Risk factors and long-term prognosis of malignant arrhythmia in elderly patients with dilated cardiomyopathy
-
摘要:
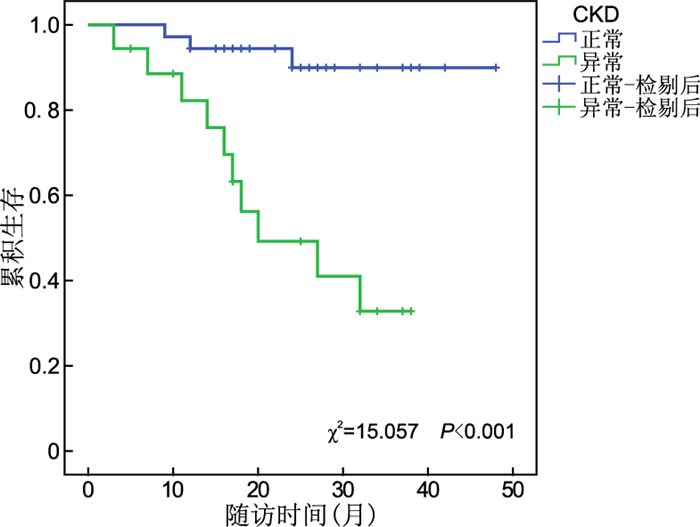
目的 筛查老年扩张型心肌病并发恶性心律失常(MA)的危险因素与影响该类患者临床预后的相关因素。 方法 选取2017年1月—2021年4月199例在遂宁市中心医院心血管中心住院的大于60岁的扩张型心肌病患者,根据资料是否并发恶性心律失常将其分为MA组(54例)与non-MA组(145例)。回顾性分析发生恶性心律失常的危险因素。并且对MA组进行随访,根据是否出现复合终点事件分为事件组与非事件组,并进行生存分析明确影响预后的因素。 结果 对MA组与non-MA组进行多因素logistic回归分析结果显示:慢性肾脏病、纽约心脏协会(NYHA)心功能分级Ⅲ~Ⅳ级、左室射血分数(LVEF)<35%、频发室性早搏是老年扩张型心肌病患者并发恶性心律失常的独立危险因素;对事件组与非事件组进行Kaplan-Meier生存分析显示:并发恶性心律失常的老年扩张型心肌病患者中,合并慢性肾脏病、慢性阻塞性肺疾病、频发室性早搏的患者心脏死亡风险更高。将Kaplan-Meier生存分析有意义的自变量纳入多因素Cox回归模型校正,结果显示合并慢性阻塞性肺疾病、频发室早是并发恶性心律失常的老年扩张型心肌病患者心脏死亡的独立危险因素(HR=7.593,95% CI:2.018~28.576,P=0.003;HR=4.090,95% CI:1.042~16.057,P=0.043)。 结论 慢性肾脏病、NYHA分级Ⅲ~Ⅳ级、LVEF<35%、频发室性早搏是老年扩张型心肌病患者恶性心律失常发生的潜在危险因素;事件组中,慢性阻塞性肺疾病、频发室早是影响预后的独立危险因素,能够较好地预测心源性死亡。 Abstract:Objective To investigate the risk factors and long-term prognosis of malignant arrhythmia (MA) in elderly patients with dilated cardiomyopathy. Methods A total of 199 patients with dilated cardiomyopathy over 60 years old who were hospitalized in the Cardiovascular Center of Suining Central Hospital were selected from January 2017 to April 2021. They were divided into MA group (54 cases) and non-MA group (145 cases) according to whether they were complicated with malignant arrhythmia. The risk factors of malignant arrhythmia were analyzed retrospectively. The MA group was followed up and divided into event group and non-event group according to the presence or absence of a composite endpoint event. The survival analysis was performed to clarify the factors affecting prognosis. Results Multifactorial logistic regression analysis of MA group and non-MA group showed that chronic kidney disease, NYHA class Ⅲ-Ⅳ, left ventricular ejection fration (LVEF) < 35%, and frequent premature ventricular beats were independent risk factors for complications of malignant arrhythmias in elderly patients with dilated cardiomyopathy. Kaplan-meier survival analysis of event group and non-event group showed that among elderly patients with dilated cardiomyopathy complicated by malignant arrhythmias, patients with comorbid chronic kidney disease, chronic obstructive pulmonary disease, and frequent premature ventricular beats were at higher risk of cardiac death. The independent variables that were significant for Kaplan-meier survival analysis were included in a multifactorial cox regression model correction, which showed that comorbid chronic obstructive pulmonary disease, frequent premature ventricular beats was an independent risk factor for cardiac death in elderly patients with dilated cardiomyopathy complicated by malignant arrhythmias (HR=7.593, 95% CI: 2.018-28.576, P=0.003; HR=4.090, 95% CI: 1.042-16.057, P=0.043). Conclusion Chronic kidney disease, NYHA class Ⅲ~Ⅳ, LVEF < 35%, and frequent premature ventricular beats are potential risk factors for the development of malignant arrhythmias in elderly patients with dilated cardiomyopathy. For event group, chronic obstructive pulmonary disease, and frequent premature ventricular beats are independent risk factors for prognosis and could better predict cardiac death. -
Key words:
- Dilated cardiomyopathy /
- Arrhythmia /
- Risk factors /
- Prognosis
-
表 1 MA组与non-MA组基线资料比较
Table 1. Comparison of baseline data between MA group and non-MA group
项目 Non-MA (n=145) MA (n=54) 统计量 P值 年龄(x±s,岁) 71.23±8.07 71.11±7.75 0.092a 0.927 性别[例(%)] 男性 106(73.1) 39(72.2) 0.015b 0.901 女性 39(26.9) 15(27.8) 慢性肾脏病[例(%)] 14(9.7) 18(33.3) 16.347b <0.001 慢性阻塞性肺疾病[例(%)] 14(9.7) 12(22.2) 5.471b 0.019 糖尿病[例(%)] 21(14.5) 5(9.3) 0.945b 0.331 频发室早[例(%)] 17(11.7) 20(37.0) 16.656b <0.001 β受体阻滞剂[例(%)] 135(93.1) 52(96.3) 0.257b 0.613 螺内酯[例(%)] 136(93.8) 49(90.7) 0.191b 0.662 ACEI/ARB[例(%)] 114(78.6) 31(57.4) 8.955b 0.003 ARNI[例(%)] 53(36.8) 15(27.8) 1.419b 0.233 SGLT2i[例(%)] 39(26.9) 16(29.6) 0.147b 0.701 高同型半胱氨酸血症[例(%)] 66(45.5) 34(63.0) 4.790b 0.029 低蛋白血症[例(%)] 33(22.8) 17(31.5) 1.591b 0.207 高甘油三酯[例(%)] 60(41.4) 26(48.1) 0.735b 0.391 LAEDD(x±s,mm) 43.82±3.84 46.51±3.98 -4.354a <0.001 LVEDD(x±s,mm) 59.46±5.54 63.28±6.28 -4.161a <0.001 LVEF<35%[例(%)] 17(11.7) 26(48.1) 30.817b <0.001 中重度二尖瓣反流[例(%)] 59(40.7) 39(72.2) 15.653b <0.001 附壁血栓[例(%)] 17(11.7) 13(24.1) 4.687b 0.030 LBBB[例(%)] 14(9.7) 8(14.8) 1.065b 0.302 RBBB[例(%)] 16(11.0) 7(13.0) 0.143b 0.705 Tp-Te间期(x±s,ms) 98.86±16.88 106.50±16.86 -2.839a 0.005 fQRS[例(%)] 11(7.6) 10(18.5) 4.982b 0.026 NYHA分级Ⅲ~Ⅳ级[例(%)] 84(57.9) 45(83.3) 11.135b 0.001 注:a为t值,b为χ2值。 表 2 不同危险因素预测恶性心律失常患病风险二元logistic回归分析
Table 2. Binary logistic regression analysis of different risk factors predicting the risk of malignant arrhythmia
变量 B SE Waldχ2 P值 OR (95% CI) 慢性肾脏病 1.248 0.482 6.702 0.010 3.483(1.354~8.957) NYHA Ⅲ~Ⅳ级 1.062 0.490 4.691 0.030 2.893(1.106~7.564) LVEF<35% 1.127 0.458 6.062 0.014 3.087(1.258~7.573) 频发室早 1.194 0.464 6.624 0.010 3.299(1.329~8.188) 表 3 影响心脏死亡的多因素Cox回归分析
Table 3. Multivariate Cox regression analysis of cardiac death
变量 β SE Waldχ2 P值 HR(95% CI) 慢性阻塞性肺疾病 2.027 0.676 8.988 0.003 7.593(2.018~28.576) 频发室早 1.409 0.698 4.076 0.043 4.090(1.042~16.057) -
[1] 中华医学会心血管病学分会, 中国心肌炎心肌病协作组. 中国扩张型心肌病诊断和治疗指南[J]. 临床心血管病杂志, 2018, 34(5): 421-434. doi: 10.13201/j.issn.1001-1439.2018.05.002Chinese Association of Cardiology Branch, Chinese myocarditis Cardiomyopathy Collaboration Group. Guidelines for diagnosis and treatment of dilated cardiomyopathy in China[J]. Journal of Clinical Cardiology, 2018, 34(5): 421-434. doi: 10.13201/j.issn.1001-1439.2018.05.002 [2] LIU X, YU H, PEI J, et al. Clinical characteristics and long-term prognosis in patients with chronic heart failure and reduced ejection fraction in China[J]. Heart Lung Circ, 2014, 23(9): 818-826. doi: 10.1016/j.hlc.2014.02.022 [3] ZEPPENFELD K, WIJNMAALEN A P, EBERT M, et al. Clinical outcomes in patients with dilated cardiomyopathy and ventricular tachycardia[J]. J Am Coll Cardiol, 2022, 80(11): 1045-1056. doi: 10.1016/j.jacc.2022.06.035 [4] SHIMOKAWA H. Trends in clinical characteristics, Treatments and prognosis in patients with dilated cardiomyopathy in japan-epidemiologic insights from the CHART Studies[J]. J Card Fail, 2016, 22(9): S154-S154. [5] ANGELIS G D, MERLO M, BARBATI G, et al. Longitudinal arrhythmic risk assessment based on ejection fraction in patients with recent-onset non-ischaemic dilated cardiomyopathy[J]. J Am Soc Echocardiogr, 2021, 35(8): 801-809. [6] YANCY C W, JESSUP M, BOZKURT B, et al. 2017 ACC/AHA/HFSA focused update of the 2013 ACCF/AHA guideline for the management of heart failure: a report of the american college of cardiology/american heart association task force on clinical practice guidelines and the Heart Failure Society of America[J]. J Card Fail, 2017, 23(8): 628-651. doi: 10.1016/j.cardfail.2017.04.014 [7] PONIKOWSKI P, VOORS A A, ANKER S D, et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure[J]. Kardiol Pol, 2016, 74(10): 1037-1147. doi: 10.5603/KP.2016.0141 [8] DI MARCO A, ANGUERA I, SCHMITT M, et al. Late gadolinium enhancement and the risk for ventricular arrhythmias or sudden death in dilated cardiomyopathy: systematic review and meta-analysis[J]. ACC Heart Fail, 2017, 5(1): 28-38. doi: 10.1016/j.jchf.2016.09.017 [9] MARCO A D, BROWN P, BRADLEY J, et al. Improved risk stratification for ventricular arrhythmias and sudden death in patients with nonischemic dilated cardiomyopathy[J]. J Am Coll Cardiol, 2021, 77(23): 2890-2905. doi: 10.1016/j.jacc.2021.04.030 [10] KHAN M Z, MUNIR M B, KHAN M U, et al. Sudden cardiac arrest in patients with chronic obstructive pulmonary disease: trends and outcomes from the national inpatient sample[J]. Am J Med Sci, 2022, 363(6): 502-510. doi: 10.1016/j.amjms.2021.10.025 [11] BRUSSELLE, GUY G, VERHAMME, et al. Cardiac effects of current treatments of chronic obstructive pulmonary disease[J]. Lancet Respir Med, 2016, 4(2): 149-164. doi: 10.1016/S2213-2600(15)00518-4 [12] RUSNAK J, BEHNES M, SCHUPP T, et al. COPD increases cardiac mortality in patients presenting with ventricular tachyarrhythmias and aborted cardiac arrest[J]. Respir Med, 2018, 145: 153-160. doi: 10.1016/j.rmed.2018.10.019 [13] WANG M T, LAI J H, TSAI C L, et al. Risk of adverse cardiovascular events with use of inhaled long-acting bronchodilators in management of chronic obstructive pulmonary disease[J]. J Food Drug Anal, 2019, 27(3): 657-670. doi: 10.1016/j.jfda.2018.12.006 [14] ZHANG Q X, ZHANG H F, WANG J J, et al. Indacaterol/glycopyrronium affects lung function and cardiovascular events in patients with chronic obstructive pulmonary diseases: a meta-analysis[J]. Heart Lung, 2021, 50(4): 532-541. doi: 10.1016/j.hrtlng.2021.02.018 [15] LIU S H, LO L W, CHOU Y H, et al. Renal denervation prevents myocardial structural remodeling and arrhythmogenicity in a chronic kidney disease rabbit model[J]. Heart Rhythm, 2021, 18(9): 1596-1604. doi: 10.1016/j.hrthm.2021.05.014 [16] SAMANTA R, CHAN C, CHAUHAN V. Arrhythmias and sudden cardiac death in end stage renal disease: epidemiology, risk factors, and management[J]. Can J Cardiol, 2019, 35(9): 1228-1240. doi: 10.1016/j.cjca.2019.05.005 [17] TALHA K M, JAIN V, YAMANI N, et al. Temporal trends and outcomes of implantable cardioverter defibrillators in heart failure and chronic kidney disease in the United States[J]. Curr Probl Cardiol, 2023, 45(4): 101548. DOI: 10.1016/j.cpcardiol.2022.101548. [18] 余福海, 沈才杰, 陆曹杰, 等. 慢性肾脏病患者心率变异性相关影响因素及预防对策[J]. 中华全科医学, 2021, 19(5): 798-800, 855. doi: 10.16766/j.cnki.issn.1674-4152.001920YU F H, SHEN C J, LU C J, et al. Related influencing factors and preventive measures of heart rate variability in patients uffer from chronic kidney disease[J]. Chinese Journal of General Practice, 2021, 19(5): 798-800, 855. doi: 10.16766/j.cnki.issn.1674-4152.001920 [19] MOK Y, BALLEW S H, MATSUSHITA K. Chronic kidney disease measures for cardiovascular risk prediction[J]. Atherosclerosis, 2021, 335: 110-118. doi: 10.1016/j.atherosclerosis.2021.09.007 [20] PUN P H, SMARZ T R, HONEYCUTT E F, et al. Chronic kidney disease is associated with increased risk of sudden cardiac death among patients with coronary artery disease[J]. Kidney Int, 2009, 76(6): 652-658. doi: 10.1038/ki.2009.219 [21] AL-KHATIB S M, STEVENSON W G, ACKERMAN M J, et al. 2017 AHA/ACC/HRS guideline for management of patients With ventricular arrhythmias and the prevention of sudden cardiac death: executive summary[J]. Heart Rhythm, 2017, 15(10): e190-e252. [22] LEE V, HEMINGWAY H, HARB R, et al. The prognostic significance of premature ventricular complexes in adults without clinically apparent heart disease: a meta-analysis and systematic review[J]. Heart, 2012, 98(17): 1290-1298. doi: 10.1136/heartjnl-2012-302005 [23] VOSKOBOINIK A, HADJIS A, ALHEDE C, et al. Predictors of adverse outcome in patients with frequent premature ventricular complexes: the ABC-VT risk score[J]. Heart Rhythm, 2020, 17(7): 1066-1074. doi: 10.1016/j.hrthm.2020.02.020 -





 下载:
下载: