Learning curve of the distal radial access for coronary intervention
-
摘要:
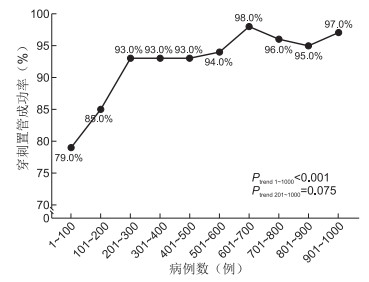
目的 探讨经远端桡动脉(DRA)行冠状动脉介入诊疗中操作数量与穿刺置管成功率的关系,并分析穿刺置管失败的危险因素。 方法 回顾性分析2021年1月—2022年12月北京潞河医院心内科单一术者经DRA入路行冠状动脉介入诊疗的患者1 000例,根据操作时间和先后顺序分为10组,每100例为一个阶段,主要研究终点为每100例患者的穿刺置管成功率,次要研究终点为每100例患者的一次性穿刺成功率和穿刺置管时间。采用logistic回归分析研究DRA穿刺置管失败的相关因素。 结果 1 000例患者中,DRA穿刺置管成功率为92.3%。200例操作后,DRA的穿刺置管成功率可达93.0%以上(P=0.075),一次性穿刺成功率从最初的74.0%增加至96.0%(P < 0.001),穿刺置管中位时间从3.00 min减少到2.00 min(P < 0.001)。Logistic回归分析显示,DRA直径(P=0.020)与左侧入路(P=0.046)均为DRA穿刺置管失败的影响因素。 结论 DRA路径需200例操作经验后穿刺置管成功率可达93.0%以上并维持稳定状态,小DRA直径和左侧入路是DRA穿刺置管失败的主要因素。 -
关键词:
- 远端桡动脉 /
- 经皮冠状动脉介入治疗 /
- 学习曲线 /
- 穿刺置管成功率
Abstract:Objective To determine the correlation between operator experience in distal transradial coronary intervention (dTRI) and the successful cannulation rate of the distal radial artery (DRA), as well as to identify risk factors for puncture and cannulation failures. Methods From January 2021 to December 2022, 1 000 patients who underwent dTRI via DRA by a single interventionist in Beijing Luhe Hospital were retrospectively enrolled. These patients were chronologically ranked and divided into ten groups (100 cases each) according to operation time and order. The primary endpoint was the successful cannulation rate of DRA for every 100 cases, while the secondary endpoints were the success rate of one-time puncture catheterization and puncture catheterization time. Logistic regression analysis was carried out to identify predictors of unsuccessful DRA. Results A total of 1 000 patients were enrolled, with a successful DRA cannulation rate of 92.3%. After 200 cases, this rate stabilized at 93.0% (P=0.075). The first attempt DRA puncture success rate improved from 74.0% to 96.0%, while the median sheath cannulation time decreased from 3.00 min to 2.00 min (P < 0.001). Logistic regression analysis showed that a negative association between DRA diameter (P=0.020) and cannulation failure, and a positive association with left artery access (P=0.046). Conclusion Achieving over 93.0% success in DRA puncture and cannulation becomes consistent after 200 cases. Small DRA diameter and left-sided access are key predictors of failure. -
表 1 ACS患者dTRI穿刺置管成功组和失败组基线资料比较
Table 1. Comparison of baseline data between successful and failed dTRI puncture catheterization groups in patients with ACS
项目 总数(n=1 000) 成功组(n=923) 失败组(n=77) 统计量 P值 年龄(x±s,岁) 61.2±12.9 61.1±12.9 63.1±13.8 -1.318a 0.188 性别[例(%)] 11.869b 0.001 男性 790(79.0) 741(80.3) 49(63.6) 女性 210(21.0) 182(19.7) 28(36.4) 身高(x±s,cm) 167.1±9.5 167.3±9.6 165.3±8.1 1.704a 0.089 体重[M(P25, P75),kg] 73.0(65.0, 80.0) 73.0(65.0, 80.0) 75.0(65.0, 82.5) -0.642c 0.526 BMI[M(P25, P75)] 25.9(23.7, 28.4) 25.8(23.5, 28.4) 26.8(24.5, 29.4) -2.377c 0.017 危险因素[例(%)] 高血压 628(62.8) 580(62.8) 48(62.3) 0.008b 0.930 糖尿病 322(32.2) 296(32.1) 26(33.8) 0.094b 0.759 高脂血症 387(38.7) 357(38.7) 30(39.0) 0.002b 0.961 当前吸烟 460(46.0) 437(47.3) 23(29.9) 8.738b 0.003 慢性肾功能不全 29(2.9) 24(2.6) 5(6.5) 3.826b 0.065 心房颤动 60(6.0) 52(5.6) 8(10.4) 2.069b 0.126 脑卒中 111(11.1) 101(10.9) 10(13.0) 0.301b 0.583 既往PRA[例(%)] 231(23.1) 210(22.8) 21(27.3) 0.818b 0.366 既往DRA[例(%)] 58(5.8) 57(6.2) 1(1.3) 2.266b 0.121 既往PCI[例(%)] 259(25.9) 241(26.1) 18(23.4) 0.277b 0.599 射血分数(x±s,%) 64.1±9.8 64.1±9.9 64.3±8.8 -0.193a 0.847 右侧入路[例(%)] 985(98.5) 912(98.8) 73(94.8) 5.237b 0.023 诊断[例(%)] UAP/NSTEMI 506(50.6) 464(50.3) 42(54.5) 0.520b 0.471 STEMI 456(45.6) 424(45.9) 32(41.6) 0.549b 0.459 其他 38(3.8) 35(3.8) 3(3.9) < 0.001b 0.999 操作[例(%)] CAG 142(14.2) 131(14.2) 11(14.3) 0.001b 0.982 PCI 858(85.8) 792(85.8) 66(85.7) 0.001b 0.982 DRA直径(x±s,mm) 2.3±0.4 2.3±0.4 2.0±0.4 5.409a < 0.001 PRA直径(x±s,mm) 3.0±0.5 3.0±0.5 2.7±0.4 5.280a < 0.001 注:a为t值,b为χ2值,c为Z值。CAG为冠状动脉造影(coronary angiography);PCI为经皮冠状动脉介入治疗(percutaneous coronary intervention);UAP为不稳定型心绞痛(unstable angina pectoris);NSTEMI为非ST段抬高型心肌梗死(non ST-segment elevation myocardial infarction);STEMI为ST段抬高型心肌梗死(ST-segment elevation myocardial infarction)。 表 2 变量赋值情况
Table 2. Variable assignment
变量 赋值方法 性别 男性=0,女性=1 身高 以实际值赋值 BMI 以实际值赋值 当前吸烟 无=0,有=1 慢性肾功能不全 无=0,有=1 入路方式 右侧=0,左侧=1 DRA直径 以实际值赋值 PRA直径 以实际值赋值 表 3 ACS患者远端桡动脉穿刺置管失败的多因素logistic回归分析
Table 3. Multivariate logistic regression analysis of failed distal radial artery puncture catheterization in ACS patients
变量 B SE Waldχ2 P值 OR值 95% CI 女性 0.310 0.367 0.717 0.397 1.364 0.665~2.797 身高 0.006 0.019 0.088 0.767 1.006 0.968~1.044 BMI < 0.001 0.003 0.010 0.921 1.000 0.994~1.005 当前吸烟 -0.404 0.285 2.006 0.157 0.667 0.381~1.168 慢性肾功能不全 0.667 0.541 1.523 0.217 1.948 0.675~5.621 左侧入路 1.262 0.633 3.972 0.046 3.533 1.021~12.224 DRA直径 -1.053 0.451 5.451 0.020 0.349 0.144~0.844 PRA直径 -0.475 0.415 1.306 0.253 0.622 0.276~1.404 表 4 ACS患者DRA和PRA入路术后并发症发生情况比较
Table 4. Comparison of postoperative complications between DRA and PRA approaches in ACS patients
项目 例数 止血时间
[M(P25, P75), h]PRAO
[例(%)]DRAO
[例(%)]血肿
[例(%)]EASY≥Ⅱ血肿
[例(%)]假性动脉瘤
[例(%)]动静脉瘘
[例(%)]手指麻木
[例(%)]DRA 923 3.27(3.00, 3.72) 19(2.1)b 37(4.0) 73(7.9) 16(1.8) 2(0.2) 1(0.1) 10(1.1) PRA 66 6.19(5.65, 6.64) 6(9.1)c 3(4.6) 6(9.1) 1(1.5) 0 0 1(1.5) 统计量 -10.445a 12.363d 0.046d 0.117d 0.017d 0.143d 0.072d 0.104d P值 < 0.001 0.005 0.745 0.734 0.999 0.999 0.999 0.534 注: a为Z值, d为χ2值。b为与同组DRAO发生率比较,差异有统计学意义(2.1% vs. 4.0%, χ2=5.967,P=0.015);c为与同组DRAO发生率比较差异无统计学意义(9.1% vs. 4.6%, χ2=1.093,P=0.296)。 -
[1] NEUMANN F J, SOUSA-UVA M, AHLSSON A, et al. 2018 ESC/EACTS guidelines on myocardial revascularization[J]. Eur Heart J, 2019, 40(2): 87-165. doi: 10.1093/eurheartj/ehy394 [2] 中华医学会心血管病学分会, 中华心血管病杂志编辑委员会. 急性ST段抬高型心肌梗死诊断和治疗指南(2019)[J]. 中华心血管病杂志, 2019, 47(10): 766-783.Chinese Society of Cardiology of Chinese Medical Association, Editorial Board of Chinese Journal of Cardiology. 2019 Chinese Society of Cardiology (CSC) guidelines for the diagnosis and management of patients with ST-segment elevation myocardial infarction[J]. Chinese Journal of Cardiology, 2019, 47(10): 766-783. [3] 吴士礼, 唐碧, 刘进军, 等. 经桡动脉急诊PCI与溶栓后早期PCI对ST段抬高型急性心肌梗死患者心功能的影响[J]. 中华全科医学, 2019, 17(11): 1829-1832. doi: 10.16766/j.cnki.issn.1674-4152.001067WU S L, TANG B, LIU J J, et al. Observation of effect of transradial emergency PCI and early PCI after thrombolysis on cardiac function in patients with ST-segment elevation acute myocardial infarction[J]. Chinese Journal of General Practice, 2019, 17(11): 1829-1832. doi: 10.16766/j.cnki.issn.1674-4152.001067 [4] BERNAT I, AMINIAN A, PANCHOLY S, et al. Best practices for the prevention of radial artery occlusion after transradial diagnostic angiography and intervention: an international consensus paper[J]. JACC Cardiovasc Interv, 2019, 12(22): 2235-2246. doi: 10.1016/j.jcin.2019.07.043 [5] TSIGKAS G, PAPAGEORGIOU A, MOULIAS A, et al. Distal or traditional transradial access site for coronary procedures: a single-center, randomized study[J]. JACC Cardiovasc Interv, 2022, 15(1): 22-32. doi: 10.1016/j.jcin.2021.09.037 [6] LEE J W, PARK S W, SON J W, et al. Real-world experience of the left distal transradial approach for coronary angiography and percutaneous coronary intervention: a prospective observational study (ledra)[J]. EuroIntervention, 2018, 14(9): e995-e1003. doi: 10.4244/EIJ-D-18-00635 [7] FEGHALY J, CHEN K, BLANCO A, et al. Distal versus conventional radial artery access for coronary catheterization: a systematic review and meta-analysis[J]. Catheter Cardiovasc Interv, 2023, 101(4): 722-736. doi: 10.1002/ccd.30602 [8] SGUEGLIA G A, DI GIORGIO A, GASPARDONE A, et al. Anatomic basis and physiological rationale of distal radial artery access for percutaneous coronary and endovascular procedures[J]. JACC Cardiovasc Interv, 2018, 11(20): 2113-2119. doi: 10.1016/j.jcin.2018.04.045 [9] VERGARA-GARCIA D, GOMEZ-PAZ S, ROBINSON T M, et al. Transition to radial approach for neurovascular procedures is safe and convenient: characterization of a learning experience[J]. Oper Neurosurg (Hagerstown), 2020, 19(5): 489-494. doi: 10.1093/ons/opaa133 [10] BERTRAND O F. Acute forearm muscle swelling post transradial catheterization and compartment syndrome: prevention is better than treatment![J]. Catheter Cardiovasc Interv, 2010, 75(3): 366-368. doi: 10.1002/ccd.22448 [11] 王欢欢, 刘丹, 郭继东, 等. 经鼻烟壶区远端桡动脉入路在冠状动脉造影和经皮冠状动脉介入治疗中的效果和安全性分析[J]. 中国循环杂志, 2021, 36(12): 1168-1172.WANG H H, LIU D, GUO J D, et al. Efficacy and safety of the distal transradial approach in coronary angiography and percutaneous coronary intervention[J]. Chinese Circulation Journal, 2021, 36(12): 1168-1172. [12] LEE J W, SON J W, GO T H, et al. Reference diameter and characteristics of the distal radial artery based on ultrasonographic assessment[J]. Korean J Intern Med, 2022, 37(1): 109-118. doi: 10.3904/kjim.2020.685 [13] ROH J W, KIM Y, LEE O H, et al. The learning curve of the distal radial access for coronary intervention[J]. Sci Rep, 2021, 11(1): 13217. DOI: 10.1038/s41598-021-92742-7. [14] BOMPOTIS G C, GIANNOPOULOS G, KARAKANAS A I, et al. Left distal radial artery access for coronary angiography and interventions: a 12-month all-comers study[J]. J Invasive Cardiol, 2022, 34(7): E505-E509. [15] MORI S, HIRANO K, YAMAWAKI M, et al. A comparative analysis between ultrasound-guided and conventional distal transradial access for coronary angiography and intervention[J]. J Interv Cardiol, 2020, 2020: 7342732. DOI: 10.1155/2020/7342732. [16] 陈超, 朱壹明, 孙俊龙, 等. 影响远端桡动脉穿刺成功率相关因素分析[J]. 浙江中医药大学学报, 2021, 45(1): 28-33.CHEN C, ZHU Y M, SUN J L, et al. Analysis of the factors influencing the success rate of distal radial artery puncture[J]. Journal of Zhejiang Chinese Medical University, 2021, 45(1): 28-33. [17] KIM Y, AHN Y, KIM I, et al. Feasibility of coronary angiography and percutaneous coronary intervention via left snuffbox approach[J]. Korean Circ J, 2018, 48(12): 1120-1130. doi: 10.4070/kcj.2018.0181 [18] SOYDAN E, AKIN M. Left distal radial artery access site in primary percutaneous coronary intervention: is it safe?[J]. Balkan Med J, 2020, 37(5): 276-280. [19] FERRANTE G, CONDELLO F, RAO S V, et al. Distal vs conventional radial access for coronary angiography and/or intervention: a meta-analysis of randomized trials[J]. JACC Cardiovasc Interv, 2022, 15(22): 2297-2311. [20] YOSHIMACHI F, IKARI Y. Distal radial approach: a review on achieving a high success rate[J]. Cardiovasc Interv Ther, 2021, 36(1): 30-38. -





 下载:
下载: