacy of each index in diagnosing sepsis in burn patients
指标 AUC 95% CI 灵敏度(%) 特异度(%) 约登指数 sTREM-1 0.731 0.626~0.836 71.05 72.31 0.43 SIRS评分 0.629 0.519~0.739 73.68 50.77 0.24 联合 0.943 0.890~0.996 92.11 93.85 0.86 -
[1] RECH M A, MOSIER M J, MCCONKEY K, et al. Outcomes in burn-injured patients who develop sepsis[J]. J Burn Care Res, 2019, 40(3): 269-273. doi: 10.1093/jbcr/irz017 [2] WONG D M, RUBY R E, DEMBEK K A, et al. Evaluation of updated sepsis scoring systems and systemic inflammatory response syndrome criteria and their association with sepsis in equine neonates[J]. J Vet Intern Med, 2018, 32(3): 1185-1193. doi: 10.1111/jvim.15087 [3] 朱梦莉, 王智超, 张婧, 等. 全身炎症反应综合征评分、序贯器官衰竭评分、快速脓毒症相关器官功能障碍评分对急诊感染性疾病预后的评估价值[J]. 安徽医药, 2021, 25(2): 261-264. doi: 10.3969/j.issn.1009-6469.2021.02.012ZHU M L, WANG Z C, ZHANG J, et al. The value of SIRS, SOFA and qSOFA in evaluating the prognosis of infectious diseases in emergency department[J]. Anhui Medical and Pharmaceutical Journal, 2021, 25(2): 261-264. doi: 10.3969/j.issn.1009-6469.2021.02.012 [4] 庾胜, 张碧波, 顾晓蕾, 等. qSOFA联合SIRS评分对急诊脓毒症的早期诊断效能分析[J]. 山东医药, 2019, 59(20): 86-89. doi: 10.3969/j.issn.1002-266X.2019.20.025YU S, ZHANG B B, GU X L, et al. Early diagnosis of emergency sepsis by qSOFA combined with SIRS score[J]. Shandong Medical Journal, 2019, 59(20): 86-89. doi: 10.3969/j.issn.1002-266X.2019.20.025 [5] 汪伟, 吴蔚, 高峰, 等. 慢性阻塞性肺疾病急性加重期患者血清sTREM-1、sCD163水平变化及临床意义[J]. 中华全科医学, 2021, 19(2): 236-240. doi: 10.16766/j.cnki.issn.1674-4152.001776WANG W, WU W, GAO F, et al. Changes and clinical significance of serum STREM-1 and sCD163 levels in patients with acute exacerbation of chronic obstructive pulmonary disease[J]. Chinese Journal of General Practice, 2021, 19(2): 236-240. doi: 10.16766/j.cnki.issn.1674-4152.001776 [6] CHANG W, PENG F, MENG S S, et al. Diagnostic value of serum soluble triggering expressed receptor on myeloid cells 1 (sTREM-1) in suspected sepsis: a meta-analysis[J]. BMC Immunol, 2020, 21(1): 2. doi: 10.1186/s12865-020-0332-x [7] 中华医学会重症医学分会. 中国严重脓毒症/脓毒性休克治疗指南(2014)[J]. 中华内科杂志, 2015, 54(6): 557-581. https://www.cnki.com.cn/Article/CJFDTOTAL-HBYX201612031.htmChinese Society of Critical Care Medicine. Chinese guidelines for the treatment of severe sepsis/septic shock (2014)[J]. Chinese Journal of Internal Medicine, 2015, 54(6): 557-581. https://www.cnki.com.cn/Article/CJFDTOTAL-HBYX201612031.htm [8] BONE R C, BALK R A, CERRA F B, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in Sepsis. The ACCP/SCCM consensus conference committee. American college of chest physicians/society of critical care medicine[J]. Chest, 1992, 101(6): 1644-1655. doi: 10.1378/chest.101.6.1644 [9] EVANS T. Diagnosis and management of sepsis[J]. Clin Med (Lond), 2018, 18(2): 146-149. [10] 林颜, 阮树斌, 陈晓东, 等. 丹参川芎嗪注射液对重度烧伤患者炎性因子影响及预防脓毒症发生效果分析[J]. 河北医学, 2018, 24(3): 382-385. doi: 10.3969/j.issn.1006-6233.2018.03.008LIN Y, RUAN S B, CHEN X D, et al. Effect of salviae miltiorrhizae and ligustrazine hydrochloride injection on the inflammatory factors of severe burn patients and the prevention of sepsis[J]. Hebei Medicine, 2018, 24(3): 382-385. doi: 10.3969/j.issn.1006-6233.2018.03.008 [11] 程高翔, 方长太, 查君敬, 等. 白细胞介素-35在脓毒症病情评估及预后中的应用[J]. 安徽医药, 2017, 21(4): 672-675. doi: 10.3969/j.issn.1009-6469.2017.04.022CHENG G X, FANG Z T, CHA J J, et al. Application research of Interleukin-35 in sepsis correlated with condition evaluation and prognosis[J]. Anhui Medical and Pharmaceutical Journal, 2017, 21(4): 672-675. doi: 10.3969/j.issn.1009-6469.2017.04.022 [12] SINGER M, DEUTSCHMAN C S, SEYMOUR C W, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3)[J]. JAMA, 2016, 315(8): 801-810. doi: 10.1001/jama.2016.0287 [13] TUSGUL S, CARRON P N, YERSIN B, et al. Low sensitivity of qSOFA, SIRS criteria and sepsis definition to identify infected patients at risk of complication in the prehospital setting and at the emergency department triage[J]. Scand J Trauma Resusc Emerg Med, 2017, 25(1): 108. doi: 10.1186/s13049-017-0449-y [14] JIANG J J, YANG J, MEI J, et al. Head-to-head comparison of qSOFA and SIRS criteria in predicting the mortality of infected patients in the emergency department: a meta-analysis[J]. Scand J Trauma Resusc Emerg Med, 2018, 26(1): 56. doi: 10.1186/s13049-018-0527-9 [15] SU L X, LIU D, CHAI W Z, et al. Role of sTREM-1 in predicting mortality of infection: a systematic review and meta-analysis[J]. BMJ Open, 2016, 6(5): e010314. DOI: 10.1136/bmjopen-2015-010314. [16] 李春华, 刘微丽. 血清HbA1c、sTREM-1与CC16联合检测对COPD患者病情程度变化的判定价值研究[J]. 河北医药, 2019, 41(10): 1494-1497. https://www.cnki.com.cn/Article/CJFDTOTAL-HBYZ201910012.htmLI C H, LIU W L. The application value of combination detection of serum levels of HbA1c, sTREM-1 and CC16 in the evaluation of the severity of patients with COPD[J]. Hebei Medical Journal, 2019, 41(10): 1494-1497. https://www.cnki.com.cn/Article/CJFDTOTAL-HBYZ201910012.htm [17] 程雪莲. Pro-ADM、sTREM-1水平测定在新生儿败血症检测中的临床价值[J]. 实验与检验医学, 2020, 38(1): 82-83, 122. https://www.cnki.com.cn/Article/CJFDTOTAL-JXJL202001025.htmCHENG X L. Clinical value of Pro-ADM and sTREM-1 levels in neonatal sepsis[J]. Experimental and Laboratory Medicine, 2020, 38(1): 82-83, 122. https://www.cnki.com.cn/Article/CJFDTOTAL-JXJL202001025.htm [18] HU C P, JIANG J, LI Z, et al. Expression pattern of soluble triggering receptor expressed on myeloid cells-1 in mice with Acinetobacter baumannii colonization and infection in the lung[J]. J Thorac Dis, 2018, 10(3): 1614-1621. [19] LI C X, ZHU L M, GONG X L, et al. Soluble triggering receptor expressed on myeloid cells-1 as a useful biomarker for diagnosing ventilator-associated pneumonia after congenital cardiac surgery in children[J]. Exp Ther Med, 2019, 17(1): 147-152. [20] AKSARAY S, ALAGOZ P, INAN A, et al. Diagnostic value of sTREM-1 and procalcitonin levels in the early diagnosis of sepsis[J]. North Clin Istanb, 2017, 3(3): 175-182. [21] CHARLES P E, NOEL R, MASSIN F, et al. Significance of soluble triggering receptor expressed on myeloid cells-1 elevation in patients admitted to the intensive care unit with sepsis[J]. BMC Infect Dis, 2016, 16(1): 559. -





 下载:
下载: