Predictive value of HIST1H3D in lymph node metastasis of early cervical cancer
-
摘要:
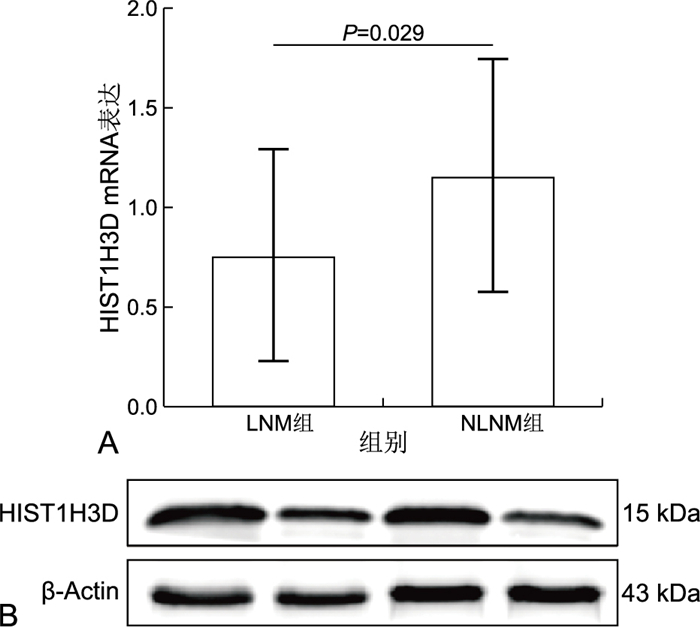
目的 分析探讨早期宫颈癌淋巴结转移的高危因素,研究HIST1H3D对早期宫颈癌淋巴结转移的预测价值。 方法 从蚌埠医学院第一附属医院选取2021年1—12月在妇产科行根治性子宫切除术的早期宫颈鳞癌患者组织40例,以及2016年1月—2020年12月的早期宫颈鳞癌患者蜡块标本124例。通过RT-qPCR、Western blotting和免疫组化分析HIST1H3D在淋巴结转移组与非转移组的表达差异;通过χ2检验及生存分析曲线分析HIST1H3D对早期宫颈癌淋巴结转移组与非转移组临床特征和生存的影响;使用二元logistic回归分析淋巴结转移的影响因素。 结果 FIGO分期(χ2=30.491,P<0.001),肿瘤大小(χ2=8.362,P<0.004),淋巴血管间隙浸润(χ2=29.350,P<0.001)和HIST1H3D表达(χ2=4.148,P<0.042)等与淋巴结转移显著相关。HIST1H3D基因过表达是早期宫颈癌淋巴结转移的高危因素,淋巴结阳性组患者生存率更差(P=0.014)。HIST1H3D的高低表达组生存率存在显著差异,HIST1H3D低表达组生存期更长(P=0.019)。ROC曲线结果表明当HIST1H3D免疫组化评分为5时,曲线下面积(AUC)为0.704,灵敏度为89.29%,特异度为64.71%,此时对淋巴结转移预测效果最佳(P<0.001)。 结论 HIST1H3D对早期宫颈癌淋巴结转移有预测价值。 -
关键词:
- 宫颈癌 /
- HIST1H3D基因 /
- 淋巴结转移 /
- 预后
Abstract:Objective To analyze the high-risk factors of lymph node metastasis in early cervical cancer, and study the predictive value of HIST1H3D in lymph node metastasis of cervical cancer. Methods A total of 40 patients with early cervical squamous cell carcinoma who underwent radical hysterectomy in Department of Obstetrics and Gynecology from January to December 2021 and 124 patients with early cervical squamous cell carcinoma from January 2016 to December 2020 were selected from the First Affiliated Hospital of Bengbu Medical College. The expression difference of HIST1H3D in lymph node metastasis group and non-metastasis group was analyzed by RT-qPCR, Western Blot and immunohistochemistry. Chi-square test and survival curve analysis were used to analyze the influence of HIST1H3D on the clinical characteristics and survival of lymph node metastasis group and non-metastasis group of early stage cervical carcinoma. The influencing factors of lymph node metastasis were analyzed by binary logistic regression. Results FIGO stage (χ2=30.491, P < 0.001), tumor size (χ2=8.362, P < 0.004), infiltration of lymphatic vascular space (P < 0.001), vaginal involvement (χ2=29.350, P < 0.001) and HIST1H3D expression (χ2=4.148, P < 0.042) were significantly related to lymph node metastasis. Overexpression of HIST1H3D gene was a high-risk factor for lymph node metastasis in early cervical cancer. The survival rate of patients with positive lymph nodes was worse (P=0.0136). There was significant difference in survival rate between the high and low expression groups of HIST1H3D, and the low expression group of HIST1H3D had a longer survival time (P=0.019). ROC curve showed that when HIST1H3D immunohistochemical score was 5, the area under the curve (AUC) was 0.704, the sensitivity was 89.29%, the specificity was 64.71%. At this time, the prediction effect of lymph node metastasis was the best (P < 0.001). Conclusion HIST1H3D has predictive value for lymph node metastasis of early stage cervical cancer. -
Key words:
- Cervical cancer /
- HIST1H3D gene /
- Lymph node metastasis /
- Prognosis
-
表 1 淋巴结转移与早期宫颈癌临床特征的关系
Table 1. Relationship between lymph node metastasis and clinical features of early cervical cancer
临床病理特征 类别 例数 淋巴结转移 阳性率(%) χ2值 P值 临床病理特征 类别 例数 淋巴结转移 阳性率(%) χ2值 P值 是 否 是 否 年龄 ≤51岁 61 30 31 49.18 0.783 0.376 阴道受累 是 67 41 26 61.19 15.128 <0.001 >51岁 63 26 37 41.27 否 57 15 42 26.32 HPV感染 是 110 49 61 44.55 0.149 0.699 淋巴血管间隙浸润 是 31 27 4 87.10 29.350 <0.001 否 14 7 7 50.00 否 93 29 64 31.18 肿瘤大小 ≤4 cm 77 27 50 35.06 8.362 0.004 术后辅助治疗 是 107 43 64 40.19 7.798 0.005 >4 cm 47 29 18 61.70 否 17 13 4 76.47 间质浸润深度 ≤1/2 28 8 20 28.57 4.019 0.045 HIST1H3D表达 高 101 50 51 49.50 4.148 0.042 >1/2 96 48 48 50.00 无或低 23 6 17 26.09 FIGO分期 ⅠA 1 0 1 0 30.491 <0.001 随访时生命状态 死亡 21 14 7 66.67 4.721 0.030 ⅠB 50 8 42 16.00 存活 103 42 61 40.78 ⅡA 73 48 25 65.75 分化等级 G1~G2 89 42 47 47.19 0.525 0.469 G3 35 14 21 40.00 表 2 早期宫颈癌淋巴结转移的二元logistic回归分析
Table 2. Binary logistic regression analysis of lymph node metastasis in early cervical cancer
变量 β SE Waldχ2 P值 OR 95% CI 变量 β SE Waldχ2 P值 OR 95% CI 年龄 -1.384 0.665 4.334 0.037 0.251 0.068~0.922 FIGO分期 2.194 0.844 6.754 0.009 8.970 1.715~46.916 HPV -0.190 0.803 0.056 0.813 0.827 0.171~3.989 阴道受累 -0.464 0.829 0.313 0.576 0.629 0.124~3.191 MRI 1.667 0.640 6.784 0.009 5.298 1.511~18.576 间质浸润深度 -1.084 0.783 1.916 0.166 0.338 0.073~1.570 肿瘤大小 -0.375 0.687 0.258 0.612 0.738 0.162~2.922 淋巴血管间隙浸润 2.395 0.972 6.066 0.014 10.967 1.631~73.753 分化等级 -0.332 0.679 0.239 0.625 0.717 0.189~2.715 HIST1H3D表达 1.987 0.736 7.296 0.007 7.296 1.725~30.858 -
[1] BENÍTEZ-ARVIZU G, CASTRO-JÁCOME T P, TOVAR-PÉREZ E, et al. Antiproliferative, apoptotic, and antimigratory activities of kafirins on cervical cancer-derived cell lines[J]. Rev Med Inst Mex Seguro Soc, 2022, 61: 4-11. [2] 胡红, 李循律, 黄德旭, 等. EGFR和自噬相关蛋白Atg5、p62在宫颈癌中的表达及意义研究[J]. 河北医药, 2020, 42(18): 2760-2765. https://www.cnki.com.cn/Article/CJFDTOTAL-HBYZ202018008.htmHU H, LI X L, HUANG D X, et al. Expression and clinical significance of EGFR and autophagy-related proteins Atg5 and p62 in cervical cancer[J]. Hebei Medical Journal, 2020, 42(18): 2760-2765. https://www.cnki.com.cn/Article/CJFDTOTAL-HBYZ202018008.htm [3] TSUYOSHI H, TSUJIKAWA T, YAMADA S, et al. Diagnostic value of 18F-FDG PET/MRI for revised 2018 FIGO staging in patients with cervical cancer[J]. Diagnostics, 2021, 11: 202. doi: 10.3390/diagnostics11020202 [4] 古丽巴努·穆海麦提, 阿比丹·吐尔汗, 先君, 等. 外周血Treg细胞、T淋巴细胞及其亚群与早期宫颈癌的关系及对淋巴结转移的预测价值研究[J]. 现代生物医学进展, 2022, 22(12): 2308-2312. https://www.cnki.com.cn/Article/CJFDTOTAL-SWCX202212020.htmGULIBANU·Muhaimaiti, ABIDAN·Tuerhan, XIAN Jun, et al. The Relationship between peripheral blood treg cells, T lymphocytes and their subsets and early cervical cancer and the predictive value of lymph node metastasis[J]. Progress in Modern Biomedicine, 2022, 22(12): 2308-2312. https://www.cnki.com.cn/Article/CJFDTOTAL-SWCX202212020.htm [5] 赵小迎, 郑胡忠, 金纬纬, 等. 宫颈癌临床病理特征与盆腔淋巴结转移的相关性分析[J]. 中华全科医学, 2019, 17(3): 430-432. doi: 10.16766/j.cnki.issn.1674-4152.000700ZHAO X Y, ZHENG H Z, JIN W W, et al. Correlation between clinicopathological features and pelvic lymph node metastasis in cervical cancer[J]. Chinese Journal of General Practice, 2019, 17(3): 430-432. doi: 10.16766/j.cnki.issn.1674-4152.000700 [6] AREZZO F, CORMIO G, MONGELLI M, et al. Machine learning applied to MRI evaluation for the detection of lymph node metastasis in patients with locally advanced cervical cancer treated with neoadjuvant chemotherapy[J]. Arch Gynecol Obstet, 2022. DOI: 10.1007/s00404-022-06824-6. [7] YILDIRIM N, SAATLI B, KOSE S, et al. Predictability of myometrial, lower uterine segment and cervical invasion with 3D transvaginal ultrasonography and magnetic resonance imaging in endometrial cancer patients: a prospective cohort study[J]. Med Ultrason, 2018, 20: 348-54. doi: 10.11152/mu-1493 [8] BALCACER P, SHERGILL A, LITKOUHI B. MRI of cervical cancer with a surgical perspective: staging, prognostic implications and pitfalls[J]. Abdom Radiol (NY), 2019, 44: 2557-2571. doi: 10.1007/s00261-019-01984-7 [9] STOJILJKOVIC M, SOBIC S D, ODALOVIC S, et al. FDG PET-CT as an important diagnostic tool and prognostic marker in suspected recurrent cervical carcinoma after radiotherapy: comparison with MRI[J]. Radiol Oncol, 2022, 56(4): 453-460. doi: 10.2478/raon-2022-0042 [10] XIA X M, LI D D, DU W, et al. Radiomics based on nomogram predict pelvic lymphnode metastasis in early-stage cervical cancer[J]. Diagnostics (Basel), 2022, 12(10): 2446. doi: 10.3390/diagnostics12102446 [11] WANG X, LI S J, LIN X H, et al. Evaluation of tracer kinetic parameters in cervical cancer using dynamic contrast-enhanced MRI as biomarkers in terms of biological relevance, diagnostic performance and inter-center variability[J]. Front Oncol, 2022, 12: 958219. DOI: 10.3389/fonc.2022.958219. [12] HOLM J, GERKE O, VILSTRUP M H, et al. Improved stratification of stage-specific survival for cervical uterine cancer by integrating FDG-PET/CT and MRI for lymph node staging in 2018 FIGO classification[J]. Gynecol Oncol, 2022. DOI: 10.1016/j.ygyno.2022.09.021. [13] 周滑雪, 杜丹丽, 叶国柳. HIST1H3D基因在宫颈癌中的表达及其临床意义[J]. 实用癌症杂志, 2020, 35(12): 1969-1972. https://www.cnki.com.cn/Article/CJFDTOTAL-SYAZ202012014.htmZHOU H X, DU D L, YE G L. Expression and clinical significance of HIST1H3D in human cervical cancer[J]. The Practical Journal of Cancer, 2020, 35(12): 1969-1972. https://www.cnki.com.cn/Article/CJFDTOTAL-SYAZ202012014.htm [14] YE G L, WANG L Q, YANG K, et al. Fucoxanthin may inhibit cervical cancer cell proliferation via downregulation of HIST1H3D[J]. J Int Med Res, 2020, 48: 815-822. [15] CHEN J, WU Y, SUN Y, et al. Bacterial endotoxin decreased histone H3 acetylation of bovine mammary epithelial cells and the adverse effect was suppressed by sodium butyrate[J]. BMC Vet Res, 2019, 15(1): 267. [16] MOUBARAK R S, DE PABLOS-ARAGONESES A, ORTIZ-BARAHONA V, et al. The histone demethylase PHF8 regulates TGFβsignaling and promotes melanoma metastasis[J]. Sci Adv, 2022, 8(7): eabi7127. DOI: 10.1126/sciadv.abi7127. [17] WANG J N, ZHANG Q Y, LI Q, et al. Phase Ⅰ study and pilot efficacy analysis of entinostat, a novel histone deacetylase inhibitor, in chinese postmenopausal women with hormone receptor-positive metastatic breast cancer[J]. Target Oncol, 2021, 16: 591-599. [18] SINGH A K, BISHAYEE A, PANDEY A K. Targeting histone deacetylases with natural and synthetic agents: an emerging anticancer strategy[J]. Nutrients, 2018, 10(6): 731. -





 下载:
下载: