Analysis of the efficacy of endoscopic submucosal dissection for early gastric cancer and precancerous lesions
-
摘要:
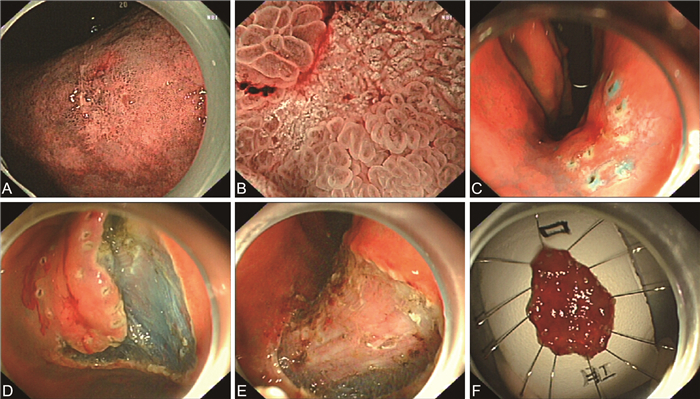
目的 研究内镜黏膜下剥离术(ESD)治疗早期胃癌(EGC)及癌前病变的安全性及有效性。 方法 对2019年1月1日—2022年12月31日期间在蚌埠医学院第一附属医院消化内镜中心行ESD治疗的110例EGC及癌前病变患者的临床病历资料进行回顾性分析,观察指标包括病灶特点、病理情况、手术并发症、术后复发情况等,比较ESD术前、术后病理结果差异,收集ESD术后合并迟发性出血组与未出血组患者的性别、年龄、病灶直径、病灶部位、是否合并术中穿孔、术后病理结果等数据并探讨ESD术后合并迟发性出血的影响因素。 结果 经ESD治疗的110例患者,整块切除率为100.0%(110/110),完整切除率为95.5%(105/110),治愈性切除率为93.6%(103/110)。术后病理:低级别上皮内瘤变54例,高级别上皮内瘤变30例,黏膜内癌20例,黏膜下癌6例,术前、术后病理差异有统计学意义(P<0.05)。术后延迟出血6例,均发生在术后24 h内,单因素分析显示,病灶直径≥3 cm可能与ESD术后发生迟发性出血有关(P<0.05)。术中穿孔3例,所有患者均无术后延迟性穿孔现象发生。随访截至2023年2月28日,110例患者均成功随访,术后随访3~50个月,中位随访时间23个月,全部患者均未复发。 结论 ESD术为治疗EGC及癌前病变安全有效的手术方式,但需严格掌握适应证,精准的术前评估尤为重要。 Abstract:Objective To study the safety and efficacy of endoscopic submucosal dissection (ESD) for early gastric cancer (EGC) and precancerous lesions. Methods The clinical data of 110 patients with EGC and precancerous lesions treated with ESD in the Digestive Endoscope Center of the First Affiliated Hospital of Bengbu Medical College from January 1, 2019 to December 31, 2022 were analyzed retrospectively. The observation indexes included the characteristics of the focus, pathology, operative complications, postoperative recurrence and so on, and the difference of pathological results was compared before and after ESD. The data of sex, age, lesion diameter, focus location, intraoperative perforation and postoperative pathological results of patients with delayed hemorrhage after ESD and non-bleeding group were collected, and the risk factors of delayed hemorrhage after ESD were explored. Results In 110 patients treated with ESD, the overall resection rate was 100.0% (110/110), the complete resection rate was 95.5% (105/110), and the curative resection rate was 93.6% (103/110). Postoperative pathology: low-grade intraepithelial neoplasia was 54, high-grade intraepithelial neoplasia was 30, intramucosal carcinoma was 20 and submucosal carcinoma was 6. There was significant difference between preoperative and postoperative pathology (P < 0.05). Delayed bleeding occurred in 6 cases, all of which occurred within 24 hours after operation. Univariate analysis showed that the lesion diameter≥3 cm might be related to delayed bleeding after ESD. There were 3 cases of intraoperative perforation, and no delayed perforation occurred in all patients. Up to February 28, 2023, 110 patients were successfully followed up for 3 to 50 months, with a median follow-up period of 23 months. All patients had no recurrence. Conclusion ESD is a safe and effective surgical procedure for the treatment of EGC and precancerous lesions, but strict indications are required and accurate preoperative evaluation is particularly important. -
表 1 110例早期胃癌及癌前病变患者ESD术前、术后病理结果比较[例(%)]
Table 1. Comparison of pre- and post-operative pathological results in 110 patients with early gastric cancer and precancerous lesions undergoing ESD [cases (%)]
时间 低级别上皮内瘤变 高级别上皮内瘤变 黏膜内癌 黏膜下癌 ESD术前 49(44.5) 52(47.3) 6(5.5) 3(2.7) ESD术后 54(49.1) 30(27.3) 20(18.2) 6(5.5) 注:ESD手术前后比较,χ2=17.730,P=0.007。 表 2 不同临床特征患者ESD并发迟发性出血情况比较(例)
Table 2. Comparison of delayed bleeding incidence in patients undergoing ESD with different clinical characteristics (cases)
项目 迟发性出血组
(n=6)未出血组
(n=104)χ2值 P值 性别 0.104 0.747 男性 4 72 女性 2 32 年龄(岁) 0.176 0.675 ≤60 2 53 >60 4 51 病灶直径(cm) 0.004a ≤3 2 92 >3 4 12 病灶部位 6.461 0.087 贲门 4 25 胃底 1 5 胃体 0 13 胃角 0 15 胃窦 1 46 合并术中穿孔 0.156a 是 1 2 否 5 102 术后病理 1.732 0.625 低级别上皮内瘤变 2 52 高级别上皮内瘤变 3 27 黏膜内癌 1 19 黏膜下癌 0 6 注:a为采用Fisher精确检验。 -
[1] 杨暄, 李定国, 孔莉. 内镜黏膜下剥离术治疗早期胃癌及癌前病变的疗效观察[J]. 海南医学, 2019, 30(9): 1127-1129.YANG X, LI D G, KONG L. Clinical effect of endoscopic submucosal dissection in early gastric carcinoma and precancerous lesion[J]. Hainan Medical Journal, 2019, 30(9): 1127-1129. [2] TAKIZAWA K, ONO H, HASUIKE N, et al. A nonrandomized, single-arm confirmatory trial of expanded endoscopic submucosal dissection indication for undifferentiated early gastric cancer: Japan Clinical Oncology Group study (JCOG1009/1010)[J]. Gastric Cancer, 2021, 24(2): 479-491. doi: 10.1007/s10120-020-01134-9 [3] 陈伟, 黄慧峰, 夏态军, 等. 消化道内镜诊治早期癌前病变62例回顾性分析[J]. 中华全科医学, 2017, 15(11): 1888-1890. doi: 10.16766/j.cnki.issn.1674-4152.2017.11.020CHEN W, HUANG H F, XIA T J, et al. Retrospective analysis of 62 cases of early precancerous lesions by diagnostic and therapeutic gastrointestinal endoscopies[J]. Chinese Journal of General Practice, 2017, 15(11): 1888-1890. doi: 10.16766/j.cnki.issn.1674-4152.2017.11.020 [4] COSTA L C D S, SANTOS J O M, MIYAJIMA N T, et al. Efficacy analysis of endoscopic submucosal dissection for the early gastric cancer and precancerous lesions[J]. Arq Gastroenterol, 2022, 59(3): 421-427. doi: 10.1590/s0004-2803.20220300075 [5] BOURKE M J, NEUHAUS H, BERGMAN J J. Endoscopic submucosal dissection: indications and application in western endoscopy practice[J]. Gastroenterology, 2018, 154(7): 1887-1900.e1885. DOI: 10.1053/j.gastro.2018.01.068. [6] 孙运军, 刘松, 李强. 内镜黏膜下剥离术治疗早期胃癌及癌前病变疗效及出血危险因素分析[J]. 中华肿瘤防治杂志, 2018, 25(9): 647-651. https://www.cnki.com.cn/Article/CJFDTOTAL-QLZL201809008.htmSUN Y J, LIU S, LI Q. Curative effect and bleeding risk factors of endoscopic submucosal dissection in the treatment of early gastric cancer and precancerous lesions[J]. Chinese Journal of Cancer Prevention and Treatment, 2018, 25(9): 647-651. https://www.cnki.com.cn/Article/CJFDTOTAL-QLZL201809008.htm [7] AHMED Y, OTHMAN M. EMR/ESD: techniques, complications, and evidence[J]. Curr Gastroenterol Rep, 2020, 22(8): 39. doi: 10.1007/s11894-020-00777-z [8] MANTA R, GALLORO G, PUGLIESE F, et al. Endoscopic submucosal dissection of gastric neoplastic lesions: an Italian, multicenter study[J]. J Clin Med, 2020, 9(3): 737. doi: 10.3390/jcm9030737 [9] MA X Q, ZHANG Q, ZHU S T, et al. Risk factors and prediction model for non-curative resection of early gastric cancer with endoscopic resection and the evaluation[J]. Front Med (Lausanne), 2021, 8: 637875. DOI: 10.3389/fmed.2021.637875. [10] YOUNG E, PHILPOTT H, SINGH R. Endoscopic diagnosis and treatment of gastric dysplasia and early cancer: current evidence and what the future may hold[J]. World J Gastroenterol, 2021, 27(31): 5126-5151. doi: 10.3748/wjg.v27.i31.5126 [11] 公宇, 张月明, 朱继庆, 等. 内镜黏膜下剥离术治疗早期胃癌及癌前病变发生迟发性出血的相关因素分析[J]. 中华肿瘤杂志, 2021, 43(8): 861-865.GONG Y, ZHANG Y M, ZHU J Q, et al. Analysis of risk factors for delayed bleeding after endoscopic submucosal dissection of gastric epithelial neoplasm[J]. Chinese Journal of Oncology, 2021, 43(8): 861-865. [12] KUMAR S, YOUN Y H, LEE J H. Life on a knife edge: the optimal approach to the management of perforations during endoscopic submucosal dissection (ESD)[J]. Expert Rev Gastroenterol Hepatol, 2020, 14(10): 965-973. doi: 10.1080/17474124.2020.1791085 [13] LEE J H, KEDIA P, STAVROPOULOS S N, et al. AGA clinical practice update on endoscopic management of perforations in gastrointestinal tract: expert review[J]. Clin Gastroenterol Hepatol, 2021, 19(11): 2252-2261. doi: 10.1016/j.cgh.2021.06.045 [14] RYU D G, CHOI C W, KANG D H, et al. Clinical outcomes of endoscopic submucosa dissection for high-grade dysplasia from endoscopic forceps biopsy[J]. Gastric Cancer, 2017, 20(4): 671-678. [15] MA M X, BOURKE M J. Endoscopic submucosal dissection in the West: current status and future directions[J]. Dig Endosc, 2018, 30(3): 310-320. [16] 张庆瑞, 张月明, 薛丽燕, 等. 内镜黏膜下剥离术治疗早期胃癌的疗效分析[J]. 中华肿瘤杂志, 2020, 42(9): 752-757. https://www.cnki.com.cn/Article/CJFDTOTAL-SYQY202310006.htmZHANG Q R, ZHANG Y M, XUE L Y, et al. Efficacy analysis of endoscopic submucosal dissection in the treatment of early gastric cancer[J]. Chinese Journal of Oncology, 2020, 42(9): 752-757. https://www.cnki.com.cn/Article/CJFDTOTAL-SYQY202310006.htm -





 下载:
下载: