Research on the monitoring of pathogens and the prediction model of risk factors for hospital-acquired pneumonia in intensive care unit
-
摘要:
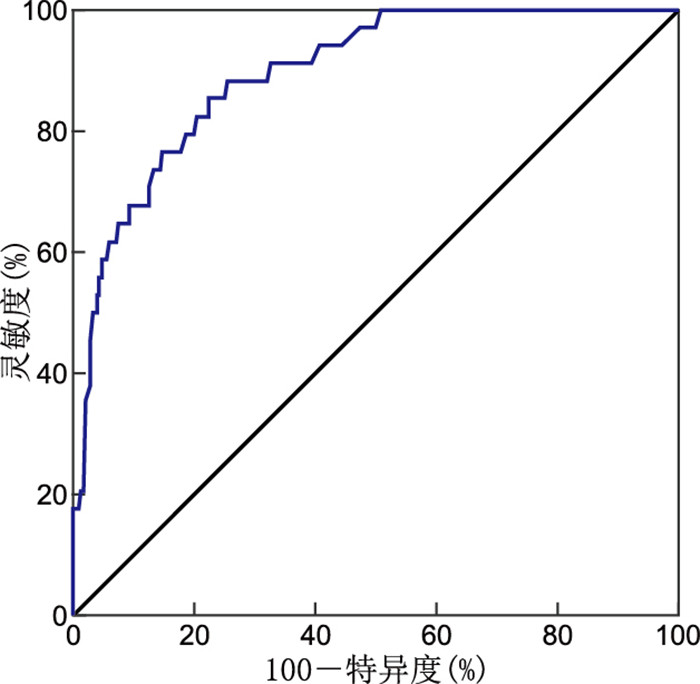
目的 研究重症监护室(ICU)医院获得性肺炎(hospital-acquired pneumonia,HAP)相关危险因素,了解HAP的病原菌构成。构建并评价HAP发生的风险因素预测模型,便于风险人群筛查,以防控HAP的发生。 方法 收集某综合性医院综合ICU 2020年1月—2021年3月住院患者资料,同时对痰标本分离病原菌进行监测。采用logistic回归分析构建HAP风险因素预测模型并评价。 结果 共纳入研究病例570例,其中HAP 34例。HAP患者痰标本中分离病原菌以革兰氏阴性菌为主。多因素分析显示,营养不良、侵袭性操作、住ICU天数>10 d、肺部慢性疾病是患者发生HAP的独立危险因素(均P<0.05)。建立回归模型:logit(P)=-7.870+2.496×营养不良+2.173×侵袭性操作+1.440×住ICU天数>10 d+1.054×肺部慢性疾病。Hosmer和Lemeshow拟合优度检验:χ2=3.022,P=0.933。ROC曲线下面积为0.895,95% CI为0.847~0.943。 结论 HAP患者痰标本分离菌以革兰氏阴性菌为主。营养不良、侵袭性操作、住ICU天数>10 d、肺部慢性疾病是ICU患者发生HAP的独立危险因素。利用logistic回归分析构建风险因素预测模型有较好的预测效果。 Abstract:Objective To study the risk factors of hospital-acquired pneumonia (HAP) in intensive care unit (ICU) and the composition of HAP pathogens. To construct and evaluate the risk prediction model of HAP, so as to facilitate the screening of risk population and prevent and control the occurrence of HAP. Methods Data of hospitalized patients in the comprehensive ICU of a general hospital from January 2020 to March 2021 were collected, and pathogenic bacteria were isolated and monitored. Logistic regression analysis was used to construct the risk factor prediction model and evaluate it. Results A total of 570 cases were included in this study, including 34 cases of HAP. The pathogens isolated from sputum specimens of HAP patients were mainly gram-negative bacteria. Multivariate analysis showed that malnutrition, invasive operation, length of stay in ICU>10 days and chronic pulmonary disease were independent risk factors for HAP (P < 0.05). Regression model was established: logit (P)=-7.870+2.496×alnutrition+2.173×nvasive operation+1.440×ength of stay in ICU>10 days+1.054×hronic pulmonary disease. Hosmer and Lemeshow goodness-of-fit test: χ2=3.022, P=0.933. The area under the ROC curve was 0.895, 95% CI was 0.847-0.943. Conclusion The bacteria isolated from HAP sputum specimens are mainly gram-negative bacteria. Malnutrition, invasive operation, length of stay in ICU>10 days and chronic pulmonary disease are independent risk factors for HAP in ICU patients. The risk factor prediction model constructed by logistic regression analysis can achieve better prediction effect. -
Key words:
- Hospital-acquired pneumonia /
- Intensive care unit /
- Risk prediction model
-
表 1 HAP检出病原菌构成情况(%)
Table 1. The composition of pathogenic bacteria(%)
细菌名称 株数 构成比(%) 革兰氏阴性菌 40 86.96 鲍曼不动杆菌 15 32.61 肺炎克雷伯菌 10 21.74 铜绿假单胞菌 5 10.87 大肠埃希菌 3 6.52 洋葱伯克霍尔德菌 3 6.52 嗜麦芽窄食单胞菌 2 4.35 阴沟肠杆菌 2 4.35 革兰氏阳性菌 3 6.52 金黄色葡萄球菌 2 4.35 人葡萄球菌 1 2.17 真菌 3 6.52 白色念珠菌 3 6.52 合计 46 100.00 表 2 HAP相关危险因素分析
Table 2. Analysis of HAP-related risk factors
因素 类别 非HAP(n=536) HAP(n=34) χ2值 P值 高龄 是 285 25 5.341 0.021 否 251 9 性别 男性 293 23 2.181 0.140 女性 243 11 吸烟 是 179 17 3.907 0.048 否 357 17 肺部慢性疾病 是 99 11 3.957 0.047 否 437 23 糖尿病 是 95 6 <0.001 0.991 否 441 28 住ICU天数>10 d 是 138 16 7.365 0.007 否 398 18 手术 是 267 23 4.069 0.044 否 269 11 营养不良 是 105 23 42.404 <0.001 否 431 11 联用抗菌药物 是 378 30 4.931 0.026 否 158 4 侵袭性操作 是 214 26 17.517 <0.001 否 322 8 恶性肿瘤 是 32 2 <0.001 0.983 否 504 32 表 3 变量赋值方法
Table 3. Variable assignment method
因素 赋值方法 发生HAP 是=1,否=0 高龄 是=1,否=0 吸烟 是=1,否=0 肺部慢性疾病 是=1,否=0 住ICU天数>10 d 是=1,否=0 手术 是=1,否=0 营养不良 是=1,否=0 联用抗菌药物 是=1,否=0 侵袭性操作 是=1,否=0 表 4 HAP危险因素的logistic多因素回归分析
Table 4. Logistic multivariate regression analysis of HAP risk factors
项目 B SE Wald χ2 P值 OR值 95% CI 营养不良 2.496 0.439 32.264 <0.001 12.132 5.128~28.704 侵袭性操作 2.173 0.477 20.732 <0.001 8.784 3.447~22.384 住ICU天数>10 d 1.440 0.438 10.807 0.001 4.219 1.788~9.953 肺部慢性疾病 1.054 0.453 5.415 0.020 2.869 1.181~6.972 -
[1] 夏品江, 张舸. 替加环素在多重或泛耐药鲍曼不动杆菌引起的重症医院获得性肺炎治疗中的运用价值[J]. 中华全科医学, 2017, 15(3): 404-406. doi: 10.16766/j.cnki.issn.1674-4152.2017.03.012XIA P J, ZHANG G. The value of the application of tigecycline in the treatment of severe hospital acquired pneumonia caused by multiple or pan drug resistant Acinetobacter baumannii[J]. Chinese Journal of General Practice, 2017, 15(3): 404-406. doi: 10.16766/j.cnki.issn.1674-4152.2017.03.012 [2] 黄琦, 王建林, 侯菊花. 改良式体位结合0.02%氯己定口腔护理对重症呼吸机相关性肺炎患者的预防效果[J]. 中华全科医学, 2018, 16(12): 2128-2130. doi: 10.16766/j.cnki.issn.1674-4152.000580HUANG Q, WANG J L, HOU J H. Analysis of preventive effect of modified posture combined with 0. 02% chlorhexidine oral care on ventilator-associated pneumonia in critically ill patients[J]. Chinese Journal of General Practice, 2018, 16(12): 2128-2130. doi: 10.16766/j.cnki.issn.1674-4152.000580 [3] MARTIN L I, RODRIGUEZ A H, TORRES A. New guidelines for hospital-acquired pneumonia/ventilator-associated pneumonia: USA vs. Europe[J]. Curr Opin Crit Care, 2018, 24(5): 347-352. doi: 10.1097/MCC.0000000000000535 [4] SHI Y, HUANG Y, ZHANG T T, et al. Chinese guidelines for the diagnosis and treatment of hospital-acquired pneumonia and ventilator-associated pneumonia in adults (2018 Edition)[J]. J Thorac Dis, 2019, 11(6): 2581-2616. doi: 10.21037/jtd.2019.06.09 [5] 王亚豪. 某医院2016—2019年住院患者肺部感染病原菌分布及影响因素[J]. 江苏预防医学, 2021, 32(3): 339-341. https://www.cnki.com.cn/Article/CJFDTOTAL-JSYF202103032.htmWANG Y H. Pathogenic bacteria distribution and influencing factors of pulmonary infection in hospitalized patients in a hospital from 2016 to 2019[J]. Jiangsu Journal of Preventive Medicine, 2021, 32(3): 339-341. https://www.cnki.com.cn/Article/CJFDTOTAL-JSYF202103032.htm [6] LIU B, LI S, LI H T, et al. Outcomes and prognostic factors of tigecycline treatment for hospital-acquired pneumonia involving multidrug-resistant Acinetobacter baumanii[J]. J Int Med Res, 2020, 48(4): 30-48. [7] 李金秀, 夏天, 潘童. 头孢哌酮舒巴坦钠与替加环素联合治疗ICU泛耐药鲍曼不动杆菌呼吸道感染的临床疗效及安全性[J]. 中国临床研究, 2017, 30(7): 886-889. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGCK201707006.htmLI J X, XIA T, PAN T. Clinical efficacy and safety of cefoperazone sulbactam sodium combined with tigecycline in treatment of respiratory tract infection of pan-drug-resistant Acinetobacter baumannii in ICU[J]. Chinese Journal of Clinical Research, 2017, 30(7): 886-889. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGCK201707006.htm [8] O'HARA L M, CALFEE D P, MILLER L G, et al. Optimizing contact precautions to curb the spread of antibiotic-resistant bacteria in hospitals: a multicenter cohort study to identify patient characteristics and healthcare personnel interactions associated with transmission of methicillin-resistant staphylococcus aureus[J]. Clin Infect Dis, 2019, 69(Suppl3): S171-S177. [9] BLANCO N, JOHNSON J K, SORKIN J D, et al. Transmission of resistant Gram-negative bacteria to healthcare personnel gowns and gloves during care of residents in community-based nursing facilities[J]. Infect Control Hosp Epidemiol, 2018, 39(12): 1425-1430. doi: 10.1017/ice.2018.247 [10] SANO M, SHINDO Y, TAKAHASHI K, et al. Risk factors for antibiotic resistance in hospital-acquired and ventilator-associated pneumonia[J]. J Infect Chemother, 2022, 28(6): 745-752. [11] 王玲. 耐多药结核病患者并发营养不良与肺部感染相关性的分析[J]. 中国医药指南, 2018, 16(16): 103-104. https://www.cnki.com.cn/Article/CJFDTOTAL-YYXK201816072.htmWANG L. Analysis of the correlation between malnutrition and pulmonary infection in patients with multi-drug resistant tuberculosis[J]. Guide of China Medicine, 2018, 16(16): 103-104. https://www.cnki.com.cn/Article/CJFDTOTAL-YYXK201816072.htm [12] GIULIANO K K, BAKER D, QUINN B, et al. The epidemiology of nonventilator hospital-acquired pneumonia in the United States[J]. Am J Infect Control, 2018, 46(3): 322-327. [13] 郑凌, 高磊, 叶静, 等. 呼吸重症监护病房HAP致病菌耐药性及其相关因素分析[J]. 安徽医科大学学报, 2021, 56(1): 134-137. https://www.cnki.com.cn/Article/CJFDTOTAL-YIKE202101026.htmZHENG L, GAO L, YE J, et al. Analysis of drug resistance and related factors of pathogenic bacteria of HAP in RICU[J]. Acta Universitatis Medicinalis Anhui, 2021, 56(1): 134-137. https://www.cnki.com.cn/Article/CJFDTOTAL-YIKE202101026.htm [14] YANG H J, FAN Y H, LI C H, et al. A retrospective study on risk factors and disease burden for hospital-acquired pneumonia caused by multi-drug-resistant bacteria in patients with intracranial cerebral hemorrhage[J]. Neurol Sci, 2022, 43(4): 2461-2467. [15] 霍盛红. 急诊气管插管后呼吸机相关性肺炎的危险因素分析[J]. 医药论坛杂志, 2019, 40(4): 41-43. https://www.cnki.com.cn/Article/CJFDTOTAL-HYYX201904014.htmHUO S H. Risk factors of ventilator-associated pneumonia after emergency endotracheal intubation[J]. Journal of Medical Forum, 2019, 40(4): 41-43. https://www.cnki.com.cn/Article/CJFDTOTAL-HYYX201904014.htm -





 下载:
下载: