Risk factors for ventilator-associated pneumonia after mechanical thrombectomy in acute ischemic stroke
-
摘要:
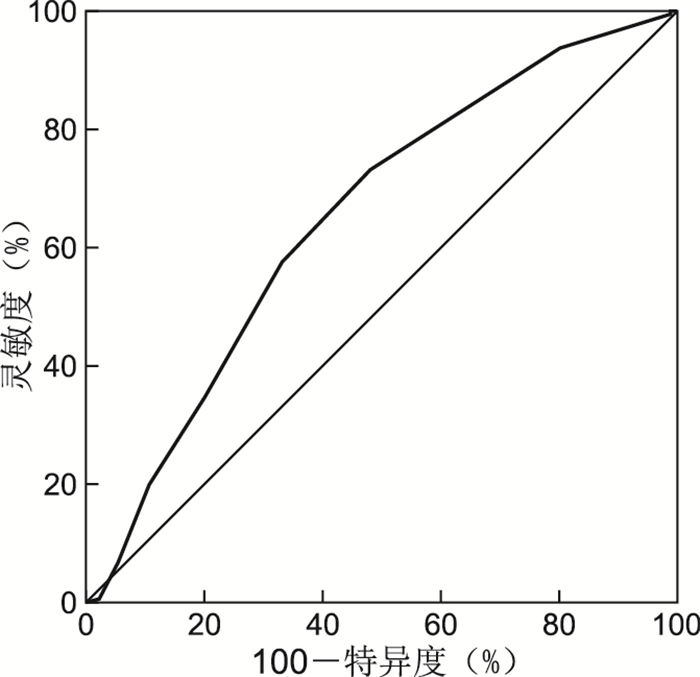
目的 探讨急性脑梗死机械取栓术后并发呼吸机相关性肺炎(VAP)的危险因素及A2DS2评分量表的预测价值。 方法 回顾性收集2020年1月—2021年12月在中国科学技术大学附属第一医院神经内科因急性脑梗死行机械取栓住院的273例患者的临床病例资料,根据是否合并VAP分为VAP组(180例)和非VAP组(93例)。对所有患者进行A2DS2评分,采用多因素logistic回归分析探究不同因素与肺炎的关系,采用受试者工作特征曲线(ROC)评价A2DS2量表对VAP的预测价值。 结果 年龄、住院时间、高血压病史、随机血糖、美国国立卫生研究院卒中量表(NIHSS)评分、中性粒细胞与淋巴细胞比值(NLR)、A2DS2评分与VAP发生相关(均P<0.05);住院时间长及既往高血压病史是VAP发生的独立危险因素(OR=1.112,95% CI: 1.053~1.173,P < 0.001;OR=1.970,95% CI: 1.130~3.433,P=0.017);A2DS2≥5分是VAP发生的独立危险因素(OR=2.412,95% CI: 1.382~4.210,P=0.002);A2DS2评分量表对VAP有预测价值(AUC为0.651,95% CI:0.580~0.721,灵敏度为0.733,特异度为0.484,最佳截断值为5分)。 结论 年龄、住院时间、高血压病史、随机血糖、NIHSS评分、NLR、A2DS2评分与VAP发生相关;住院时间长、既往高血压病史、高A2DS2评分是VAP的独立危险因素;A2DS2评分量表对卒中合并VAP有预测价值。 Abstract:Objective To investigate the risk factors of ventilator-associated pneumonia (VAP) after mechanical thrombectomy in acute stroke and the predictive value of A2DS2 score scale. Methods From January 2020 to December 2021, the clinical data of 273 patients admitted to the Department of Neurology, the First Affiliated Hospital, University of Science and Technology of China (USTC) for acute cerebral infarction were retrospectively collected. The patients were divided into VAP group (180 cases) and non-VAP group (93 cases). A2DS2 scores were obtained for all patients. Multivariate logistic regression analysis was used to investigate the relationship between various factors and pneumonia. Receiver operating characteristic curve (ROC) was used to evaluate the predictive value of the A2DS2 scale for VAP. Results Age, length of hospital stay, history of hypertension, random blood glucose, NIHSS score, neutrophil to lymphocyte ratio (NLR), A2DS2 score were correlated with VAP (all P < 0.05). length of hospital stay and history of hypertension were independent risk factors for VAP (OR=1.112, 95% CI: 1.053-1.173, P < 0.001; OR=1.970, 95% CI: 1.130-3.433, P=0.017); A2DS2≥5 points was an independent risk factor for VAP (OR=2.412, 95% CI: 1.382-4.210, P=0.002). The A2DS2 score scale had predictive value for VAP (AUC=0.651, 95% CI: 0.580-0.721, sensitivity was 0.733, specificity was 0.484, and optimal cut-off value was 5 points). Conclusion Age, hospitalization days, history of hypertension, random blood glucose, NIHSS score, NLR, A2DS2 score were correlated with VAP. Long hospital stay, history of hypertension and high A2DS2 score were independent risk factors for VAP. The A2DS2 score scale has predictive value for stroke combined with VAP. -
表 1 VAP组与非VAP组AIS患者基线资料比较
Table 1. Comparison of baseline characteristics between VAP and non-VAP groups in AIS patients
项目 总体(273例) VAP组(180例) 非VAP组(93例) 统计量 P值 年龄[M(P25, P75),岁] 67(57,76) 68(58,77) 66(54,73) -2.188a 0.029 性别(男性/女性,例) 166/107 112/68 54/39 0.445b 0.505 住院时间[M(P25, P75),d] 12(8,16) 13(9,18) 10(8,13) -4.493a <0.001 既往高血压[例(%)] 163(59.7) 118(65.6) 45(48.4) 7.513b 0.006 既往冠心病[例(%)] 91(33.3) 56(31.1) 35(37.6) 1.174b 0.279 既往糖尿病[例(%)] 48(17.6) 35(19.4) 13(14.0) 1.264b 0.261 既往房颤[例(%)] 91(33.3) 59(32.8) 32(34.4) 0.073b 0.786 既往吸烟[例(%)] 72(26.4) 48(26.7) 24(25.8) 0.011b 0.918 既往饮酒[例(%)] 56(20.5) 34(18.9) 22(23.6) 1.031b 0.310 收缩压[M(P25, P75),mmHg] 135(120,153) 137(119,157) 131(121,150) -1.378a 0.168 血糖[M(P25, P75),mmol/L] 7.340(6.190,8.560) 7.505(6.403,9.103) 7.03(5.705,7.995) -2.910a 0.004 中性粒细胞计数[M(P25, P75),109/L] 7.940(6.365,9.350) 8.030(6.425,9.453) 7.57(6.280,9.090) -1.334a 0.182 淋巴细胞计数[M(P25, P75),109/L] 1.170(0.865,1.570) 1.160(0.860,1.485) 1.220(0.905,1.670) -1.227a 0.220 NLR[M(P25, P75)] 6.800(4.630,9.660) 7.020(4.980,10.640) 5.790(4.360,8.590) -2.023a 0.043 肌酐[M(P25, P75),μmol/L] 66.00(56.00,81.00) 67.50(57.25,81.75) 64.00(54.00,77.50) -0.927a 0.354 尿酸[M(P25, P75),μmol/L] 296(235,368) 301(235,371) 280(230,351) -0.812a 0.417 NIHSS评分[M(P25, P75),分] 14(11,18) 15(12,19) 13(10,15) -3.333a 0.001 A2DS2评分[M(P25, P75),分] 5(4,7) 6(4,7) 4(4,6) -4.151a <0.001 前循环卒中[例(%)] 39(14.3) 28(15.6) 11(11.8) 0.696b 0.404 注: a为Z值,b为χ2值。1 mmHg=0.133 kPa。 表 2 AIS患者发生VAP影响因素的多因素logistic回归分析
Table 2. Multivariable logistic regression analysis of risk factors for VAP in patients with AIS
项目 B SE Wald χ2 P值 OR(95% CI) 住院时间 0.106 0.028 14.665 <0.001 1.112(1.053~1.173) 既往高血压病史 0.678 0.283 5.724 0.017 1.970(1.130~3.433) 随机血糖 0.102 0.067 2.305 0.129 1.107(0.971~1.262) NLR 0.018 0.033 0.321 0.571 1.020(0.956~1.086) A2DS2≥5分 0.881 0.284 9.604 0.002 2.412(1.382~4.210) -
[1] 中华医学会神经病学分会, 中华医学会神经病学分会脑血管病学组. 中国急性缺血性脑卒中诊治指南2018[J]. 中华神经科杂志, 2018, 51(9): 666-682. doi: 10.3760/cma.j.issn.1006-7876.2018.09.004Cerebrovascular Group, Chinese Society of Neurology, Chinese Society of Neurology. Chinese Guidelines for Diagnosis and Treatment of acute ischemic Stroke 2018[J]. Chinese Journal of Neurology, 2018, 51(9): 666-682. doi: 10.3760/cma.j.issn.1006-7876.2018.09.004 [2] 中华医学会神经病学分会, 中华医学会神经病学分会脑血管病学组, 中华医学会神经病学分会神经血管介入协作组. 中国急性缺血性脑卒中早期血管内介入诊疗指南2022[J]. 中华神经科杂志, 2022, 55(6): 565-580. https://www.cnki.com.cn/Article/CJFDTOTAL-LCLZ202307020.htmChinese Society of Neurology, Cerebral Vascular Group, Neurovascular Intervention Group, Chinese Society of Neurology. Guidelines for early endovascular intervention in acute ischemic stroke in China 2022[J]. Chinese Journal of Neurology, 2022, 55(6): 565-580. https://www.cnki.com.cn/Article/CJFDTOTAL-LCLZ202307020.htm [3] SMITH C J, KISHORE A K, VAIL A, et al. Diagnosis of stroke associated pneumonia: recommendations from the pneumonia in stroke consensus group[J]. Stroke, 2015, 46(8): 2335-2340. doi: 10.1161/STROKEAHA.115.009617 [4] KISHORE A K, JEANS A R, GARAU J, et al. Antibiotic treatment for pneumonia complicating stroke: recommendations from the pneumonia in stroke consensus (PISCES) group[J]. Eur Stroke J, 2019, 4(4): 318-328. doi: 10.1177/2396987319851335 [5] 董漪, 叶婷, 董强. 卒中后呼吸系统感染气道管理专家指导意见[J]. 中国卒中杂志, 2021, 16(6): 602-610. https://www.cnki.com.cn/Article/CJFDTOTAL-ZUZH202106015.htmDONG Y, YE T, DONG Q. Experts consensus on post-stroke respiratory tract infection management[J]. Chinese Journal of Stroke, 2021, 16(6): 602-610. https://www.cnki.com.cn/Article/CJFDTOTAL-ZUZH202106015.htm [6] 中国卒中学会急救医学分会, 中华医学会急诊医学分会卒中学组, 中国老年医学学会急诊医学分会, 等. 卒中相关性肺炎诊治中国专家共识(2019更新版)[J]. 中国卒中杂志, 2019, 14(12): 1251-1262. https://www.cnki.com.cn/Article/CJFDTOTAL-ZUZH201912014.htmEmergency Medicine Branch of Chinese Stroke Society, Stroke Group of Emergency Medicine Branch of Chinese Medical Association, Emergency Medicine Branch of Chinese Geriatric Society, et al. An updated Chinese consensus statement on stroke-associated pneumonia 2019[J]. Chinese Journal of Stroke, 2019, 14(12): 1251-1262. https://www.cnki.com.cn/Article/CJFDTOTAL-ZUZH201912014.htm [7] MUHL H, ROTH C, SCHRÖTER A, et al. Pneumonia in acute ischemic stroke patients with proximal occlusions within the anterior circulation after endovascular therapy or systemic thrombolysis[J]. J Clin Med, 2022, 11(3): 482. doi: 10.3390/jcm11030482 [8] ZHU Y B, GAO J, LV Q S, et al. Risk factors and outcomes of stroke-associated pneumonia in patients with stroke and acute large artery occlusion treated with endovascular thrombectomy[J]. J Stroke Cerebrovasc Dis, 2020, 29(11): 105223. DOI: 10.1016/j.jstrokecerebrovasdis.2020.105223. [9] ZHANG X M, XIAO L, NIU L Q, et al. Comparison of six risk scores for stroke-associated pneumonia in patients with acute ischemic stroke: a systematic review and Bayesian network meta-analysis[J]. Front Med (Lausanne), 2022, 9: 964616. DOI: 10.3389/fmed.2022.964616. [10] JI R J, SHEN H P, PAN Y S, et al. Novel risk score to predict pneumonia after acute ischemic stroke[J]. Stroke, 2013, 44(5): 1303-1309. doi: 10.1161/STROKEAHA.111.000598 [11] SMITH C J, BENJAMIN D B, HOFFMAN A, et al. Can a novel clinical risk score improve pneumonia prediction in acute stroke care? A UK multicenter cohort study[J]. J Am Heart Assoc, 2015, 4(1): 1307-1316. [12] HOFFMANN S, MALZAHN U, HARMS H, et al. Development of a clinical score (A2DS2) to predict pneumonia in acute ischemic stroke[J]. Stroke, 2012, 43(10): 2617-2623. doi: 10.1161/STROKEAHA.112.653055 [13] ZAPATA-ARRIAZA E, MONICHE F, BLANCA P G, et al. External validation of the ISAN, A2DS2, and AIS-APS scores for predicting stroke-associated pneumonia[J]. J Stroke Cerebrovasc Dis, 2018, 27(3): 673-676. doi: 10.1016/j.jstrokecerebrovasdis.2017.09.059 [14] 陈云, 徐敏, 张力壬, 等. A2DS2评分联合中性粒细胞与淋巴细胞比值对急性缺血性卒中相关性肺炎的预测价值[J]. 中国临床医学, 2020, 27(5): 806-810. https://www.cnki.com.cn/Article/CJFDTOTAL-LCYX202005018.htmCHEN Y, XU M, ZHANG L R, et al. A2DS2 combined with neutrophil-to-lymphocyte ratio in the prediction of acute ischemic stroke-associated pneumonia[J]. Chinese Journal Of Clinical Medicine, 2020, 27(5): 806-810. https://www.cnki.com.cn/Article/CJFDTOTAL-LCYX202005018.htm [15] HOFLER S F, HESCHLB S, KNEIHSL M, et al. Ventilation time and prognosis after stroke thrombectomy: the shorter, the better![J]. Eur J Neurol, 2020, 27(5): 849-855. doi: 10.1111/ene.14178 [16] 刘玉岭, 夏宏林, 张会平, 等. 综合医院呼吸机相关性肺炎发生情况及相关因素分析[J]. 中华全科医学, 2022, 20(4): 685-687. doi: 10.16766/j.cnki.issn.1674-4152.002430LIU Y L, XIA H L, ZHANG H P, et al. Analysis on the incidence and related factors of ventilator-related pneumonia in a general hospital[J]. Chinese Journal of General Practice, 2022, 20(4): 685-687. doi: 10.16766/j.cnki.issn.1674-4152.002430 [17] 中华医学会呼吸病学分会感染学组. 中国成人医院获得性肺炎与呼吸机相关性肺炎诊断和治疗指南(2018年版)[J]. 中华结核和呼吸杂志, 2018, 41(4): 255-280.Infectious Diseases Group, Respiratory Society, Chinese Medical Association. Guidelines for the diagnosis and treatment of hospital-acquired pneumonia and ventilator-associated pneumonia in Chinese adults (2018 edition)[J]. Chinese Journal of Tuberculosis and Respiratory Diseases, 2018, 41(4): 255-280. [18] LIU D D, CHU S F, CHEN C, et al. Research progress in stroke-induced immunodepression syndrome (SIDS) and stroke-associated pneumonia (SAP)[J]. Neurochem Int, 2018, 114: 42-54. [19] CUGY E, SIBON I. Stroke-associated pneumonia risk score: validity in a French Stroke Unit[J]. J Stroke Cerebrovasc Dis, 2017, 26(1): 225-229. [20] THOMAS R. Risk factors for pneumonia in patients with acute ischaemic stroke: a retrospective study[J]. J Clin Diagn Res, 2021, 15(1): 805-807. -





 下载:
下载: