Application of the FRQ and MFS in assessing the fall risk in postmenopausal osteoporosis
-
摘要:
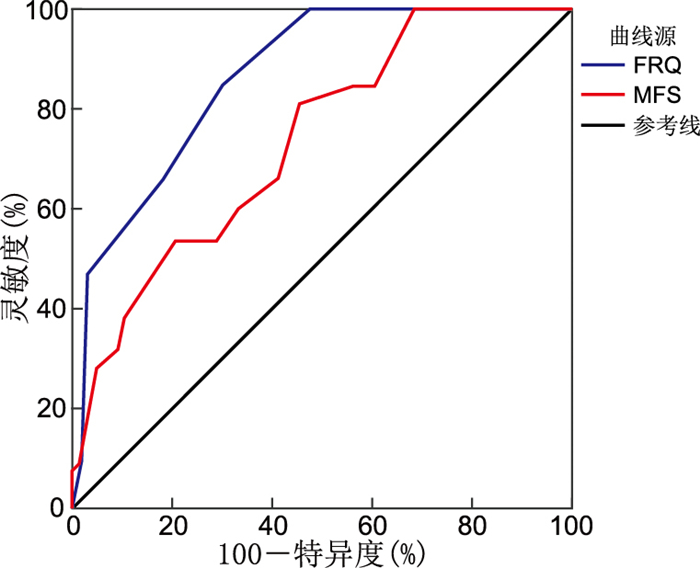
目的 比较跌倒风险自评表(FRQ)与Morse跌倒评估量表(MFS)在绝经后骨质疏松症(PMOP)人群中的应用价值,为该人群跌倒风险评估工具的选择提供参考。 方法 采用便利抽样法纳入2020年9月—2022年1月于蚌埠医科大学第一附属医院体检或就诊的193例PMOP患者作为研究对象,使用FRQ和MFS进行跌倒风险评估。根据随访期间是否跌倒分为跌倒组(32例)和未跌倒组(161例),通过ROC曲线、灵敏度、特异度及Bayes判别分析评价量表。 结果 跌倒组FRQ和MFS量表得分均高于未跌倒组,差异有统计学意义(P<0.001);FRQ、MFS的AUC分别为0.865和0.737,差异有统计学意义(P=0.003);FRQ、MFS临界值分别为4分和40分时,约登指数分别为0.546和0.360,此时灵敏度分别为0.844和0.813,特异度分别为0.702和0.547,阳性预测值、阴性预测值、阳性似然比、阴性似然比分别为0.360、0.958、2.830、0.223和0.263、0.936、1.792、0.343,交叉检验准确率分别为72.5%和60.6%。 结论 FRQ与MFS均能有效预测PMOP人群的跌倒风险。与MFS相比,FRQ预测价值更高。 -
关键词:
- 跌倒风险自评表 /
- Morse跌倒评估量表 /
- 绝经后骨质疏松症 /
- 跌倒风险评估
Abstract:Objective To compare the value of the self-rated fall risk questionnaire (FRQ) and the Morse fall scale (MFS) in assessing fall risk in postmenopausal osteoporosis (PMOP), and to inform the selection of fall risk assessment tools for this population. Methods A total of 193 postmenopausal women with a confirmed diagnosis of osteoporosis were selected from the First Affiliated Hospital of Bengbu Medical University from September 2020 to January 2022 by convenience sampling method, and were invited to attend a survey of their fall risk assessed by the FRQ and MFS and follow-up on falls. The group was divided into a fall group (n=32) and a non-fall group (n=161) according to whether they fell or not during the follow-up period, and the scale was evaluated by means of ROC curve, sensitivity, specificity and Bayes discriminant analysis. Results The scores of both scales in the fall group were higher than those in the non-fall group, and the difference was statistically significant (P<0.001); the AUC of the FRQ and MFS were 0.865 and 0.737, respectively, and the difference was statistically significant (P=0.003); the Youden ' s index was 0.546 and 0.360 at critical values of 4 and 40 for the FRQ and MFS, respectively, when the sensitivity was 0.844 and 0.813, and specificity was 0.702 and 0.547, respectively. The positive predictive value, negative predictive value, positive likelihood ratio and negative likelihood ratio were 0.360, 0.958, 2.830, 0.223 and 0.263, 0.936, 1.792, 0.343, respectively. The cross-check accuracy of the FRQ and MFS was 72.5% and 60.6%, respectively. Conclusion Both FRQ and MFS can effectively predict the risk of falls in postmenopausal osteoporosis, while, FRQ shows a higher predictive value compared to MFS. -
表 1 193例PMOP患者一般资料
Table 1. General data of 193 patients with postmenopausal osteoporosis (PMOP)
项目 类别 例数 构成比(%) 年龄(岁) <60 65 33.7 60~79 109 56.5 ≥80 19 9.8 自然绝经年龄(岁) ≤45 39 20.2 46~54 145 75.1 ≥55 9 4.7 绝经年限(年) ≤6 44 22.8 7~9 15 7.8 ≥10 134 69.4 BMI <18.5 13 6.7 18.5~23.9 105 54.5 24.0~27.9 63 32.6 ≥28.0 12 6.2 随访中跌倒次数(次) 0 161 83.4 ≥1 32 16.6 FRQ得分(分) 0~3 118 61.1 ≥4 75 38.9 MFS得分(分) 0~45 121 62.7 >45 72 37.3 表 2 2组PMOP患者FRQ和MFS评分比较[M(P25, P75),分]
Table 2. Comparison of FRQ and MFS scores in two groups of PMOP patients [M(P25, P75), points]
组别 例数 FRQ MFS 跌倒组 32 5(4, 6) 60(40, 75) 未跌倒组 161 2(1, 4) 35(15, 55) Z值 6.602 4.241 P值 <0.001 <0.001 表 3 最佳临界值下FRQ与MFS对PMOP患者跌倒风险的预测价值
Table 3. Predictive value of FRQ and MFS at optimal thresholds for fall risk in patients with postmenopausal osteoporosis
量表 灵敏度 特异度 阳性预测值 阴性预测值 阳性似然比 阴性似然比 FRQ 0.844 0.702 0.360 0.958 2.830 0.223 MFS 0.813 0.547 0.263 0.936 1.792 0.343 表 4 FRQ与MFS最佳临界值分组PMOP患者跌倒发生情况比较(例)
Table 4. Comparison of incidence of falls in pmop patients by optimal threshold grouping of FRQ and MFS (cases)
量表 类别 跌倒组 未跌倒组 总计 χ2值 P值 FRQ 跌倒高风险组1 27 48 75 33.447 <0.001 跌倒低风险组1 5 113 118 MFS 跌倒高风险组2 26 73 99 13.777 <0.001 跌倒低风险组2 6 88 94 表 5 FRQ与MFS的Bayes判别分析
Table 5. Bayesian discriminant analysis of FRQ and MFS
量表 Bayes判别方程 准确率(%) Y0(未跌倒组) Y1(跌倒组) FRQ Y0=-1.888+0.930X Y1=-5.558+1.875X 72.5 MFS Y0=-1.583+1.715X Y1=-2.328+2.326X 60.6 -
[1] AIBAR-ALMAZÁN A, VOLTES-MARTÍNEZ A, CASTELLOTE-CABALLERO Y, et al. Current status of the diagnosis and management of osteoporosis[J]. Int J Mol Sci, 2022, 23(16): 9465. DOI: 10.3390/ijms23169465. [2] SCHOBERER D, BREIMAIER H E, ZUSCHNEGG J, et al. Fall prevention in hospitals and nursing homes: clinical practice guideline[J]. Worldviews Evid Based Nurs, 2022, 19(2): 86-93. doi: 10.1111/wvn.12571 [3] KOMISAR V, ROBINOVITCH S N. The role of fall biomechanics in the cause and prevention of bone fractures in older adults[J]. Curr Osteoporos Rep, 2021, 19(4): 381-390. doi: 10.1007/s11914-021-00685-9 [4] DIEBO B G, STROUD S G, SHAH N V, et al. Can we predict imbalance in patients? Analysis of the CDC national health and nutrition examination survey[J]. J Clin Med, 2023, 12(5): 1943. DOI: 10.3390/jcm12051943. [5] North American Menopause Society. Management of osteoporosis in postmenopausal women: the 2021 position statement of The North American Menopause Society[J]. Menopause, 2021, 28(9): 973-997. doi: 10.1097/GME.0000000000001831 [6] 中华医学会妇产科学分会绝经学组. 中国绝经管理与绝经激素治疗指南2023版[J]. 中华妇产科杂志, 2023, 58(1): 4-21. doi: 10.3760/cma.j.cn112141-20221118-00706Menopause Subgroup, Chinese Society of Obstetrics and Gynecology, Chinese Medical Association. The 2023 Chinese menopause symptom management and menopausal hormone therapy guidelines[J]. Chinese Journal of Obstetrics and Gynecology, 2023, 58(1): 4-21. doi: 10.3760/cma.j.cn112141-20221118-00706 [7] KITCHARANANT N, VANITCHAROENKUL E, UNNANUNTANA A. Validity and reliability of the self-rated fall risk questionnaire in older adults with osteoporosis[J]. BMC Musculoskel Dis, 2020, 21(1): 757. DOI: 10.1186/s12891-020-03788-z. [8] 宋俊敏, 万丹婷, 郑中梅, 等. 美国CDC社区老人跌倒风险自评表在我国老年人群中测试和信效度[J]. 中国公共卫生, 2020, 36(4): 592-595. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGGW202004028.htmSONG J M, WAN D T, ZHENG Z M, et al. Reliability and validity of US CDC self-rated fall risk questionnaire among Chinese community-dwelling older adults[J]. Chinese Journal of Public Health, 2020, 36(4): 592-595. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGGW202004028.htm [9] MORSE J M, BLACK C, OBERLE K, et al. A prospective study to identify the fall-prone patient[J]. Soc Sci Med, 1989, 28(1): 81-86. doi: 10.1016/0277-9536(89)90309-2 [10] BARRETT B J, FARDY J M. Evaluation of diagnostic tests[J]. Methods Mol Biol, 2021, 2249: 319-333. [11] 汤淑女, 尹香君, 余卫, 等. 中国40岁及以上绝经后女性骨质疏松症患病率及其影响因素研究[J]. 中华流行病学杂志, 2022, 43(4): 509-516. doi: 10.3760/cma.j.cn112338-20210826-00680TANG S N, YIN X J, YU W, et al. Prevalence of osteoporosis and related factors in postmenopausal women aged 40 and above in China[J]. Chinese Journal of Epidemiology, 2022, 43(4):509-516. doi: 10.3760/cma.j.cn112338-20210826-00680 [12] HOKE M, OMAR N B, AMBURGY J W, et al. Impact of exercise on bone mineral density, fall prevention, and vertebral fragility fractures in postmenopausal osteoporotic women[J]. J Clin Neurosci, 2020, 76: 261-263. doi: 10.1016/j.jocn.2020.04.040 [13] BURNS E R, LEE R, HODGE S E, et al. Validation and comparison of fall screening tools for predicting future falls among older adults[J]. Arch Gerontol Geriatr, 2022, 101: 104713. DOI: 10.1016/j.archger.2022.104713. [14] DE HOND A A H, STEYERBERG E W, VAN CALSTER B. Interpreting area under the receiver operating characteristic curve[J]. Lancet Digital health, 2022, 4(12): e853-e855. DOI: 10.1016/S2589-7500(22)00188-1. [15] ALHARBI A A, AL AMER H S, ALBALWI A A, et al. Cross-cultural adaptation and psychometric properties of the Arabic version of the fall risk questionnaire[J]. Int J Environ Res Public Health, 2023, 20(8): 5606. DOI: 10.3390/ijerph20085606. [16] SONG C Y, TSAUO J Y, FANG P H, et al. Physical fitness among community-dwelling older women with and without risk of falling-the Taipei study, Taiwan[J]. Int J Environ Res Public Health, 2021, 18(14): 7243. DOI: 10.3390/ijerph18147243. [17] LOHSE K R, DUMMER D R, HAYES H A, et al. Combining the AM-PAC "6-Clicks" and the Morse fall scale to predict individuals at risk for falls in an inpatient rehabilitation hospital[J]. Arch Phys Med Rehabil, 2021, 102(12): 2309-2315. doi: 10.1016/j.apmr.2021.07.800 [18] WONG M M C, PANG P F, CHAN C F, et al. Wilson Sims fall risk assessment tool versus Morse fall scale in psychogeriatric inpatients: a multicentre study[J]. East Asian Arch Psychiatry, 2021, 31(3): 67-70. doi: 10.12809/eaap2113 [19] GERSTLE E E, O'CONNOR K, KEENAN K G, et al. The influence of age and fall history on single transition step kinematics[J]. Clin Biomech(Bristol, Avon), 2021, 89: 105456. DOI: 10.1016/j.clinbiomech.2021.105456. [20] MONTERO-ODASSO M, VAN DER VELDE N, MARTIN F C, et al. World guidelines for falls prevention and management for older adults: a global initiative[J]. Age Ageing, 2022, 51(9): 1-36. [21] GARBIN A J, FISHER B E. The interplay between fear of falling, balance performance, and future falls: data from the national health and aging trends study[J]. J Geriatr Phys Ther, 2023, 46(2): 110-115. doi: 10.1519/JPT.0000000000000324 -





 下载:
下载: