Association of serum MCP-1 levels with vasculitis: A meta-analysis
-
摘要:
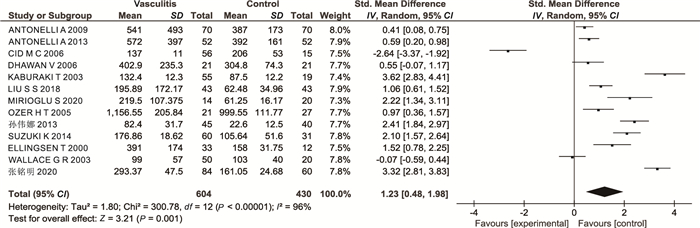
目的 单核细胞趋化蛋白1(monocyte chemotactic protein 1, MCP-1)是一种促炎趋化因子,参与血管炎的发病过程。本文系统评价血清MCP-1与血管炎的相关性,为评估MCP-1对血管炎诊断的临床价值提供依据。 方法 本研究利用Web of Science、PubMed、万方和CNKI数据库(截至2020年7月1日)对关于MCP-1与血管炎的相关研究进行检索。由2名研究人员根据纳入、排除标准筛查文献,提取有效数据;然后采用Review Manager(5.4.0版)软件和Stata 12.0统计学软件进行数据分析。 结果 最终纳入13项血清MCP-1和血管炎的研究(共1 034例患者)。血管炎组MCP-1水平高于健康对照组(SMD=1.23,95% CI:0.48~1.98,P=0.001)。血管炎亚组分析表明,小血管炎患者血清MCP-1水平显著高于健康对照组,而大血管炎和白塞病患者与健康人群血清MCP-1之间的差异无统计学意义。 结论 Meta分析表明,血管炎尤其是小血管炎患者血清MCP-1水平明显高于健康对照人群, 提示该指标对血管炎诊断有一定的临床价值。 -
关键词:
- 单核细胞趋化蛋白-1 /
- 血管炎 /
- Meta分析
Abstract:Objective Monocyte chemotactic protein 1 (MCP-1) is a proinflammatory chemokine that is involved in the pathogenesis of vasculitis. The purpose of this meta-analysis is to determine the relationship between serum MCP-1 levels with vasculitis. Methods Articles were identified by searching Web of Science, PubMed, Wanfang, and CNKI databases (up to July 1, 2020). Two independent evaluators screened literature according to inclusion and exclusion criteria, extracted relevant data, and then used Review Manager software (version 5.4.0) and Stata 12.0 software for meta-analysis. Results A total of 13 original articles of vasculitis (1 034 participants) were finally included. The vasculitis group had a higher level of MCP-1 than healthy control (SMD=1.23, 95% CI: 0.48-1.98, P=0.001). Subgroup analysis based on the classification of vasculitis indicated that the serum MCP-1 levels in small vessel vasculitis patients were significantly higher compared to healthy controls, but not in large vessel vasculitis and Behcet ' s disease patients. Conclusion Meta-analysis shows that serum MCP-1 level is significantly higher in patients with vasculitis, especially small vessel vasculitis, than in healthy controls. It suggests that this index has some clinical value for the diagnosis of vasculitis. -
Key words:
- Monocyte chemotactic protein 1 /
- Vasculitis /
- Meta-analysis
-
表 1 纳入文献的基本信息
Table 1. Basic information on the literature included
第一作者 出版时间 国家 疾病 组别(例) 年龄(岁) 性别(男性/女性,例) 血管炎 健康对照 血管炎 健康对照 血管炎 健康对照 张铭明[10] 2020 China AAV 84 60 67.64±12.23 46.86±13.23 33/51 19/41 MIRIOGLU S[11] 2020 Turkey AAV 14 20 61.00±6.25 28.00±2.88 7/7 5/15 LIU S S[5] 2018 China SV 43 43 38.88±9.89 41.44±13.57 25/18 18/25 SUZUKI K[12] 2014 Japan AAV 60 31 67.07±12.21 69.19±15.01 9/51 15/16 孙伟娜[17] 2013 China SV 45 40 18~75 20~70 21/24 16/24 ANTONELLI A[15] 2013 Italy CV 52 52 62.00±9.00 62.00±9.00 15/37 15/37 ANTONELLI A[16] 2009 Italy CV 70 70 60.00±11.00 60.00±11.00 13/57 13/57 CID M C[8] 2006 Spain GCA 56 18 - - 16/40 matched DHAWAN V[18] 2006 India TA 21 21 26.00±12.00 28.00±10.00 5/16 7/14 OZER H T[13] 2005 Turkey BD 21 27 38.95±1.60 37.00±6.60 11/10 14/13 KABURAKI T[14] 2003 Japan BD 55 19 40.60±10.60 40.50±12.60 48/7 16/3 WALLACE G R[19] 2003 England RV 50 20 - - - - ELLINGSEN T[9] 2000 Denmark GCA 33 12 71.40±7.75 43.00±6.50 8/25 6/6 注: AAV为抗中性粒细胞质抗体相关性血管炎; BD为白塞病;CV为冷球蛋白血症性血管炎;GCA为巨细胞动脉炎; GPA为肉芽肿性多血管炎;MPA为显微镜下多血管炎;TA为大动脉炎;RV为视网膜血管炎;SV为系统性血管炎;“-”为未提供。 表 2 纳入研究的质量评价和单核细胞趋化因子1水平
Table 2. Quality assessment of included studies and levels of monocyte chemokine 1
第一作者 血管炎组(x±s,pg/mL) 健康对照组(x±s,pg/mL) 诊断标准 检测方法 NOS(分) 张铭明[10] 293.37±47.50 161.05±24.68 CHCC ELISA 8 MIRIOGLU S[11] 219.50±107.37 61.25±16.17 2012CHCC ELISA 7 LIU S S[5] 195.89±140.07 62.48±39.09 ACR/CHCC ELISA 8 SUZUKI K[12] 176.86±18.62 105.64±51.60 ACR multiplex assay 7 孙伟娜[17] 82.40±31.70 22.60±12.50 ACR FCM 7 ANTONELLI A[15] 572.00±397.00 392.00±161.00 Symptoms+lab tests ELISA 7 ANTONELLI A[16] 541.00±493.00 387.00±173.00 Symptoms+lab tests ELISA 7 CID M C[8] 137.00±11.00 206.00±53.00 ACR ELISA 6 DHAWAN V[18] 402.90±253.30 304.80±74.30 Ishikawa's criteria ELISA 7 OZER H T[13] 1 156.55±205.84 999.55±111.77 Symptoms+lab tests ELISA 6 KABURAKI T[14] 132.40±12.30 87.50±12.20 Symptoms+lab tests ELISA 6 WALLACE G R[19] 99.00±37.00 103.00±40.00 Symptoms+lab tests ELISA 6 ELLINGSEN T[9] 391.00±174.00 158.00±31.75 Symptoms and biopsy ELISA 7 注: CHCC为教堂山会议;ACR为美国风湿病学会;FCM为流式细胞术;NOS为纽卡斯尔-渥太华质量评估量表。 -
[1] FELICETTI M, TREPPO E, POSARELLI C, et al. One year in review 2020: vasculitis[J]. Clin Exp Rheumatol, 2020, 124(2): 3-14. [2] 侯传云, 李志军. 系统性血管炎的诊断与治疗[J]. 中华全科医学, 2020, 18(5): 710-711. http://www.zhqkyx.net/article/id/450159ed-8208-42b3-bea4-23f0ad841586HOU C Y, LI Z J. Diagnosis and treatment of systemic vasculitis[J]. Chinese Journal of General Practice, 2020, 18(5): 710-711. http://www.zhqkyx.net/article/id/450159ed-8208-42b3-bea4-23f0ad841586 [3] ZHU Q, LIU S S, HEIZHATI M, et al. Systemic vasculitis: an important and underestimated cause of malignant hypertension[J]. Cardiovasc Innov Appl, 2019, 4(2): 99-108. [4] JENNETTE J C, FALK R J, BACON P A, et al. 2012 revised international chapel hill consensus conference nomenclature of vasculitides[J]. Arthritis Rheum, 2013, 65(1): 1-11. doi: 10.1002/art.37715 [5] LIU S S, LI N F, ZHU Q, et al. Increased serum MCP-1 levels in systemic vasculitis patients with renal involvement[J]. J Interferon Cytokine Res, 2018, 38(9): 406-412. doi: 10.1089/jir.2017.0140 [6] DESHMANE S L, KREMLEV S, AMINI S, et al. Monocyte chemoattractant protein-1 (MCP-1): an overview[J]. J Interferon Cytokine Res, 2009, 29(6): 313-326. doi: 10.1089/jir.2008.0027 [7] HALLER H, BERTRAM A, NADROWITZ F, et al. Monocyte chemoattractant protein-1 and the kidney[J]. Curr Opin Nephrol Hypertens, 2016, 25(1): 42-49. doi: 10.1097/MNH.0000000000000186 [8] CID M C, HOFFMAN M P, HERNÁNDEZ-RODRÍGUEZ J, et al. Association between increased CCL2 (MCP-1) expression in lesions and persistence of disease activity in giant-cell arteritis[J]. Rheumatology (Oxford), 2006, 45(11): 1356-1363. doi: 10.1093/rheumatology/kel128 [9] ELLINGSEN T, ELLING P, OLSON A, et al. Monocyte chemoattractant protein 1 (MCP-1) in temporal arteritis and polymyalgia rheumatica[J]. Ann Rheum Dis, 2000, 59(10): 775-780. doi: 10.1136/ard.59.10.775 [10] 张铭明, 张锐, 杨小珂, 等. 抗中性粒细胞胞浆抗体相关性血管炎患者中MIF及MCP-1的检测及临床意义[J]. 国际检验医学杂志, 2020, 41(13): 1581-1584. doi: 10.3969/j.issn.1673-4130.2020.13.011ZHANG M M, ZHANG R, YANG X K, et al. The study of MIF and MCP-1 in patients with anti-neutrophil cytoplasmic antibody associated vasculitis[J]. International Journal of Laboratory Medicine, 2020, 41(13): 1581-1584. doi: 10.3969/j.issn.1673-4130.2020.13.011 [11] MIRIOGLU S, CINAR S, YAZICI H, et al. Serum and urine TNF-like weak inducer of apoptosis, monocyte chemoattractant protein-1 and neutrophil gelatinase-associated lipocalin as biomarkers of disease activity in patients with systemic lupus erythematosus[J]. Lupus, 2020, 29(4): 379-388. doi: 10.1177/0961203320904997 [12] SUZUKI K, NAGAO T, ITABASHI M, et al. A novel autoantibody against moesin in the serum of patients with MPO-ANCA-associated vasculitis[J]. Nephrol Dial Transplant, 2014, 29(6): 1168-1177. doi: 10.1093/ndt/gft469 [13] OZER H T, ERKEN E, GUNESACAR R, et al. Serum RANTES, MIP-1alpha, and MCP-1 levels in Behet ' s disease[J]. Rheumatol Int, 2005, 25(6): 487-488. doi: 10.1007/s00296-004-0519-0 [14] KABURAKI T, FUJINO Y, KAWASHIMA H, et al. Plasma and whole-blood chemokine levels in patients with Behcet ' s disease[J]. Graefes Arch Clin Exp Ophthalmol, 2003, 241(5): 353-358. doi: 10.1007/s00417-003-0668-y [15] ANTONELLI A, FALLAHI P, FERRARI S M, et al. Parallel increase of circulating CXCL11 and CXCL10 in mixed cryoglobulinemia, while the proinflammatory cytokine IL-6 is associated with high serum Th2 chemokine CCL2[J]. Clin Rheumatol, 2013, 32(8): 1147-1154. doi: 10.1007/s10067-013-2246-y [16] ANTONELLI A, FERRI C, FALLAHI P, et al. CXCL10 and CCL2 serum levels in patients with mixed cryoglobulinaemia and hepatitis C[J]. Dig Liver Dis, 2009, 41(1): 42-48. doi: 10.1016/j.dld.2008.04.009 [17] 孙伟娜, 陈院朝, 蔡文杰. 45例系统性血管炎患者炎症性因子检测结果分析[J]. 中外健康文摘, 2013, 10(28): 158.SUN W N, CHEN Y C, CAI W J. Analysis of inflammatory factors in 45 patients with systemic vasculitis[J]. World Health Digest Medical Periodieal, 2013, 10(28): 158. [18] DHAWAN V, MAHAJAN N, JAIN S. Role of C-C chemokines in Takayasu ' s arteritis disease[J]. Int J Cardiol, 2006, 112(1): 105-111. doi: 10.1016/j.ijcard.2005.11.101 [19] WALLACE G R, FARMER I, CHURCH A, et al. Serum levels of chemokines correlate with disease activity in patients with retinal vasculitis[J]. Immunol Lett, 2003, 90(1): 59-64. doi: 10.1016/S0165-2478(03)00159-7 [20] 朱晴, 朱彬, 吴婷, 等. 高迁移率族蛋白水平与系统性血管炎相关性的Meta分析[J]. 中华全科医学, 2021, 19(1): 131-136. doi: 10.16766/j.cnki.issn.1674-4152.001749ZHU Q, ZHU B, WU T, et al. Meta-analysis of the relationship between HMGB1 level and systemic vasculitis[J]. Chinese Journal of General Practice, 2021, 19(1): 131-136. doi: 10.16766/j.cnki.issn.1674-4152.001749 [21] NORRIS J M, SIMPSON B S, BALLR, et al. A modified Newcastle-Ottawa scale for assessment of study quality in genetic urological research[J]. Eur Urol, 2021, 79(3): 325-326. [22] SUGIYAMA M, WADA Y, KANAZAWA N, et al. A cross-sectional analysis of clinicopathologic similarities and differences between Henoch-Schönlein purpura nephritis and IgA nephropathy[J]. PLoS One, 2020, 15(4): e0232194. DOI: 10.1371/journal.pone.0232194. [23] TAM F W, SANDERS J S, GEORGE A, et al. Urinary monocyte chemoattractant protein-1 (MCP-1) is a marker of active renal vasculitis[J]. Nephrol Dial Transplant, 2004, 19(11): 2761-2768. [24] MORAN S M, MONACH P A, ZGAGA L, et al. Urinary soluble CD163 and monocyte chemoattractant protein-1 in the identification of subtle renal flare in anti-neutrophil cytoplasmic antibody-associated vasculitis[J]. Nephrol Dial Transplant, 2020, 35(2): 283-291. -





 下载:
下载: