Establishment and validation of model for the risk of Carbapenem-Resistant Enterobacteriaceae infection in elderly patients with pulmonary infection
-
摘要:
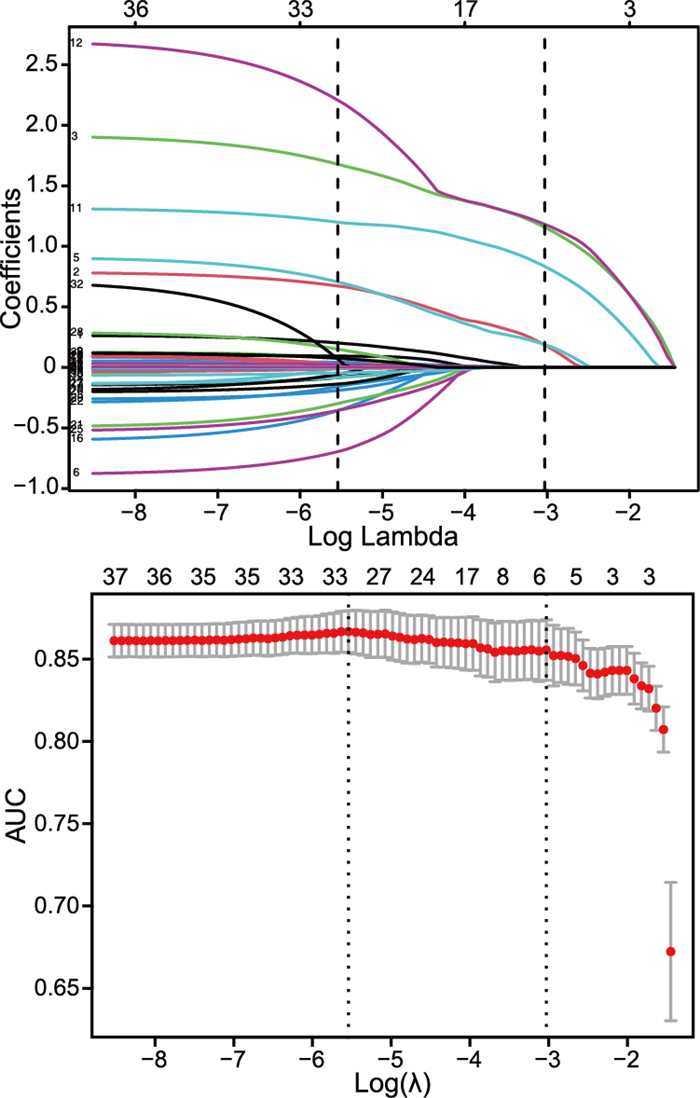
目的 分析及筛选影响老年肺部耐碳青霉烯肠杆菌(CRE)感染的高危因素,构建并验证风险Nomogram预测模型。 方法 回顾性对安徽地区共894例的老年(≥60岁)肺部感染痰培养为肠杆菌科细菌的住院患者的临床资料进行收集,抽取2个医院作为验证组(250例),其余作为建模组(644例),使用单因素Lasso回归和多变量logistic回归分析对建模组数据进行分析,确定CRE感染的独立危险因素。构建Nomogram预测模型, 并对模型进行多中心验证。 结果 气管插管≥72 h、长期卧床、抗生素使用种类≥2种、脑血管疾病、营养不良是老年肺部耐碳青霉烯肠杆菌感染的独立危险因素。基于上述5项独立危险因素,建立预测风险Nomogram模型,建模组和验证组2组AUC值分别为0.862、0.858;且Hosmer-Lemeshow检验可见建模组P=0.761,验证组P=0.339;Decision曲线分析显示,模型在较大的阈值内获益性均良好。 结论 构建老年肺部CRE感染风险预测模型具有一定的临床意义,能够针对可控因素进行早期个体化干预。 Abstract:Objective To analyze and screen the high-risk factors for CRE infection in elderly people with pulmonary infection, and to construction and validate a risk nomogram prediction model. Methods Clinical data of a total of 894 elderly (≥60 years old) hospitalized patients with pulmonary infection cultured by Enterobacteriaceae bacteria in Anhui Province were retrospectively collected. Two hospitals were selected as verification group (250 cases), and the rest were used as training group(644 cases). Univariate Lasso regression and multivariate logistic regression analysis were used to analyze the modeling group data to identify independent risk factors for CRE infection. Construct a Nomogram prediction model and verify the model in multiple centers. Results The independent risk factors of CRE infection in the elderly were endotracheal intubation≥72 h, long-term bed rest, ≥2 types of antibiotics, cerebrovascular disease and malnutrition. Based on the above five independent risk factors, a Nomogram model for predicting risk was established, and the AUC values of the training group and verification group were 0.862 and 0.858. The Hosmer-Lemeshow test shows that the training group P=0.761 and the verification group P=0.339. Decision curve analysis shows that the model has good benefit within large thresholds. Conclusion The construction of a risk prediction model for the risk of CRE infection in the lungs of elderly people have some clinical significance, allowing early individualized intervention according to controllable factors. -
表 1 建模组及验证组老年肺部感染患者一般临床特征比较
Table 1. Comparison of general clinical characteristics of elderly patients with pulmonary infection between the modeling group and the verification group
项目 建模组(n=644) 验证组(n=250) 统计量 P值 年龄(x±s,岁) 80.9±8.0 76.7±9.0 6.698a <0.001 性别(男性/女性,例) 442/202 157/93 1.541b 0.215 吸烟史[例(%)] 67(10.4) 50(20.0) 2.602b 0.107 药物过敏史[例(%)] 31(4.8) 34(13.6) 1.754b 0.185 手术史[例(%)] 356(55.3) 126(50.4) 0.157b 0.692 既往住院史[例(%)] 512(79.5) 166(66.4) 0.779b 0.377 长期卧床[例(%)] 263(40.8) 118(47.2) 3.455b 0.063 合并症[例(%)] 其他部位感染 228(35.4) 80(32.0) 1.722b 0.188 心力衰竭 136(21.1) 48(19.2) 0.021b 0.884 休克 112(17.4) 14(5.6) 2.893b 0.089 重症肺炎 193(29.9) 79(31.6) 1.885b 0.170 呼吸衰竭 160(24.8) 56(22.4) 1.270b 0.260 基础疾病[例(%)] 慢性阻塞性肺疾病 102(15.8) 49(19.6) 0.124b 0.725 慢性肺源性心脏病 37(5.7) 15(6.0) 0.270b 0.603 冠心病 156(24.2) 74(29.6) 0.007b 0.935 糖尿病 171(26.6) 64(25.6) 2.806b 0.094 高血压 376(58.4) 134(53.6) 0.029b 0.865 消化道出血 40(6.2) 16(6.4) 0.373b 0.541 肿瘤 179(27.8) 68(27.2) 2.064b 0.151 动脉硬化 232(36.0) 87(34.8) 0.439b 0.507 脑血管疾病 413(64.1) 145(58.0) 0.001b 0.979 治疗相关因素[例(%)] 抗生素使用时长≥2周 190(29.5) 102(40.8) 2.941b 0.086 抗生素使用种类≥2种 246(38.2) 113(45.2) 0.790b 0.374 住院时长[M(P25, P75),d] 15.66(12.00,18.00) 16.06(14.00,18.00) -1.010c 0.313 治疗中吸痰[例(%)] 483(75.0) 173(69.2) 0.250b 0.617 有创操作[例(%)] 气管插管≥72 h 106(16.9) 61(24.4) 3.262b 0.071 留置胃管 473(73.4) 159(63.6) 0.419b 0.518 留置导尿管 331(51.4) 111(44.4) 0.674b 0.412 老年综合征[例(%)] 痴呆 183(28.4) 46(18.4) 3.808b 0.051 营养不良 197(30.6) 80(32.0) 3.371b 0.066 实验室检查指标[M(P25, P75)] 白细胞计数(×109/L) 10.3(6.7, 12.3) 12.3(6.1, 11.7) -1.860c 0.063 中性粒百分比(%) 77.8(69.3, 88.0) 77.0(68.1, 87.9) -0.586c 0.558 红细胞计数(×109/L) 3.8(3.3, 4.3) 3.8(3.3, 4.3) -0.537c 0.591 血红蛋白(g/L) 112.2(97.0, 128.0) 114.4(99.0, 131.0) -1.671c 0.095 ALT(μ/L) 32.2(11.3, 31.7) 29.3(11.0, 29.3) -0.588c 0.556 AST(μ/L) 45.4(17.0, 38.5) 43.3(16.0, 35.0) -1.815c 0.069 肌酐(μmol/L) 102.2(53.1, 99.7) 93.3(51.8, 97.0) -0.842c 0.400 尿素(mmol/L) 10.5(5.0, 10.7) 7.7(4.6, 9.0) -2.565c 0.010 白蛋白(g/L) 35.1(33.0, 38.3) 34.8(31.2, 38.3) -1.825c 0.068 注:a为t值,b为χ2值,c为Z值。其他部位感染包括血液、尿液、引流液、腹腔等;抗生素使用时长≥2周指不同抗生素总使用疗程≥2周;抗生素使用种类包括所有针对阴性菌及阳性菌的抗生素。 表 2 CRE组和CSE组老年肺部感染患者菌株类型分布情况[例(%)]
Table 2. Distribution of bacterial strains in elderly patients with pulmonary infection between CRE group and CSE group [cases(%)]
组别 例数 肺炎克雷伯菌 阴沟肠杆菌 大肠埃希菌 其他a CRE组 404 262(64.9) 29(7.2) 52(12.8) 61(15.1) CSE组 490 311(63.5) 41(8.4) 97(19.8) 41(8.3) 注:a包括弗劳地枸橼酸杆菌、产气克雷伯菌、产酸克雷伯菌、变栖克雷伯菌、粘质沙雷菌等。 表 3 老年肺部感染患者CRE感染的多因素logistic回归分析
Table 3. Multivariate logistic regression analysis of CRE infection in elderly patients with pulmonary infection
项目 B SE Wald χ2 P值 OR值(95%CI) 气管插管≥72 h 0.701 0.336 4.353 0.037 2.015(1.043~3.891) 长期卧床 1.598 0.213 56.176 <0.001 4.945(3.256~7.511) 抗生素使用种类≥2种 0.451 0.223 4.085 0.043 1.569(1.014~2.429) 脑血管疾病 1.282 0.231 30.656 <0.001 3.603(2.289~5.671) 营养不良 1.558 0.252 38.144 <0.001 4.747(2.896~7.783) -
[1] CHERAK Z, LOUCIF L, MOUSSI A, et al. Carbapenemase-producing Gram-negative bacteria in aquatic environments: a review[J]. J Glob Antimicrob Resist, 2021, 25: 287-309. doi: 10.1016/j.jgar.2021.03.024 [2] 池水晶, 封燚, 李慧, 等. 多重耐药菌感染术后肺炎相关危险因素分析及控制方法学探究[J]. 中华全科医学, 2021, 19(4): 671-673, 701. doi: 10.16766/j.cnki.issn.1674-4152.001890CHI S J, FENG Y, LI H, et al. Analysis of risk factors related to pneumonia after multidrug-resistant bacterial infection and exploration of control methodology[J]. Chinese Journal of General Practice, 2021, 19(4): 671-673, 701. doi: 10.16766/j.cnki.issn.1674-4152.001890 [3] LUTGRING J D. Carbapenem-resistant Enterobacteriaceae: an emerging bacterial threat[J]. Semin Diagn Pathol, 2019, 36(3): 182-186. doi: 10.1053/j.semdp.2019.04.011 [4] HUMPHRIES R, BOBENCHIK A M, HINDLER J A, et al. Overview of changes to the clinical and laboratory standards institute performance standards for antimicrobial susceptibility testing, M100, 31st edition[J]. J Clin Microbiol,2021,59(12):e0021321.DOI: 10.1128/JCM.00213-21.DOI:10.1128/JCM.00213-21. [5] 冯贺强, 何丽洁, 张彩红, 等. 老年耐碳青霉烯类肠杆菌科细菌感染特点与影响因素分析[J]. 中华医院感染学杂志, 2019, 29(11): 1609-1613.FENG H Q, HE L J, ZHANG C H, et al. Characteristics and risk factors of carbapenem-resistant Eenterobacteriaceae infection in elderly patients[J]. Chinese Journal of Nosocomiology, 2019, 29(11): 1609-1613. [6] 陈亚男, 刘菁, 李爱民, 等. 304例耐碳青霉烯类肠杆菌科细菌医院感染流行病学特征与干预措施及效果[J]. 中华医院感染学杂志, 2022, 32(10): 1450-1453.CHEN Y N, LIU J, LI A M, et al. Epidemiological characteristics of nosocomial infection of 304 cases caused by carbapenem-resistant Enterobacteriaceae and effect of intervention measures[J]. Chinese Journal of Nosocomiology, 2022, 32(10): 1450-1453. [7] BUTLER M S, GIGANTE V, SATI H, et al. Analysis of the clinical pipeline of treatments for drug-resistant bacterial infections: despite progress, more action is needed[J]. Antimicrob Agents Chemother, 2022, 66(3): e0199121. DOI: 10.1128/AAC.01991-21. [8] 中华人民共和国卫生部. 医院感染诊断标准(试行)[J]. 中华医学杂志, 2001, 81(5): 314-320. doi: 10.3760/j:issn:0376-2491.2001.05.027Ministry of Health of the People's Republic of China. Diagnostic criteria for Nosocomial infection (Trial)[J]. National Medical Journal of China, 2001, 81(5): 314-320. doi: 10.3760/j:issn:0376-2491.2001.05.027 [9] YANG S, XU H, SUN J, et al. Shifting trends and age distribution of ESKAPEEc resistance in bloodstream infection, Southwest China, 2012-2017[J]. Antimicrob Resist Infect Control, 2019, 8: 61. DOI: 10.1186/s13756-019-0499-1. [10] 赵建兰, 许东风, 赵静, 等. 老年肺部感染住院患者多药耐药菌感染影响因素的回顾性调查[J]. 中华医院感染学杂志, 2019, 29(6): 835-838.ZHAO J L, XU D F, ZHAO J, et al. Retrospective survey of influencing factors for multidrug-resistant organisms infections in elderly hospitalized patients with pulmonary infections[J]. Chinese Journal of Nosocomiology, 2019, 29(6): 835-838. [11] CHARANI E, MCKEE M, BALASEGARAM M, et al. Global burden of antimicrobial resistance: essential pieces of a global puzzle[J]. Lancet, 2022, 399(10344): 2346-2347. doi: 10.1016/S0140-6736(22)00935-7 [12] ZHANG Y, WANG Q, YIN Y, et al. Epidemiology of carbapenem-resistant enterobacteriaceae infections: report from the China CRE network[J]. Antimicrob Agents Chemother, 2018, 62(2): e01882-17. DOI: 10.1128/AAC.01882-17. [13] 张安汝, 王启, 周朝娥, 等. 碳青霉烯类耐药肠杆菌目细菌院内感染危险因素和临床预后分析[J]. 中华医学杂志, 2021, 101(21): 1572-1582. doi: 10.3760/cma.j.cn112137-20201224-03455ZHANG A R, WANG Q, ZHOU Z E, et al. Risk factors and clinical prognosis analysis of carbapenem-resistant Enterobacterales bacteria nosocomial infection[J]. National Medical Journal of China, 2021, 101(21): 1572-1582. doi: 10.3760/cma.j.cn112137-20201224-03455 [14] 陈慧玲, 张媛, 徐敏, 等. 医养结合机构老年坠积性肺炎患者多重耐药菌分布及感染的危险因素[J]. 中国老年学杂志, 2020, 40(16): 3425-3427. doi: 10.3969/j.issn.1005-9202.2020.16.021CHEN H L, ZHANG Y, XU M, et al. Distribution of multi-drug resistant bacteria and risk factors of infection in elderly patients with hypostatic pneumonia in hospitals and nursing institutions[J]. Chinese Journal of Gerontology, 2020, 40(16): 3425-3427. doi: 10.3969/j.issn.1005-9202.2020.16.021 [15] 谯瞧, 宋平义, 官彬, 等. 气管插管全身麻醉行腹部手术老年患者肺部感染的危险因素及预测模型构建[J]. 重庆医学, 2022, 51(7): 1167-1171, 1176. doi: 10.3969/j.issn.1671-8348.2022.07.017QIAO Q, SONG P Y, GUAN B, et al. Risk factors and predictive modeling of pulmonary infection in elderly patients undergoing abdominal surgery with tracheal intubation and general anesthesia[J]. Chongqing Medicine, 2022, 51(7): 1167-1171, 1176. doi: 10.3969/j.issn.1671-8348.2022.07.017 [16] 谢朝云, 陈应强, 熊芸, 等. 老年肺结核合并肺部多重耐药菌感染危险因素[J]. 中国老年学杂志, 2019, 39(20): 4977-4980. doi: 10.3969/j.issn.1005-9202.2019.20.031XIE C Y, CHEN Y Q, XIONG Y, et al. Risk factors of pulmonary tuberculosis in the elderly with multidrug-resistant bacteria infection[J]. Chinese Journal of Gerontology, 2019, 39(20): 4977-4980. doi: 10.3969/j.issn.1005-9202.2019.20.031 [17] AGARWAL N, AGARWAL S K, BHATTACHARYA S, et al. Antibiotic prophylaxis for breast oncosurgery in a setting with a high prevalence of multidrug-resistant bacteria: common sense infection control measures are more important than prolonged antibiotics[J]. Infect Control Hosp Epidemiol, 2018, 39(4): 498-500. doi: 10.1017/ice.2017.313 [18] 庞天义, 满德强, 常群. 老年肺部感染住院患者合并多重耐药菌感染的危险因素探讨及风险Nomogram模型的建立[J]. 中国抗生素杂志, 2021, 46(12): 1157-1161. doi: 10.3969/j.issn.1001-8689.2021.12.015PANG T Y, MAN D Q, CHANG Q, et al. Study on the risk factors of multidrug-resistant bacteria infection and the establishment of risk Nomogram model in elderly patients with pulmonary infection[J]. Chinese Journal of Antibiotics, 2021, 46(12): 1157-1161. doi: 10.3969/j.issn.1001-8689.2021.12.015 [19] MIYASHITA K, NAKATANI E, HOZUMI H, et al. Risk factors for pneumonia and death in adult patients with seasonal influenza and establishment of prediction scores: a population-based study[J]. Open Forum Infect Dis, 2021, 8(3): ofab068. DOI: 10.1093/ofid/ofab068. [20] LIU Y X, CAO Q M, MA B C. Pathogens distribution and drug resistance in patients with acute cerebral infarction complicated with diabetes and nosocomial pulmonary infection[J]. BMC Infect Dis, 2019, 19(1): 603. doi: 10.1186/s12879-019-4142-9 [21] 孙明秀, 左东辉, 吴宇欣. 脑梗死患者合并肺部感染的危险因素及预防措施[J]. 湖南师范大学学报(医学版), 2020, 17(5): 87-89.SUN M X, ZUO D H, WU Y X. Risk factors and preventive measures for pulmonary infection in patients with cerebral infarction[J]. Journal of Hunan Normal University(Medical Sciences), 2020, 17(5): 87-89. -





 下载:
下载: