Analysis of etiology and inflammatory markers in patients with biliary tract infection after choledocchojejunostomy
-
摘要:
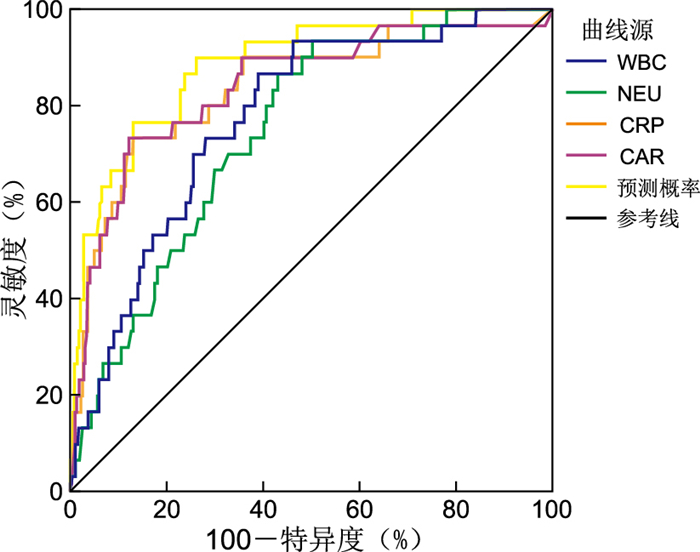
目的 调查本院胆肠吻合术后胆道感染致病菌病原学特点及耐药情况,并借助有关炎症标志物,来评价其诊断术后胆道感染的诊断效能。 方法 选取河南省人民医院2020年9月—2022年8月行胆肠吻合术的351例患者为研究对象,分析其胆道感染病原菌的特征和药敏试验结果,并评估白细胞计数、中性粒细胞计数、C-反应蛋白、CAR和SII水平在术后胆道感染诊断中的价值。 结果 351例行胆肠吻合术后患者中有31例发生胆道感染(为感染组,其余为非感染组),感染率为8.83%,共分离出致病菌36株,其中革兰阴性菌25株(69.4%)、革兰阳性菌8株(22.22%)和真菌3株(8.33%),常见致病菌有大肠埃希菌、肺炎克雷伯菌、屎肠球菌等,在革兰氏阴性细菌中,以大肠埃希菌和肺炎克雷伯菌对氨苄西林的耐药性最强,而对碳青霉烯类抗生素的耐药性最弱;术前2组患者WBC、NEU、CAR、CRP及SII水平差异均无统计学意义,术后次日、术后3 d两组患者的WBC、NEU、CAR及CRP高于术前(均P<0.05), 且感染组均高于非感染组(均P<0.05)。ROC曲线结果显示:联合指标的曲线下面积为0.887,各单个炎症指标均比联合指标预测价值低(均P<0.05)。 结论 本院行胆肠吻合术后出现的胆道感染主要由革兰阴性菌引起,例如肺炎克雷伯菌、大肠埃希菌等,且在常规抗生素治疗中具有较高的耐药性,可用于指导术后胆道感染经验性用药, 对患者术后血清WBC、NEU、CAR及CRP水平进行检测可以预测术后发生胆道感染的可能。 Abstract:Objective To investigate the pathogenic characteristics and drug resistance of pathogenic bacteria in biliary tract infection after cholangioenterostomy in Henan University People's Hospital and to evaluate the diagnostic value of biliary tract infection by relevant inflammatory markers. Methods A total of 351 patients who underwent choledocchojejunostomy from September 2020 to August 2022 in Henan Provincial People's Hospital were enrolled as the research objects. The characteristics of biliary tract infection pathogens and the results of drug sensitivity tests were analyzed. The levels of leukocytes, neutrophils, C-reactive protein (CRP), creactive protein-to-albumin ratio (CAR) and systemic immune-inflammation index (SII) were evaluated in diagnosing the occurrence of biliary tract infection. Results Among 351 patients, 31 had biliary tract infections (infection group, the rest were uninfected group), and the infection rate was 8.83%. A total of 36 strains of pathogenic bacteria were isolated, including 25 strains of Gram-negative bacteria (69.4%) and 8 strains of Gram-positive bacteria (22.22%) and 3 strains of fungi (8.33%). The common pathogens were Escherichia coli, Klebsiella pneumoniae and Enterococcus faecium. Among the Gram-negative bacteria, Escherichia coli and Klebsiella pneumoniae had the highest drug-resistance rates to ampicillin and the lowest drug-resistance rates to carbapenem antibiotics. There was no statistically significant difference in WBC, NEU, CAR, CRP, and SII levels between the two groups of patients before surgery. The level of NEU, CAR, WBC and CRP between the two groups on the second and third day after operation were higher than those before operation (all P < 0.05), and the infection group were higher than the uninfected group (all P < 0.05). The results of ROC curve showed that the area under the curve of combined indexes was 0.887, and its predictive value were higher than those of each individual index (all P < 0.05). Conclusion The main pathogenic bacteria of postoperative biliary tract infection in patients are Gram-negative bacteria such as Escherichia coli and Klebsiella pneumoniae, and they have strong drug-resistance to commonly used antibacterial drugs which can be used to guide postoperative preventive medication for biliary tract infection. The detection of serum WBC, NEU, CAR and CRP levels in patients can predict the occurrence of biliary tract infection after surgery. -
表 1 CJ术后胆道感染的病原菌类型和比例(n=36)
Table 1. Types and proportion of pathogenic bacteria in biliary tract infection after CJ surgery (n=36)
菌种 株 构成比(%) 革兰阴性菌 25 69.44 大肠埃希菌 17 47.20 肺炎克雷伯菌 3 8.33 阴沟肠杆菌 2 5.56 弗氏柠檬酸杆菌 2 5.56 阿氏肠杆菌 1 2.78 革兰阳性菌 8 22.22 屎肠球菌 5 13.89 粪肠球菌 1 2.78 鸟肠球菌 1 2.78 海氏肠球菌 1 2.78 真菌 3 8.33 白色念珠菌 3 8.33 表 2 革兰阴性菌对常见抗生素的耐药率(%)
Table 2. The resistance rate of gram-negative bacteria to common antibiotics (%)
抗菌药物 大肠埃希菌 肺炎克雷伯 阴沟肠杆菌 抗菌药物 大肠埃希菌 肺炎克雷伯 阴沟肠杆菌 氨苄西林 94.11 100.00 100.00 阿米卡星 0 33.33 0 哌拉西林 88.24 100.00 100.00 环丙沙星 88.24 66.67 100.00 阿莫西林克拉维酸 58.82 33.33 50.00 左氧氟沙星 82.35 66.67 50.00 氨苄西林舒巴坦 82.35 66.67 100.00 氯霉素 58.82 33.33 100.00 哌拉西林他唑巴坦 23.52 33.33 50.00 四环素 64.71 100.00 50.00 头孢呋辛 94.11 66.67 100.00 复方磺胺 58.82 100.00 0 头孢唑林 94.11 66.67 100.00 比阿培南 5.80 33.33 0 头孢噻肟 94.11 66.67 100.00 亚胺培南 5.88 33.33 0 头孢吡肟 88.24 66.67 0 美罗培南 5.88 33.33 0 头孢他啶 64.70 33.33 100.00 替加环素 0 0 0 头孢哌酮舒巴坦 35.29 66.67 50.00 氨曲南 70.59 66.67 100.00 头孢他啶阿维巴坦 5.88 0 0 多黏菌素 0 0 0 庆大霉素 47.05 33.33 0 表 3 革兰阳性菌对常见抗生素的耐药率(%)
Table 3. The resistance rate of gram-positive bacteria to common antibiotics (%)
抗菌药物 屎肠球菌 粪肠球菌 左氧氟沙星 60.00 100.00 氨苄西林 60.00 100.00 克林霉素 100.00 100.00 红霉素 80.00 100.00 庆大霉素筛选试验 20.00 100.00 利奈唑胺 0 0 妥布霉素 100.00 100.00 青霉素 80.00 100.00 利福平 40.00 100.00 复方磺胺 80.00 100.00 奎奴普丁达福普汀 20.00 0 替考拉宁 0 0 甲氧苄啶 100.00 100.00 万古霉素 0 0 阿莫西林克拉维酸 80.00 100.00 表 4 感染组与未感染组各指标水平比较[M(P25, P75)]
Table 4. Comparison of each index level between the infected group and the uninfected group [M(P25, P75)]
指标 时间 感染组 非感染组 H值 P值 WBC(×109/L) 术前 6.18(4.20, 7.91) 6.18(4.77, 7.44) 39.950a <0.001a 术后次日 13.03(11.58, 14.81) 8.20(8.10, 12.16) 346.810b <0.001b 术后3 d 15.34(12.45, 17.90) 9.30(6.84, 9.19) 24.030c 0.812c NEU(×109/L) 术前 4.08(2.58, 5.57) 4.02(3.03, 5.43) 35.620a <0.001a 术后次日 11.30(9.80, 13.25) 6.88(6.72, 10.84) 410.930b <0.001b 术后3 d 12.40(10.60, 15.31) 7.39(5.11, 7.44) 21.550c 0.231c CRP(mg/L) 术前 6.43(1.60, 24.44) 6.62(0.70, 15.63) 58.468a <0.001a 术后次日 72.30(28.19, 111.80) 14.61(7.49, 32.19) 299.698b <0.001b 术后3 d 79.95(31.20, 113.30) 14.82(5.40, 23.08) 2.441c 0.211c SII(×109/L) 术前 867.38(470.45, 1 355.82) 884.27(429.54, 1 221.33) 4.940a 0.714a 术后次日 3 103.50(1 924.58, 4 787.76) 2 749.68(1 475.05, 4 787.91) 266.218b 0.190b 术后3 d 3 006.94(1 787.14, 3 967.29) 1 589.12(927.73, 2 782.07) 3.434c 0.187c CAR(mg/g) 术前 0.16(0.04, 0.64) 0.14(0.02, 0.28) 58.286a <0.001a 术后次日 2.59(0.93, 3.61) 0.46(0.24, 0.98) 307.771b <0.001b 术后3 d 3.74(0.87, 3.80) 0.57(0.15, 0.66) 2.608c 0.214c 注:a为指标的组间效应;b为指标的时间效应;c为指标的组间与时间交互作用。 表 5 CJ胆道感染早期诊断的ROC曲线分析
Table 5. ROC curve analysis for early diagnosis of CJ biliary tract infection
指标 AUC 截断值 敏感度 特异度 阳性预测值 阴性预测值 95% CI 约登指数 WBC 0.774 11.095 0.389 0.523 0.073 0.900 0.696~0.853 0.477 NEU 0.747 9.435 0.867 0.570 0.163 0.980 0.609~0.825 0.437 CRP 0.839 48.035 0.733 0.869 0.351 0.971 0.754~0.923 0.602 CAR 0.840 1.675 0.733 0.879 0.370 0.971 0.757~0.923 0.612 联合 0.887 0.900 0.738 0.250 0.987 0.827~0.947 0.638 -
[1] KIM E Y, LEE S H, HONG T H. Palliative laparoscopic Roux-en-Y choledochojejunostomy as a feasible treatment option for malignant distal biliary obstruction[J]. Surg Today, 2022, 52(11): 1568-1575. doi: 10.1007/s00595-022-02513-8 [2] 邓雅文, 林海雄, 钟日辉, 等. 457例不同胆道疾病胆汁微生物培养及抗菌药物耐药性比较分析[J]. 中国卫生检验杂志, 2021, 31(1): 45-49. https://www.cnki.com.cn/Article/CJFDTOTAL-ZWJZ202101012.htmDENG Y W, LIN H X, ZHONG R H, et al. Microbiological culture and resistance analysis of bile from 457 cases with different biliary tract diseases[J]. Chinese Journal of Health Laboratory Technology, 2021, 31(1): 45-49. https://www.cnki.com.cn/Article/CJFDTOTAL-ZWJZ202101012.htm [3] CANENA J, LOPES L, FERNANDES J, et al. Influence of a novel classification of the papilla of vater on the outcome of needle-knife fistulotomy for biliary cannulation[J]. BMC Gastroenterol, 2021, 21(1): 147. doi: 10.1186/s12876-021-01735-3 [4] 廖米荣, 屠巍巍, 蔡立真. 中性粒细胞CD64指数与PCT及CRP对烧伤患者感染诊断的价值研究[J]. 中华全科医学, 2020, 18(6): 950-953. doi: 10.16766/j.cnki.issn.1674-4152.001400LIAO M R, TU W W, CAI L Z. The value of neutrophil CD64 index, PCT and CRP in diagnosis of infection in burn patients[J]. Chinese Journal of General Practice, 2020, 18(6): 950-953. doi: 10.16766/j.cnki.issn.1674-4152.001400 [5] 中华医学会外科学分会胆道外科学组. 急性胆道系统感染的诊断和治疗指南(2021版)[J]. 中华外科杂志, 2021, 59(6): 422-429. doi: 10.3760/cma.j.cn112139-20210421-00180Biliary tract Surgery Group, Surgery Society of Chinese Medical Association. Guidelines for diagnosis and treatment of acute biliary tract infections (2021)[J]. Chinese Journal of Surgery, 2021, 59(6): 422-429. doi: 10.3760/cma.j.cn112139-20210421-00180 [6] 高宇光. 肝胆胰腺肿瘤患者术后感染的病原菌分布及药敏分析[D]. 石家庄: 河北医科大学, 2017.GAO Y G. Pathogenic bacteria distribution and drug sensitivity analysis of postoperative infection in patients with hepatobiliary pancreatic tumor[D]. Shijiazhuang: Hebei Medical University, 2017. [7] 殷红莲, 汤国宁, 郭丽红. 胆道感染病原菌分布及耐药性分析[J]. 实用医技杂志, 2020, 27(1): 52-55. https://www.cnki.com.cn/Article/CJFDTOTAL-SYYJ202001030.htmYAN H L, TANG G N, GUO L H. Distribution and drug resistance of pathogenic bacteria in biliary tract infection[J]. Journal of Practical Medical Techniques, 2020, 27(1): 52-55. https://www.cnki.com.cn/Article/CJFDTOTAL-SYYJ202001030.htm [8] 邬丽娜, 宋毓飞, 周云, 等. 宁波地区3410例胆道感染患者胆汁培养病原菌分布及耐药性调查分析[J]. 现代实用医学, 2019, 31(5): 649-650. doi: 10.3969/j.issn.1671-0800.2019.05.042WU L N, SONG Y F, ZHOU Y, et al. Investigation and analysis of pathogen distribution and drug resistance in bile culture of 3 410 patients with biliary tract infection in Ningbo area[J]. Modern Practical Medicine, 2019, 31(5): 649-650. doi: 10.3969/j.issn.1671-0800.2019.05.042 [9] 张健, 刘鸿亚, 袁克文, 等. 某院113例胆道感染患者胆汁病原菌分布及耐药谱描述[J]. 中国校医, 2019, 33(1): 36-38. https://www.cnki.com.cn/Article/CJFDTOTAL-XIYI201901016.htmZHANG J, LIU H Y, YUAN K W, et al. Distribution of pathogenic bacteria and drug resistance spectrum analysis of bile in patients with biliary duct infection[J]. Chinese Journal of School Doctor, 2019, 33(1): 36-38. https://www.cnki.com.cn/Article/CJFDTOTAL-XIYI201901016.htm [10] DAVID J C, PIEDNOIR E, DELOUVéE S. Knowledge and perceptions of antibiotic resistance in the French population[J]. Infect Dis Now, 2022, 52(5): 306-310. doi: 10.1016/j.idnow.2022.03.004 [11] EL-DALATI S, CRONIN D, SHEA M, et al. Clinical Practice Update on Infectious Endocarditis[J]. Am J Med, 2020, 133(1): 44-49. doi: 10.1016/j.amjmed.2019.08.022 [12] 王穆群, 张永. 非鲍曼的不动杆菌的临床分布特征及耐药机制分析[J]. 中华全科医学, 2020, 18(10): 1645-1648. doi: 10.16766/j.cnki.issn.1674-4152.001582WANG M Q, ZHANG Y. Clinical distribution and antibiotics resistance mechanisms of non-baumannii Acinetobacter[J]. Chinese Journal of General Practice, 2020, 18(10): 1645-1648. doi: 10.16766/j.cnki.issn.1674-4152.001582 [13] 谢伟蓉, 汤敏婷, 朱文洪. 某院2020年细菌耐药情况及其与抗菌药物用药强度的相关性分析[J]. 临床合理用药杂志, 2022, 15(21): 160-163. https://www.cnki.com.cn/Article/CJFDTOTAL-PLHY202221050.htmXIE W R, TANG M T, ZHU W H. Analysis of bacterial drug resistance in a hospital in 2020 and its correlation with antimicrobial drug use intensity[J]. Chinese Journal of Clinical Rational Drug Use, 2022, 15(21): 160-163. https://www.cnki.com.cn/Article/CJFDTOTAL-PLHY202221050.htm [14] ÖZTVRK Z A, YESIL Y, KUYUMCU M E, et al. Inverse relationship between neutrophil lymphocyte ratio (NLR) and bone mineral density (BMD) in elderly people[J]. Arch Gerontol Geriatr, 2013, 57(1): 81-85. [15] WANG J, ZHOU D, DAI Z, et al. Association Between Systemic Immune-Inflammation Index and Diabetic Depression[J]. Clin Interv Aging, 2021, 16: 97-105. [16] HUANG Y, CHEN Y, ZHU Y, et al. Postoperative Systemic Immune-Inflammation Index (SII): a Superior Prognostic Factor of Endometrial Cancer[J]. Front Surg, 2021, 8: 704235. DOI: 10.3389/fsurg.2021.704235. [17] MACHADO V, BOTELHO J, ESCALDA C, et al. Serum C-reactive protein and periodontitis: a systematic review and meta-analysis[J]. Front Immunol, 2021, 12: 706432. DOI: 10.3389/fimmu.2021.706432. [18] 刘珍, 王峰, 高晖, 等. 血浆肝素结合蛋白联合降钙素原及C-反应蛋白对脓毒症及脓毒性休克患者诊断价值的研究[J]. 中国卫生检验杂志, 2021, 31(22): 2696-2701. https://www.cnki.com.cn/Article/CJFDTOTAL-ZWJZ202122003.htmLIU Z, WANG F, GAO H, et al. A study on the diagnostic value of plasma heparin binding protein combined with procalcitonin and C-reactive protein for patients with sepsis and septic shock[J]. Chinese Journal of Health Laboratory Technology, 2021, 31(22): 2696-2701. https://www.cnki.com.cn/Article/CJFDTOTAL-ZWJZ202122003.htm [19] GARCIA-MARTINEZ R, CARACENI P, BERNARDI M, et al. Albumin: pathophysiologic basis of its role in the treatment of cirrhosis and its complications[J]. Hepatology, 2013, 58(5): 1836-1846. [20] FERRAH N, CAMERON P, GABBE B, et al. Trends in the nature and management of serious abdominal trauma[J]. World J Surg, 2019, 43(5): 1216-1225. -





 下载:
下载: