Value of predicting liver failure after primary hepatocellular carcinoma resection based on two-dimensional shear wave elastography
-
摘要:
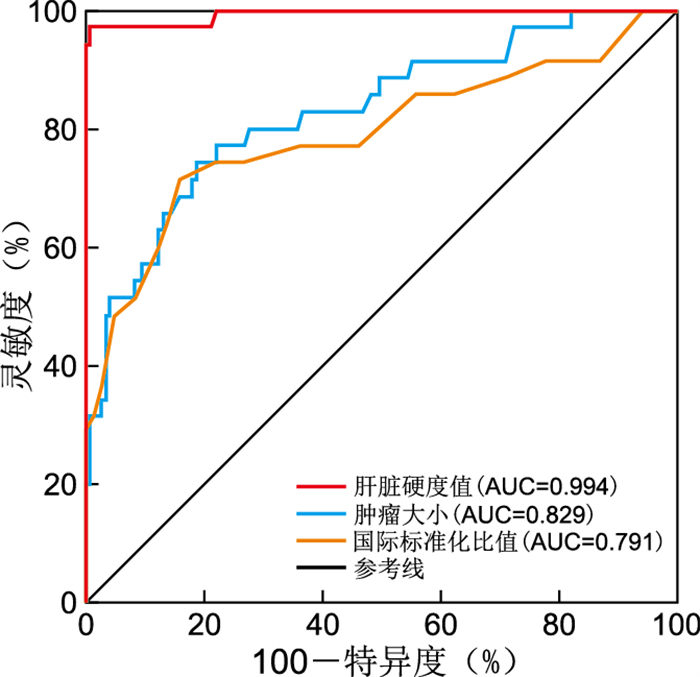
目的 探讨二维剪切波弹性成像(2D-SWE)预测原发性肝细胞癌切除术后肝衰竭的价值,帮助医师判断预后。 方法 回顾性分析2021年5月—2022年5月在浙江省荣军医院及浙江省中医院行原发性肝细胞癌切除术的180例患者的临床资料,根据术后是否发生肝衰竭分为肝衰竭组(35例)和非肝衰竭组(145例)。患者术前接受实验室和2D-SWE检查,经单因素分析和多因素logistic回归分析筛选出预测原发性肝细胞癌切除术后肝衰竭的危险因素,并分析其预测价值。 结果 单因素分析结果显示,肝衰竭组和非肝衰竭组在白蛋白、总胆红素、谷草转氨酶、γ-谷氨酰转移酶、凝血酶原时间、国际标准化比值及Child-Pugh评分、终末期肝病模型(MELD)评分、肿瘤大小、有肝门阻断、肝脏硬度值的差异有统计学意义(均P < 0.05)。经多因素logistic回归分析,国际标准化比值、肿瘤大小、肝脏硬度值是原发性肝细胞癌切除术后肝衰竭的独立影响因素(OR=5.078、4.943、5.073,均P < 0.05)。经ROC曲线分析,国际标准化比值、肿瘤大小、肝脏硬度值预测原发性肝细胞癌切除术后肝衰竭的曲线下面积为0.791、0.829、0.994,预测效能较好。 结论 基于2D-SWE预测原发性肝细胞癌切除术后肝衰竭的临床价值较高,国际标准化比值在1.01及以上、肿瘤大小在4.82 cm及以上、肝脏硬度值在10.66 kPa及以上是原发性肝细胞癌切除术后肝衰竭的独立危险因素。 Abstract:Objective To explore the value of two-dimensional shear wave elastography (2D-SWE) in predicting liver failure after resection of primary hepatocellular carcinoma (HCC) and to help doctors judge the prognosis. Methods The clinical data of 180 patients who underwent primary hepatocellular carcinoma resection in Zhejiang Provincial Veterans ' Hospital and Zhejiang Provincial Hospital of Traditional Chinese Medicine from May 2021 to May 2022 were analyzed retrospectively. They were divided into liver failure group (35 cases) and non-liver failure group (145 cases) according to whether there was liver failure after surgery. The patients received laboratory and 2D-SWE examination before operation. Through univariate analysis and multivariate logistic regression analysis, the risk factors for predicting liver failure after primary hepatocellular carcinoma resection were screened, and their predictive value was analyzed. Results Univariate analysis showed that there were significant differences in albumin, total bilirubin, aspartate aminotransferase, γ-glutamyltransferase, prothrombin time, international standardized ratio and Child Pugh score, model for end-stage liver disease (MELD) score, tumor size, hepatic portal occlusion, and liver hardness (all P < 0.05). Multivariate logistic regression analysis showed that international standardized ratio, tumor size and liver hardness were independent risk factors for liver failure after resection of primary hepatocellular carcinoma (OR=5.078, 4.943, 5.073, all P < 0.05). The ROC curve analysis results showed that the area under the curve for predicting liver failure after primary hepatocellular carcinoma resection using international standardized ratios, tumor size, and liver hardness values were 0.791, 0.829 and 0.994, with good prediction efficiency. Conclusion The clinical value of predicting liver failure after primary hepatocellular carcinoma resection based on 2D-SWE is high. International standardized ratios of 1.01 and above, tumor sizes of 4.82 cm and above, and liver hardness values of 10.66 kPa and above are independent risk factors for liver failure after primary hepatocellular carcinoma resection. -
表 1 肝衰竭组和非肝衰竭组患者一般资料比较
Table 1. Comparison of general data between liver failure group and nonliver failure group
组别 例数 性别[例(%)] 年龄(x±s,岁) 白蛋白(x±s,g/L) 总胆红素(x±s,μmol/L) 谷丙转氨酶(x±s,U/L) 天冬氨酸转氨酶(x±s,U/L) γ-谷氨酰转移酶(x±s,U/L) 男性 女性 肝衰竭组 35 32(91.43) 3(8.57) 56.22±8.94 37.55±6.23 15.72±2.49 32.26±5.39 37.31±6.42 76.48±16.55 非肝衰竭组 145 129(88.97) 16(11.03) 55.64±8.62 39.82±5.97 13.28±1.78 32.19±4.94 33.25±5.39 53.30±13.95 统计量 0.014a 0.354b 2.002b 6.693b 0.074b 3.849b 8.499b P值 0.905 0.723 0.047 < 0.001 0.941 < 0.001 < 0.001 组别 例数 凝血酶原时间(x±s,s) 国际标准化比值(x±s) Child-Pugh评分(x±s,分) MELD评分(x±s,分) 肿瘤大小(x±s,cm) 肝门阻断[例(%)] 肝脏硬度值(x±s,kPa) 有 无 肝衰竭组 35 12.16±1.13 1.03±0.06 6.00±1.00 7.56±1.25 5.32±0.87 12(34.29) 23(65.71) 12.99±1.47 非肝衰竭组 145 11.24±0.89 0.96±0.04 5.00±0.00 6.64±1.04 4.21±0.74 7(4.83) 138(95.17) 8.16±0.91 统计量 5.194b 8.349b 12.149b 4.510b 7.689b 22.888a 24.648b P值 < 0.001 < 0.001 < 0.001 < 0.001 < 0.001 < 0.001 < 0.001 注:a为χ2值,b为t值。 表 2 原发性肝细胞癌切除术后肝衰竭的变量赋值
Table 2. Variable assignment of liver failure after resection of primary hepatocellular carcinoma
变量 赋值方法 因变量 肝衰竭 未发生=0,发生=1 自变量 白蛋白 >37.75 g/L=0,≤37.75 g/L=1 总胆红素 < 14.24 μmol/L=0,≥14.24 μmol/L=1 谷草转氨酶 < 35.26 U/L=0,≥35.26 U/L=1 γ-谷氨酰转移酶 < 69.29 U/L=0,≥69.29 U/L=1 凝血酶原时间 < 11.57 s=0,≥11.57 s=1 国际标准化比值 < 1.01=0,≥1.01=1 Child-Pugh评分 < 5.44分=0,≥5.44分=1 MELD评分 < 6.85分=0,≥6.85分=1 肿瘤大小 < 4.82 cm=0,≥4.82 cm=1 肝门阻断 无=0,有=1 肝脏硬度值 < 10.66 kPa=0,≥10.66 kPa=1 表 3 原发性肝细胞癌切除术后肝衰竭的多因素logistic回归分析
Table 3. Multivariate logistic regression analysis of liver failure after primary hepatocellular carcinoma resection
变量 β SE Wald χ2 P值 OR值 95% CI 白蛋白 1.147 0.628 3.336 0.068 3.149 0.920~10.782 总胆红素 1.074 0.593 3.280 0.071 2.927 0.916~9.358 谷草转氨酶 0.963 0.528 3.326 0.069 2.620 0.931~7.373 γ-谷氨酰转移酶 0.854 0.493 3.001 0.084 2.349 0.894~6.174 凝血酶原时间 0.702 0.481 2.130 0.145 2.018 0.786~5.180 国际标准化比值 1.625 0.417 15.186 < 0.001 5.078 2.243~11.500 Child-Pugh评分 0.742 0.501 2.193 0.139 2.100 0.787~5.607 MELD评分 0.803 0.526 2.331 0.128 2.232 0.796~6.259 肿瘤大小 1.598 0.511 9.779 0.002 4.943 1.816~13.458 肝门阻断 0.884 0.573 2.380 0.124 2.421 0.787~7.442 肝脏硬度值 1.624 0.476 11.640 0.001 5.073 1.996~12.897 表 4 国际标准化比值、肿瘤大小、肝脏硬度值预测原发性肝细胞癌的价值
Table 4. Value of international normalized ratio, tumor size and liver hardness value in predicting primary hepatocellular carcinoma
指标 AUC 95% CI P值 截断值 约登指数 灵敏度(%) 特异度(%) 国际标准化比值 0.791 0.724~0.848 < 0.001 1.010 0.556 71.40 84.10 肿瘤大小 0.829 0.766~0.881 < 0.001 4.820 0.557 74.30 81.40 肝脏硬度值 0.994 0.968~1.000 < 0.001 10.660 0.965 97.10 99.30 -
[1] 王太成, 宋文渊, 赵红岩, 等. 肝细胞癌患者血清前白蛋白水平和自然杀伤细胞比率与肝切除术后发生急性肝衰竭的相关性分析[J]. 中华实用诊断与治疗杂志, 2021, 35(7): 676-679. https://www.cnki.com.cn/Article/CJFDTOTAL-HNZD202107007.htmWANG T C, SONG W Y, ZHAO H Y, et al. Correlations of serum prealbumin level and natural killer cell ratio with acute liver failure after hepatectomy in patients with hepatocellular carcinoma[J]. Journal of Chinese Practical Diagnosis and Therapy, 2021, 35(7): 676-679. https://www.cnki.com.cn/Article/CJFDTOTAL-HNZD202107007.htm [2] 麦荣云, 叶甲舟, 曾洁, 等. 血清前白蛋白-胆红素评分预测乙肝相关性肝细胞癌肝切除术后肝衰竭的价值[J]. 中华肝胆外科杂志, 2018, 24(11): 737-741. doi: 10.3760/cma.j.issn.1007-8118.2018.11.003MAI R Y, YE J Z, ZENG J, et al. Clinical significance of serum prealbumin-bilirubin score (PALBI) in predicting posthepatectomy liver failure in patients with HBV-related hepatocellular carcinoma[J]. Chinese Journal of Hepatobiliary Surgery, 2018, 24(11): 737-741. doi: 10.3760/cma.j.issn.1007-8118.2018.11.003 [3] 朱倩, 陈怡然, 徐畅, 等. 肝细胞癌破裂危险因素及其行肝切除术后临床预后分析[J]. 中国实用外科杂志, 2021, 41(8): 905-912, 918. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGWK202108020.htmZHU Q, CHEN Y R, XU C, et al. Predictors and clinical outcomes for spontaneous rupture of hepatocellular carcinoma among patients undergoing partial hepatectomy[J]. Chinese Journal of Practical Surgery, 2021, 41(8): 905-912, 918. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGWK202108020.htm [4] 陈皓, 马俊永, 钱利强, 等. 脾脏硬度和体积预测肝细胞癌患者肝切除术后发生肝功能衰竭的价值[J]. 临床肝胆病杂志, 2019, 35(12): 2725-2729. https://www.cnki.com.cn/Article/CJFDTOTAL-LCGD201912020.htmCHEN H, MA J Y, QIAN L Q, et al. Value of spleen stiffness and spleen volume in predicting posthepatectomy liver failure in patients with hepatocellular carcinoma[J]. Journal of Clinical Hepatology, 2019, 35(12): 2725-2729. https://www.cnki.com.cn/Article/CJFDTOTAL-LCGD201912020.htm [5] HU H, HAN H, HAN X K, et al. Nomogram for individualised prediction of liver failure risk after hepatectomy in patients with resectable hepatocellular carcinoma: the evidence from ultrasound data[J]. Eur Radiol, 2018, 28(2): 877-885. doi: 10.1007/s00330-017-4900-2 [6] 薛立云, 付甜甜, 丁红, 等. 二维剪切波弹性成像对原发性肝细胞癌切除术后肝衰竭的预测价值[J]. 中华医学杂志, 2020, 100(39): 3075-3080. doi: 10.3760/cma.j.cn112137-20200228-00506XUE L Y, FU T T, DING H, et al. Predictive value of two-dimentional shear wave elastography in posthepatoectomy liver failure[J]. National Medical Journal of China, 2020, 100(39): 3075-3080. doi: 10.3760/cma.j.cn112137-20200228-00506 [7] 中华人民共和国国家卫生健康委员会医政医管局. 原发性肝癌诊疗指南(2022年版)[J]. 中国实用外科杂志, 2022, 42(3): 241-273. https://www.cnki.com.cn/Article/CJFDTOTAL-XIBU202304002.htmMedical Administration Bureau of the National Health Commission of the People's Republic of China. Standardization for Diagnosis and Treatment of Primary Hepatic Carcinoma(2022 Edition)[J]. Chinese Journal of Practical Surgery, 2022, 42(3): 241-273. https://www.cnki.com.cn/Article/CJFDTOTAL-XIBU202304002.htm [8] 高梦丹, 张永宏, 赵艳. STAT1与STAT3在肝细胞癌及肝衰竭发病机制中的作用[J]. 临床肝胆病杂志, 2018, 34(9): 2017-2020. doi: 10.3969/j.issn.1001-5256.2018.09.040GAO M D, ZHANG Y H, ZHAO Y. Role of signal transduction and transcription factors STAT1 and STAT3 in the pathogenesis of hepatocellular carcinoma and liver failure[J]. Journal of Clinical Hepatology, 2018, 34(9): 2017-2020. doi: 10.3969/j.issn.1001-5256.2018.09.040 [9] 朱二畅, 鲁正, 徐建中, 等. 腹腔镜与开腹肝切除术治疗原发性肝细胞癌的临床疗效对比[J]. 中华全科医学, 2020, 18(11): 1845-1847, 1973. doi: 10.16766/j.cnki.issn.1674-4152.001634ZHU E C, LU Z, XU J Z, et al. Comparison of clinical efficacy of laparoscopic and open hepatectomy for primary hepatocellular carcinoma[J]. Chinese Journal of General Practice, 2020, 18(11): 1845-1847, 1973. doi: 10.16766/j.cnki.issn.1674-4152.001634 [10] 张长坤, 张龙辉, 王东, 等. 术前肝功能Child-Pugh评分与白蛋白-胆红素评分对肝癌患者肝切除术后肝衰竭和预后的预测价值[J]. 中华消化外科杂志, 2018, 17(5): 474-482.ZHANG C K, ZHANG L H, WANG D, et al. Value of the preoperative Child. Pugh score and albumin-bilirubin score predicting posthepatectomy liver failure and prognosis of patients with hepatocellular carcinoma[J]. Chinese Journal of Digestive Surgery, 2018, 17(5): 474-482. [11] 高杨, 张熙冰, 张春平, 等. 合并乙型肝炎的肝细胞癌切除术前FibroScan弹性值与术后肝衰竭严重程度及预后的相关性[J]. 贵州医科大学学报, 2018, 43(1): 114-117. https://www.cnki.com.cn/Article/CJFDTOTAL-GYYB201801027.htmGAO Y, ZHANG X B, ZHANG C P, et al. FibroScan Elasticity before Resection of Hepatocellular Carcinoma Complicated with Hepatitis B Associated with Severity and Prognosis of Postoperative Liver Failure[J]. Journal of Guizhou Medical University, 2018, 43(1): 114-117. https://www.cnki.com.cn/Article/CJFDTOTAL-GYYB201801027.htm [12] 谢雪焜, 王宗玉, 陈欣欣, 等. 4种评分系统预测肝细胞癌患者经肝动脉化疗栓塞术后肝衰竭的价值[J]. 中国肿瘤临床, 2020, 47(12): 614-620. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGZL202012007.htmXIE X K, WANG Z Y, CHEN X X, et al. Value of four scoring systems in predicting liver failure after transcatheter arterial chemoembolization in patients with hepatocellular carcinoma[J]. Chinese Journal of Clinical Oncolog, 2020, 47(12): 614-620. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGZL202012007.htm [13] 代鸿华, 张高明, 杨慧林, 等. γ-谷氨酰转移酶对原发性肝细胞癌术后患者预后的预测价值[J]. 癌症进展, 2019, 17(5): 589-591, 616. https://www.cnki.com.cn/Article/CJFDTOTAL-AZJZ201905025.htmDAI H H, ZHANG G M, YANG H L, et al. Prognostic predictive value of γ-glutamyltransferase in primary liver cell carcinoma[J]. Oncology Progress, 2019, 17(5): 589-591, 616. https://www.cnki.com.cn/Article/CJFDTOTAL-AZJZ201905025.htm [14] 陈晓杰, 黄敬杨, 翁亮, 等. 实时组织弹性成像技术对原发性肝细胞癌切除术后发生肝衰竭的价值分析[J]. 东南国防医药, 2018, 20(6): 575-579. https://www.cnki.com.cn/Article/CJFDTOTAL-DNGY201806004.htmCHEN X J, HUANG J Y, WENG L, et al. The study of real time tissue elastography for predicting the value of liver failure after hepatectomy in patients with primary hepatocellular carcinoma[J]. Military Medical Journal of Southeast China, 2018, 20(6): 575-579. https://www.cnki.com.cn/Article/CJFDTOTAL-DNGY201806004.htm [15] LONG H Y, ZHONG X, SU L Y, et al. Liver stiffness measured by two-dimensional shear wave elastography for predicting symptomatic post-hepatectomy liver failure in patients with hepatocellular carcinoma[J]. Ann Surg Oncol, 2022, 29(1): 327-336. [16] 龙海怡, 谢晓燕, 苏丽娅, 等. 基于剪切波弹性成像技术构建肝细胞癌切除术后肝衰竭预测模型[J]. 中华超声影像学杂志, 2020, 29(5): 399-404.LONG H Y, XIE X Y, SU L Y, et al. A model based on shear wave elastography to predict post-hepatectomy liver failure in patients with hepatocellular carcinoma[J]. Chinese Journal of Ultrasonography, 2020, 29(5): 399-404. [17] 赵子瑜, 王明强, 牛垚飞. 影响乙型肝炎肝硬化相关肝细胞癌患者肝切除术后急性肝衰竭的临床因素分析[J]. 肝脏, 2022, 27(10): 1092-1095. https://www.cnki.com.cn/Article/CJFDTOTAL-ZUAN202210012.htmZHAO Z Y, WANG M Q, NIU Y F. Clinical factors affecting liver failure in patients with HBV related hepatocellular carcinoma after hepatectomy[J]. Chinese Hepatology, 2022, 27(10): 1092-1095. https://www.cnki.com.cn/Article/CJFDTOTAL-ZUAN202210012.htm [18] 王诚, 陈厚斌, 田泽彬, 等. 抗凝血酶Ⅲ在预测肝细胞癌术后肝衰竭中的应用价值[J]. 实用临床医药杂志, 2019, 23(20): 66-69. https://www.cnki.com.cn/Article/CJFDTOTAL-XYZL201920018.htmWANG C, CHEN H B, TIAN Z B, et al. Value of antithrombin Ⅲ in prediction of liver failure after hepatocellular carcinoma operation[J]. Journal of Clinical Medicine in Practice, 2019, 23(20): 66-69. https://www.cnki.com.cn/Article/CJFDTOTAL-XYZL201920018.htm -





 下载:
下载: