Short-term clinical effect analysis of unilateral biportal endoscopic surgery for of single responsible segment lumbar spinal stenosis
-
摘要:
目的 探讨单侧双通道内镜(unilateral biportal endoscopic,UBE)下椎管减压治疗单节段腰椎管狭窄症(lumbar spinal stenosis,LSS)的短期临床疗效。 方法 回顾性分析滨州医学院附属医院2020年6月—2021年3月脊柱外科119例LSS患者的临床资料,男性57例,女性62例,年龄为(58.3±10.0)岁,病程为(19.6±9.2)个月,责任节段L3/4 9例,L4/5 85例,L5/S1 25例。所有患者均通过UBE技术单侧入路部分椎板切除实现单侧或双侧受压神经的充分减压。比较术前、术后3个月、12个月患者腰腿痛视觉模拟评分(VAS)和Oswestry功能障碍指数(ODI);比较术前、术后1个月硬膜囊面积;评价术后12个月的临床疗效(改良MacNab标准),并记录手术时间、术中出血量及并发症情况。 结果 手术均顺利完成,术中出血量为(15.3±10.0)mL,手术时间为(75.2±31.2)min,术后住院时间为(6.7±1.6)d,随访(14.5±1.4)个月。术后出现硬膜囊撕裂1例,硬膜外血肿2例。术后1个月硬膜囊面积较术前改善明显[(129.6±13.8)mm2 vs. (52.6±11.5)mm2,P<0.05]。术后3个月、12个月VAS评分及ODI指数均较术前明显改善(均P<0.05)。临床疗效:优84例,良26例,可6例,差3例,优良率为92.4%(110/119)。 结论 UBE治疗单责任节段LSS疗效确切,创伤小、操作方便、术后恢复快。 -
关键词:
- 腰椎管狭窄症 /
- 单侧双通道内镜 /
- 微创腰椎减压 /
- 单侧椎板入路双侧椎管减压
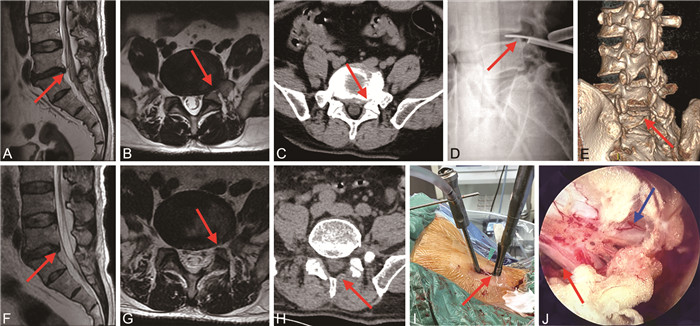
Abstract:Objective To investigate the short-term clinical effect of spinal canal decompression under Unilateral Biportal Endoscopy (UBE) in the treatment of single-segment lumbar spinal stenosis (LSS). Methods The clinical data of 119 patients with LSS in spine surgery from June 2020 to March 2021 in the Affiliated Hospital of Binzhou Medical University were analyzed retrospectively. There were 57 males and 62 females, with an average age of (58.3±10.0) years, a course of disease of (19.6±9.2) months, segmental L3/4 9 cases, L4/5 85 cases and L5/S1 25 cases. All patients underwent partial laminectomy through unilateral approach with UBE technology to achieve full decompression of unilateral or bilateral compressed nerves. Visual Analogue Scale (VAS) and Oswestry Disability Index (ODI) were compared before operation, 3 months and 1 year after operation. The area of dural sac was compared before and 1 month after operation. The clinical efficacy (modified MacNab standard) at 1 year after operation was evaluated, and the operation time, intraoperative blood loss and complications were recorded. Results All operations were successfully completed. The intraoperative blood loss was (15.3±10.0) mL, the operation time was (75.2±31.2) min, the postoperative hospital stay was (6.7±1.6) days, and the follow-up time was (14.5±1.4) months. There were 1 case of dural sac tear and 2 cases of epidural hematoma after operation. The dural sac area was significantly improved [(129.6±13.8) mm2 vs. (52.6±11.5) mm2, P < 0.05] one month after operation. The VAS score and ODI were significantly improved at 3 months and 12 months after operation (all P < 0.05). The clinical efficacy was excellent in 84 cases, good in 26 cases, fair in 6 cases, and poor in 3 cases. The excellent and good rate was 92.4% (110/119). Conclusion The UBE has definite curative effect, less trauma, convenient operation and rapid postoperative recovery in the treatment of single responsible segmental LSS. -
表 1 不同时间点LSS患者VAS评分及ODI指数比较(x±s)
Table 1. Comparison of VAS score and ODI index of LSS patients at different time points(x±s)
时间 VAS(分) ODI(%) 术前 7.5±1.2 72.1±6.9 术后3个月 2.1±1.0a 36.1±8.1a 术后12个月 1.2±0.8ab 17.2±2.9ab F值 771.767 1 603.564 P值 <0.001 <0.001 注:与术前比较,aP<0.001;与术后3个月比较,bP<0.001。 -
[1] KATZ J N, ZIMMERMAN Z E, MASS H, et al. Diagnosis and management of lumbar spinal stenosis: a review[J]. JAMA, 2022, 327(17): 1688-1699. doi: 10.1001/jama.2022.5921 [2] HATAKKA J, PERNAA K, RANTAKOKKO J, et al. Effect of lumbar laminectomy on spinal sagittal alignment: a systematic review[J]. Eur Spine J, 2021, 30(9): 2413-2426. doi: 10.1007/s00586-021-06827-y [3] ZHANG J, LIU T F, SHAN H, et al. Decompression using minimally invasive surgery for lumbar spinal stenosis associated with degenerative spondylolisthesis: a review[J]. Pain Ther, 2021, 10(2): 941-959. doi: 10.1007/s40122-021-00293-6 [4] AHN Y. A historical review of endoscopic spinal discectomy[J]. World Neurosurg, 2021, 145: 591-596. doi: 10.1016/j.wneu.2020.08.008 [5] 汪文龙, 刘正, 吴四军, 等. 单侧双通道内镜下减压治疗腰椎管狭窄症的早期疗效观察[J]. 中国脊柱脊髓杂志, 2021, 31(10): 911-918. doi: 10.3969/j.issn.1004-406X.2021.10.06WANG W L, LIU Z, WU S J, et al. Preliminary clinical outcomes of unilateral biportal endoscopy for decompressing lumbar spinal stenosis[J]. Chinese Journal of Spine and Spinal Cord, 2021, 31(10): 911-918. doi: 10.3969/j.issn.1004-406X.2021.10.06 [6] 赵龙, 张荣宜, 刘畅. 椎间孔镜手术与等离子联合胶原酶手术治疗腰椎间盘突出症的临床疗效比较[J]. 中华全科医学, 2021, 19(11): 1827-1830. doi: 10.16766/j.cnki.issn.1674-4152.002177ZHAO L, ZHANG R Y, LIU C. Comparison of the clinical effects of percutaneous transforaminal endoscopic discectomy and plasma-mediated radiofrequency ablation combined with collagenase in the treatment of lumbar disc herniation[J]. Chinese Journal of General Practice, 2021, 19(11): 1827-1830. doi: 10.16766/j.cnki.issn.1674-4152.002177 [7] HENNEMANN S, DE ABREU M R. Degenerative lumbar spinal stenosis[J]. Rev Bras Ortop (Sao Paulo), 2021, 56(1): 9-17. doi: 10.1055/s-0040-1712490 [8] OULD-SLIMANE M, CANTOGREL P, LEFÈVRE E, et al. Minimally invasive unilateral lumbar interbody fusion (UNILIF) in over-80-year-olds. Continuous series of 42 patients at 1.4 years ' follow-up[J]. Orthop Traumatol Surg Res, 2020, 106(2): 275-279. doi: 10.1016/j.otsr.2020.01.003 [9] KNIO Z O, SCHALLMO M S, HSU W, et al. Unilateral laminotomy with bilateral decompression: a case series studying one- and two-year outcomes with predictors of minimal clinical improvement[J]. World Neurosurg, 2019, 131: e290-e297. doi: 10.1016/j.wneu.2019.07.144 [10] YE J W, YANG S Z, WEI Z H, et al. Incidence and risk factors for adjacent segment disease after transforaminal lumbar interbody fusion in patients with lumbar degenerative diseases[J]. Int J Gen Med, 2021, 14: 8185-8192. doi: 10.2147/IJGM.S337298 [11] HAIMOTO S, NISHIMURA Y, HARA M, et al. Clinical and radiological outcomes of microscopic lumbar foraminal decompression: a pilot analysis of possible risk factors for restenosis[J]. Neurol Med Chir (Tokyo), 2018, 58(1): 49-58. doi: 10.2176/nmc.oa.2017-0121 [12] CHOI C M. Biportal endoscopic spine surgery (BESS): considering merits and pitfalls[J]. J Spine Surg, 2020, 6(2): 457-465. doi: 10.21037/jss.2019.09.29 [13] XU J, ZHUANG W D, ZHENG W, et al. Microscopic ventral neural decompression in oblique lateral interbody fusion[J]. World Neurosurg, 2019, 128: e315-e321. doi: 10.1016/j.wneu.2019.04.142 [14] 谷艳超, 李莹, 谢维, 等. 单边双通道脊柱内镜技术治疗腰椎椎管狭窄症临床分析[J]. 国际骨科学杂志, 2021, 42(5): 323-328. doi: 10.3969/j.issn.1673-7083.2021.05.014GU Y C, LI Y, XIE W, et al. Clinical analysis of unilateral biportal endoscopy for treatment of lumbar spinal stenosis[J]. International Journal of Orthopaedics, 2021, 42(5): 323-328. doi: 10.3969/j.issn.1673-7083.2021.05.014 [15] KIM J E, CHOI D J, PARK E J J, et al. Biportal endoscopic spinal surgery for lumbar spinal stenosis[J]. Asian Spine J, 2019, 13(2): 334-342. doi: 10.31616/asj.2018.0210 [16] LI J C, LI H, HE Y W, et al. The protection of superior articular process in percutaneous transforaminal endoscopic discectomy should decreases the risk of adjacent segment diseases biomechanically[J]. J Clin Neurosci, 2020, 79: 54-59. doi: 10.1016/j.jocn.2020.07.025 [17] SPINA N T, MORENO G S, BRODKE D S, et al. Biomechanical effects of laminectomies in the human lumbar spine: a finite element study[J]. Spine J, 2021, 21(1): 150-159. doi: 10.1016/j.spinee.2020.07.016 [18] 毕经纬, 李瑞, 孙宁, 等. 单侧双通道内镜与椎间孔镜治疗腰椎管狭窄症的比较[J]. 中国微创外科杂志, 2022, 22(2): 102-107. doi: 10.3969/j.issn.1009-6604.2022.02.002BI J W, LI R, SUN N, et al. Comparison of unilateral biportal endoscopic and percutaneous transforaminal endoscopic discectomy for lumbar spinal stenosis[J]. Chinese Journal of Minimally Invasive Surgery, 2022, 22(2): 102-107. doi: 10.3969/j.issn.1009-6604.2022.02.002 [19] HEO D H, LEE D C, PARK C K. Comparative analysis of three types of minimally invasive decompressive surgery for lumbar central stenosis: biportal endoscopy, uniportal endoscopy, and microsurgery[J]. Neurosurg Focus, 2019, 46(5): E9. DOI: 10.3171/2019.2.FOCUS197. -





 下载:
下载: