Predictive value of serum levels of estrone and estriol for pregnancy outcomes in patients with threatened abortion
-
摘要:
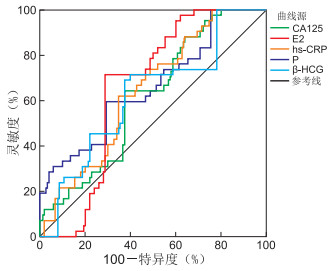
目的 探究先兆流产孕妇血清中雌酮(E1)和雌三醇(E3)水平及其对不良妊娠结局的预测价值,旨在为临床早期干预治疗提供参考。 方法 选取广元市妇幼保健院2020年1月—2021年12月收治的122例先兆流产孕妇,根据是否流产将先兆流产孕妇分为妊娠结局良好组(80例)和妊娠结局不良组(42例),同时选取70例相同年龄层在本院分娩的正常妊娠孕妇作为对照组。比较血清中E1和E3水平在不同组别中的差异,通过Pearson分析评估E1、E3水平与血清中相关激素的相关性,通过二元logistic回归分析研究孕妇发生不良妊娠结局的影响因素,通过ROC曲线评估E1、E3水平对孕妇发生不良妊娠结局的诊断价值。 结果 妊娠结局不良组血清β-人绒毛膜促性腺激素(β-HCG)、孕酮(P)、雌二醇(E2)、E1及E3水平均较对照组和妊娠结局良好组降低,而血清超敏C反应蛋白、糖类抗原125较对照组和妊娠结局良好组升高(P<0.05)。血清E1、E3水平与血清β-HCG、P及E2水平呈正相关关系(P<0.05)。二元logistic回归分析显示,血清E1、E3升高均是不良妊娠结局发生的影响因素(P<0.05)。ROC曲线显示,血清E1、E3联合诊断的AUC(0.841)明显高于单一E1(0.745)或E3(0.735)诊断,灵敏度和特异度分别为85.71%和86.00%。 结论 妊娠结局不良的孕妇血清中E1、E3水平降低。E1、E3联合诊断对孕妇发生不良妊娠结局具有良好的诊断效能,可为临床早期干预治疗提供重要的依据。 Abstract:Objective This study aims to investigate the serum levels of estrone (E1) and estriol (E3) in pregnant women with threatened miscarriage and evaluate their predictive value for adverse pregnancy outcomes. The findings will provide valuable reference for early clinical intervention and treatment. Methods A total of 122 pregnant women with threatened abortion who were admitted to Guangyuan Maternal and Child Health Hospital from January 2020 to December 2021 were selected. Based on whether they experienced a miscarriage, the pregnant women with threatened abortion were divided into two groups: the good pregnancy outcome group (n=80) and the poor pregnancy outcome group (n=42). Additionally, 70 normal pregnant women of the same age who delivered in our hospital were selected as the control group. The levels of E1 and E3 in serum were compared among the different groups. Pearson analysis was used to evaluate the correlation between E1 and E3 levels and other related hormones in serum. Furthermore, we conducted binary logistic analysis to analyze the factors contributing to poor pregnancy outcomes. Lastly, we used ROC curve analysis to assess the diagnostic value of E1 and E3 levels in predicting poor pregnancy outcomes. Results The serum levels of β-human chorionic gonadotropin (β-HCG), progesterone (P), estradiol (E2), E1, and E3 in the poor pregnancy outcome group were lower than those compared to both the control group and the good pregnancy outcome group (P < 0.05).Conversely, the levels of high sensitivity C-reactive protein and cancer antigen 125 in serum were higher compared to the control group and the good pregnancy outcome group (P < 0.05). There was a positive correlation between the serum levels of E1, E3, β-HCG, P, and E2 were positively correlated (P < 0.05). Binary logistic regression analysis showed that elevated E1 and E3 were influencing protective factors against adverse pregnancy outcomes (P < 0.05). The ROC curve demonstrated that the combined diagnosis of E1 and E3 (0.841) had a significantly higher area under the curve (AUC) compared to using E1 (0.745) or E3 (0.735) alone. The sensitivity and specificity of the combined diagnosis were 85.71% and 86.00%, respectively. Conclusion The levels of E1 and E3 in serum decreased in pregnant women experiencing poor pregnancy outcomes. The combined diagnosis of E1 and E3 has a good diagnostic efficiency for identifying poor pregnancy outcomes, offering a valuable foundation for early clinical intervention and treatment. -
Key words:
- Threatened abortion /
- Estrone /
- Estriol /
- ROC curve
-
表 1 3组孕妇一般资料比较
Table 1. Comparison of general data among three groups of pregnant women
组别 例数 年龄(x±s, 岁) 妊娠前BMI(x±s) 孕周(x±s, 周) 孕次(x±s, 次) 初产妇[例(%)] 甲亢[例(%)] 吸烟史[例(%)] 对照组 70 27.52±3.51 21.03±1.51 8.75±2.06 1.35±0.39 31(44.29) 5(7.14) 12(17.14) 妊娠结局良好组 80 27.15±3.23 21.22±1.68 8.30±2.23 1.24±0.28 35(43.75) 9(11.25) 15(18.75) 妊娠结局不良组 42 28.03±3.65 21.57±1.29 8.02±2.42 1.29±0.32 17(40.48) 4(9.52) 7(16.67) 统计量 0.916a 1.614a 1.576a 2.044a 0.171b 0.742b 0.106b P值 0.402 0.202 0.210 0.132 0.918 0.690 0.948 注:a为F值,b为χ2值。 表 2 3组孕妇血清指标比较(x±s)
Table 2. Comparison of serum indicators in three groups of pregnant women (x±s)
组别 例数 hs-CRP(mg/L) β-HCG(mIU/L) P(nmol/L) E2(ng/mL) E1(ng/mL) E3(ng/mL) CA125(IU/mL) FSH(ng/mL) AMH(ng/mL) 对照组 70 5.03±1.38 37 188.52±1 003.21 27.52±5.24 33.16±8.79 5.32±1.18 12.15±3.06 17.23±4.10 5.68±2.06 3.43±0.96 妊娠结局良好组 80 14.19±3.52a 32 207.15±1 325.23a 22.62±5.03a 15.98±4.57a 2.56±0.59a 7.26±1.79a 28.50±6.23a 5.46±1.96 3.74±0.94 妊娠结局不良组 42 20.67±4.03ab 29 828.13±1 231.65ab 18.13±5.78ab 10.88±3.03ab 1.07±0.33ab 4.09±1.06ab 40.12±10.28ab 5.43±1.90 3.76±0.95 F值 368.592 577.509 43.151 214.043 396.785 186.749 155.575 0.303 2.389 P值 <0.001 <0.001 <0.001 <0.001 <0.001 <0.001 <0.001 0.739 0.094 注:与对照组比较,aP<0.05;与妊娠结局良好组比较,bP<0.05。 表 3 血清E1、E3水平与血清指标的相关性分析
Table 3. Correlation analysis of serum E1 and E3 levels with serum indicators
项目 E1(ng/mL) E3(ng/mL) r值 P值 r值 P值 β-HCG(mIU/L) 0.681 <0.001 0.714 <0.001 P(nmol/L) 0.675 <0.001 0.701 <0.001 hs-CRP(mg/L) -0.303 0.082 -0.315 0.069 CA125(IU/mL) -0.234 0.106 -0.241 0.101 FSH(ng/mL) 0.275 0.091 0.201 0.180 AMH(ng/mL) -0.164 0.375 -0.147 0.396 E2(ng/mL) 0.826 <0.001 0.835 <0.001 表 4 二元logistic回归模型分析不良妊娠结局的影响因素
Table 4. Binary logistic regression model analysis of adverse pregnancy outcomes factors
变量 B SE Waldχ2 P值 OR值 95% CI β-HCG -0.529 0.333 2.524 0.112 0.589 0.307~1.132 P -0.620 0.408 2.309 0.129 0.538 0.242~1.197 hs-CRP 0.526 0.307 2.936 0.087 1.692 0.927~3.089 CA125 0.419 0.340 1.519 0.218 1.520 0.781~2.961 E2 -0.686 0.317 4.683 0.030 0.504 0.271~0.938 E1 -0.569 0.257 4.902 0.027 0.566 0.342~0.937 E3 -0.729 0.301 5.866 0.015 0.482 0.267~0.870 表 5 各项指标对不良妊娠结局发生的诊断价值
Table 5. Diagnostic value of various indicators for adverse pregnancy outcomes
项目 AUC(95% CI) 最佳截断值 约登指数 灵敏度(%) 特异度(%) β-HCG 0.623(0.528~0.717)ab 30 225 0.32 69.05 62.67 P 0.662(0.566~0.757)ab 19.99 0.30 59.52 70.67 hs-CRP 0.643(0.557~0.729)ab 18.48 0.27 61.90 65.33 CA125 0.616(0.528~0.704)ab 36.73 0.27 64.29 62.67 E2 0.655(0.578~0.731) 12.76 0.43 71.43 71.33 E1 0.745(0.673~0.817) 1.58 0.46 69.05 77.33 E3 0.735(0.662~0.808) 4.38 0.45 73.81 72.00 E1+E3 0.841(0.761~0.921)ab 85.71 86.00 注:与E1比较, aP<0.05;与E3比较, bP<0.05。 -
[1] 杜黎黎, 蔡璐, 王林. 先兆流产患者保胎后妊娠结局的相关影响因素分析[J]. 中国妇幼保健, 2021, 36(3): 629-631. https://www.cnki.com.cn/Article/CJFDTOTAL-ZFYB202103046.htmDU L L, CAI L, WANG L. Analysis of related influencing factors of pregnancy outcome in patients with threatened abortion after fetal protection[J]. Maternal and Child Health Care of China, 2021, 36(3): 629-631. https://www.cnki.com.cn/Article/CJFDTOTAL-ZFYB202103046.htm [2] 张丽, 姜凤华, 关莹莹, 等. 血清HCG、P、E2水平与早期先兆流产中医证型的关系研究[J]. 中华中医药学刊, 2023, 41(4): 221-225. https://www.cnki.com.cn/Article/CJFDTOTAL-ZYHS202304046.htmZHANG L, JIANG F H, GUAN Y Y, et al. Relationship between serum HCG, P, E2 and TCM syndrome types of early threatened abortion[J]. Chinese Archives of Traditional Chinese Medicine, 2023, 41(4): 221-225. https://www.cnki.com.cn/Article/CJFDTOTAL-ZYHS202304046.htm [3] HENRÍQUEZ S, KOHEN P, XU X, et al. Significance of pro-angiogenic estrogen metabolites in normal follicular development and follicular growth arrest in polycystic ovary syndrome[J]. Hum Reprod, 2020, 35(7): 1655-1665. doi: 10.1093/humrep/deaa098 [4] ZHOU Y P, GU B X, BRICHANT G, et al. The steroid hormone estriol (E3) regulates epigenetic programming of fetal mouse brain and reproductive tract[J]. BMC Biol, 2022, 20(1): 93. DOI: 10.1186/s12915-022-01293-4. [5] 谢幸, 孔北华, 段涛. 妇产科学[M]. 9版. 北京: 人民卫生出版社, 2018: 70-73.XIE X, KONG B H, DUAN T. Obstetrics and gynecology[M]. 9th edition. Beijing: People ' s Medical Publishing House, 2018: 70-73. [6] 吴丹, 楼叶琳. 经阴道超声检测黄体及子宫螺旋动脉血流用于诊断早孕流产的临床价值[J]. 中华全科医学, 2021, 19(5): 830-832, 837. doi: 10.16766/j.cnki.issn.1674-4152.001928WU D, LIU Y L. Clinical value of transvaginal ultrasonography in the diagnosis of abortion during early pregnancy[J]. Chinese Journal of General Practice, 2021, 19(5): 830-832, 837. doi: 10.16766/j.cnki.issn.1674-4152.001928 [7] TEBBENS M, HEIJBOER A C, T ' SJOEN G, et al. The role of estrone in feminizing hormone treatment[J]. J Clin Endocrinol Metab, 2022, 107(2): e458-e466. doi: 10.1210/clinem/dgab741 [8] GARGUS E S, BAE Y, CHEN J, et al. An ovarian steroid metabolomic pathway analysis in basal and polycystic ovary syndrome (PCOS)-like gonadotropin conditions reveals a hyperandrogenic phenotype measured by mass spectrometry[J]. Biomedicines, 2022, 10(7): 1646. DOI: 10.3390/biomedicines10071646. [9] JI X Y, LI N, MA M, et al. Comparison of the mechanisms of estrogen disrupting effects between triphenyl phosphate (TPhP) and tris (1, 3-dichloro-2-propyl) phosphate (TDCIPP)[J]. Ecotoxicol Environ Saf, 2022, 229(9): 1130-1139. [10] ALABIAD M A, SAID W M M, GAD A H, et al. Evaluation of different doses of the aromatase inhibitor letrozole for the treatment of ectopic pregnancy and its effect on villous trophoblastic tissue[J]. Reprod Sci, 2022, 29(10): 2983-2994. doi: 10.1007/s43032-022-00993-0 [11] ZHANG J, CHEN L, ZHENG C H, et al. Effect of Shoutai Pills on Th1/Th2 cytokines in serum and endometrium of rats with stimulated ovulation[J]. Curr Med Sci, 2019, 39(2): 285-290. doi: 10.1007/s11596-019-2032-4 [12] HE L G, ZHANG W J, YANG S Y, et al. Impact of genetic variants in IL-2RA and IL-2RB on breast cancer risk in Chinese Han women[J]. Biochem Genet, 2021, 59(3): 697-713. doi: 10.1007/s10528-021-10029-y [13] TEJERA E, PÉREZ-CASTILLO Y, CHAMORRO A, et al. A multi-objective approach for drug repurposing in preeclampsia[J]. Molecules, 2021, 26(4): 63-70. [14] RUSIDZÉ M, GARGAROS A, FÉBRISSY C, et al. Estrogen actions in placental vascular morphogenesis and spiral artery remodeling: a comparative view between humans and mice[J]. Cells, 2023, 12(4): 620. DOI: 10.3390/cells12040620. [15] ZHANG S J, TANG Y, WANG X J, et al. Estrogen valerate pretreatment with the antagonist protocol does not increase oocyte retrieval in patients with low ovarian response: a randomized controlled trial[J]. Hum Reprod, 2022, 37(7): 1431-1439. doi: 10.1093/humrep/deac081 [16] GIBSON D A, ESNAL-ZUFIAURRE A, BAJO-SANTOS C, et al. Profiling the expression and function of oestrogen receptor isoform ER46 in human endometrial tissues and uterine natural killer cells[J]. Hum Reprod, 2020, 35(3): 641-651. doi: 10.1093/humrep/dez306 [17] HIROTA Y. Progesterone governs endometrial proliferation -differentiation switching and blastocyst implantation[J]. Endocr J, 2019, 66(3): 199-206. doi: 10.1507/endocrj.EJ18-0431 -





 下载:
下载: