Longitudinal study on adherence to dietary treatment and its influencing factors in patients with primary hepatic cancer
-
摘要:
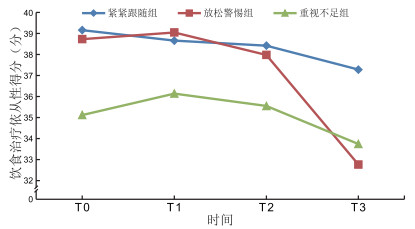
目的 随访观察原发性肝癌患者饮食治疗依从性的变化轨迹,并分析其影响因素。 方法 采用方便抽样法于2021年3月—2022年4月选取在温州医科大学附属第二医院住院首次治疗的243例肝癌患者为研究对象。出院前(T0)完成第1次问卷调查,首次治疗后1个月(T1)、3个月(T2)及6个月(T3)随访完成依从性量表调查。 结果 肝癌患者在T0、T1、T2和T3时点的饮食治疗依从性得分分别为(37.62±6.53)分、(37.82±6.34)分、(37.12±6.10)分和(34.43±5.76)分,T0-T1、T0-T2和T1-T2间的差异无统计学意义(P>0.05),而T0-T3、T1-T3、T2-T3间的差异有统计学意义(P < 0.05)。使用潜类别增长模型可识别3个潜在轨迹类别:“紧紧跟随组”占比30.87%(75例),“放松警惕组”占比33.33%(81例),“重视不足组”占比35.80%(87例)。宗教信仰、营养不良风险、独居和健康信念是肝癌患者饮食治疗依从性潜在轨迹类别的影响因素。 结论 医护人员应尊重患者的宗教信仰,帮助重度营养不良风险的患者形成正确的疾病认知,配合社区开展独居患者精准关爱服务,准确评估患者的健康信念状况,提高饮食治疗的依从性。 Abstract:Objective To explore the change track of dietary treatment adherence of primary hepatic cancer patients and its influencing factors. Methods A convenience sample of 243 hepatic cancer patients undergoing their first treatment in the Second Affiliated Hospital of Wenzhou Medical University between March 2021 and April 2022 was selected. The initial data collection was completed before discharge (T0), followed by collecting data on dietary treatment adherence scale at 1 month (T1), 3 months (T2) and 6 months (T3) after the first treatment. Results The dietary treatment adherence scores at points T0, T1, T2 and T3 were (37.62±6.53) points, (37.82±6.34) points, (37.12±6.10) points and (34.43±5.76) points. The differences between T0-T1, T0-T2 and T1-T2 were not statistically significant (P>0.05), while the differences between T0-T3, T1-T3 and T2-T3 were statistically significant (P < 0.05). Three potential trajectory categories could be identified by the potential category growth model: "closely follow group" accounted for 30.87% (75 cases), "relaxed group" accounted for 33.33% (81 cases) and "underappreciated group" accounted for 35.80% (87 cases). Religious beliefs, risk of malnutrition, living alone and health beliefs were the influencing factors in determining the potential trajectory category of dietary treatment adherence. Conclusion Medical staff should respect patients ' religious beliefs, assist patients at risk of severe malnutrition in developing a correct understanding of the disease, cooperate with the community to provide accurate care services for patients living alone, accurately assess their health beliefs, and improve the diet treatment adherence. -
Key words:
- Primary hepatic cancer /
- Dietary treatment adherence /
- Longitudinal study
-
表 1 PHC患者各时点的饮食治疗依从性(x ±s,分)
Table 1. Dietary treatment adherence of PHC patients at different time points (x ±s, points)
项目 T0 T1 T2 T3 日常饮食管理行为 3.29±0.51 3.38±0.53 3.43±0.56 2.98±0.44 饮食依从性态度 3.21±0.51 3.31±0.51 3.09±0.55 3.17±0.51 遵医饮食行为 3.46±0.54 3.40±0.52 3.21±0.49 3.02±0.47 家属支持度 3.66±0.58 3.53±0.61 3.54±0.58 3.25±0.55 限酒行为 3.89±0.62 3.82±0.58 3.72±0.59 3.63±0.54 总分 3.42±0.61 3.44±0.59 3.39±0.57 3.13±0.52 表 2 PHC患者饮食治疗依从性的潜在轨迹类别拟合结果
Table 2. The fitness of potential trajectory categories of dietary treatment adherence in PHC patients
类别数 AIC BIC aBIC 信息熵 LMRT(P值) BLRT(P值) 类别概率(%) 1 9 386.258 9 430.983 9 391.192 100 2 9 108.562 9 165.290 9 114.381 0.865 < 0.001 < 0.001 55.97/44.03 3 8 976.577 9 045.337 8 983.062 0.910 0.034 < 0.001 30.87/33.33/35.80 4 8 922.246 9 003.706 8 929.975 0.916 0.215 0.188 30.86/29.22/34.16/5.76 5 8 900.148 8 994.132 8 911.848 0.922 0.523 0.389 25.51/29.22/25.93/15.23/4.11 表 3 PHC患者饮食治疗依从性的潜在轨迹类别的单因素分析[例(%)]
Table 3. Univariate analysis of the potential trajectory categories of dietary treatment adherence in PHC patients [cases (%)]
项目 分类 例数 类别1(n=75) 类别2(n=81) 类别4(n=87) 统计量 P值 性别 男性 139 34(24.46) 51(36.69) 54(38.85) 6.255a 0.044 女性 104 41(39.42) 30(28.85) 33(31.73) 文化程度 小学及以下 44 9(20.45) 13(29.55) 22(50.00) 9.940b 0.007 中学 95 26(27.37) 31(32.63) 38(40.00) 大专及以上 104 40(38.46) 37(35.58) 27(25.96) 独居 是 48 7(14.58) 15(31.25) 26(54.17) 10.849a 0.004 否 195 68(34.87) 66(33.85) 61(31.28) 宗教信仰 有 45 24(53.33) 13(28.89) 8(17.78) 14.373a 0.001 无 198 51(25.76) 68(34.34) 79(39.90) 肿瘤最大径(cm) <5 132 33(25.00) 43(32.58) 56(42.42) 7.407a 0.025 ≥5 111 42(37.84) 38(34.23) 31(27.93) 营养不良风险 低营养不良风险 203 69(33.99) 70(34.48) 64(31.53) 13.112b < 0.001 中度营养不良风险 30 4(13.33) 9(30.00) 17(56.67) 重度营养不良风险 10 2(20.00) 2(20.00) 6(60.00) 注:a为χ2值,b为H值。类别1为紧紧跟随组;类别2为放松警惕组;类别3为重视不足组。本表仅列出差异有统计学意义的变量。 表 4 变量赋值情况
Table 4. Variable assignment
变量 赋值方法 饮食治疗依从性潜在轨迹类别 类别1=1,类别2=2,类别3=3 性别 男性=0,女性=1 文化程度 小学及以下=1, 中学=2, 大专及以上=3 独居 否=0,是=1 宗教信仰 无=0,有=1 肿瘤最大径 <5 cm=0,≥5 cm=1 营养风险筛查 重营养不良风险=1, 中度营养不良风险=2, 轻度营养不良风险=3 表 5 PHC患者饮食治疗依从性潜在轨迹类别的logistic回归分析
Table 5. Logistic regression of the potential trajectory categories of dietary treatment adherence in PHC patients
项目 自变量 B值 SE Waldχ2 P值 OR(95% CI) 类别1与类别2a 宗教信仰 0.823 0.291 7.999 0.005 2.277(1.573~3.002) 营养风险筛查 0.683 0.269 6.447 0.011 1.980(1.234~2.551) 类别1与类别3b 是否独居 0.949 0.306 9.618 0.002 2.583(1.346~3.896) 健康信念 1.307 0.624 4.385 0.036 3.695(2.764~4.518) 宗教信仰 0.855 0.374 5.221 0.022 2.351(1.896~2.987) 类别2与类别3b 是否独居 0.883 0.331 7.110 0.008 0.414(0.186~0.621) 健康信念 0.587 0.245 5.746 0.017 1.799(1.257~2.342) 注:类别1为紧紧跟随组;类别2为放松警惕组;类别3为重视不足组。a类别2为参照组,b类别3为参照组。 -
[1] 肖文博, 朱广涵, 朱云, 等. 1990—2019年中国主要消化系统恶性肿瘤发病变化分析[J]. 中国肿瘤, 2022, 31(9): 693-700.XIAO W B, ZHU G H, ZHU Y, et al. Incidence of major digestive system cancers in China, 1990-2019[J]. China Cancer, 2022, 31(9): 693-700. [2] 潘杰, 毛景松, 姚天虹, 等. 影像组学在肝癌中应用的研究进展[J]. 中国CT和MRI杂志, 2023, 21(4): 174-177. doi: 10.3969/j.issn.1672-5131.2023.04.061PAN J, MAO J S, YAO T H, et al. The research progress in the application of radiomics in liver cancer[J]. Chinese Journal of CT and MRI, 2023, 21(4): 174-177. doi: 10.3969/j.issn.1672-5131.2023.04.061 [3] 陶敏洁, 雷宇, 金俊, 等. 个体化饮食指导对肝癌患者肝动脉灌注化疗栓塞术后营养状况和生活质量的影响[J]. 中华全科医学, 2022, 20(3): 507-510. doi: 10.16766/j.cnki.issn.1674-4152.002388TAO M J, LEI Y, JIN J, et al. Effect of individualised dietary guidance on nutritional status and quality of life of liver cancer patients after TACE[J]. Chinese Journal of General Practice, 2022, 20(3): 507-510. doi: 10.16766/j.cnki.issn.1674-4152.002388 [4] OKADOME K, BABA Y, YAGI T, et al. Prognostic nutritional index, tumor-infiltrating lymphocytes, and prognosis in patients with esophageal cancer[J]. Ann Surg, 2020, 271(4): 693-700. doi: 10.1097/SLA.0000000000002985 [5] ARENDS J, STRASSER F, GONELLA S, et al. Cancer cachexia in adult patients: ESMO Clinical Practice Guidelines[J]. ESMO Open, 2021, 40(5): 2898-2913. [6] 夏小平. 饮食调整及症状管理对胃癌术后患者营养状况、饮食依从性及生活质量水平的影响[J]. 中外医学研究, 2021, 19(18): 161-164.XIA X P. Influence of dietary adjustment and symptom management on levels of nutritional status, dietary compliance and quality of life in postoperative patients with gastric cancer surgery[J]. Chinese And Foreign Medical Research, 2021, 19(18): 161-164. [7] 郑芹, 周光花, 李春梅, 等. 肝癌术后患者饮食治疗依从性量表的编制及信效度[J]. 解放军护理杂志, 2015, 32(17): 15-18.ZHENG Q, ZHOU G H, LI C M, et al. Design of postoperative liver cancer patients diet treatment compliance scale and the reliability and validity analysis[J]. Military Nursing, 2015, 32(17): 15-18. [8] 吕雨梅, 郭玉成, 周郁秋. 脑卒中患者康复锻炼依从性发展轨迹及其潜在类别预测因素分析[J]. 中华护理杂志, 2023, 58(17): 2103-2111.LYU Y M, GUO Y C, ZHOU Y Q. Research on the developmental trajectory of rehabilitation exercise adherence and its potential classes predictors in stroke patients[J]. Chinese Journal of Nursing, 2023, 58(17): 2103-2111. [9] 中华人民共和国国家卫生健康委员会医政医管局. 原发性肝癌诊疗规范(2019年版)[J]. 中华消化病与影像杂志, 2020, 10(1): 22-48. doi: 10.3877/cma.j.issn.2095-2015.2020.01.007Medical Administration and Medical Management Bureau, National Health Commission, PRC. Standardization for diagnosis and treatment of hepatocellular carcinoma (2019 edition)[J]. Chinese Journal of Digestive Surgery, 2020, 10(1): 22-48. doi: 10.3877/cma.j.issn.2095-2015.2020.01.007 [10] 宋煜, 丁劲, 葸英博, 等. 老年心力衰竭病人衰弱的影响因素及风险预测模型的构建[J]. 护理研究, 2023, 37(14): 2538-2543. doi: 10.12102/j.issn.1009-6493.2023.14.010SONG Y, DING J, XI Y B, et al. Influencing factors and development of risk prediction model for frailty in elderly patients with heart failure[J]. Nursing Research, 2023, 37(14): 2538-2543. doi: 10.12102/j.issn.1009-6493.2023.14.010 [11] 季韶艳, 杨辉. 健康信念量表的跨文化调试与信效度评价[J]. 中国医学创新, 2013, 10(9): 139-141.JI S Y, YANG H. The cross-cultural debugging and evaluation reliability and validity of the health belief scale[J]. Medical Innovation of China, 2013, 10(9): 139-141. [12] 陆俊雯, 陈英, 曹松梅, 等. 基于Pender健康促进模式的慢性肝病病人饮食依从性影响因素的质性研究[J]. 循证护理, 2023, 9(18): 3336-3340. doi: 10.12102/j.issn.2095-8668.2023.18.020LU J W, CHEN Y, CAO S M, et al. Qualitative study on the influencing factors of dietary compliance in chronic liver disease patients based on the Pender health promotion model[J]. Chinese Evidence-Based Nursing, 2023, 9(18): 3336-3340. doi: 10.12102/j.issn.2095-8668.2023.18.020 [13] 范春艳, 蔡银珠. 泌尿系结石病人健康促进生活方式现状及影响因素[J]. 全科护理, 2022, 20(34): 4886-4890. doi: 10.12104/j.issn.1674-4748.2022.34.033FAN C Y, CAI Y Z. Current status and influencing factors of health promotion and lifestyle in patients with urinary stones[J]. Chinese General Practice Nursing, 2022, 20(34): 4886-4890. doi: 10.12104/j.issn.1674-4748.2022.34.033 [14] 李京燃. 食管癌患者灵性健康现状及影响因素研究[D]. 扬州: 扬州大学, 2022.LI J R. Research on spiritual well-being and influencing factors of patients with esophageal cancer[D]. Yangzhou: Yangzhou University, 2022. [15] 杨宇, 练玉颖, 赵铟. 全球领导人营养不良倡议标准、患者全面主观营养评估及血清白蛋白在肿瘤患者营养不良诊断中的一致性研究[J]. 实用临床医药杂志, 2022, 26(2): 82-87.YANG Y, LIAN Y Y, ZHAO Y. A consistency study of global leadership initiative on malnutrition standard, patient-generated subjective global assessment and serum albumin in diagnosis of malnutrition in cancer patients[J]. Journal of Clinical Medicine in Practice, 2022, 26(2): 82-87. [16] 汪晨晨, 谢晖, 蔡维维. 社区老年人衰弱及其影响因素分析[J]. 中华全科医学, 2021, 19(4): 625-627, 683. doi: 10.16766/j.cnki.issn.1674-4152.001878WANG C C, XIE H, CAI W W. Analysis on the frailty of the elderly in community and its influencing factors[J]. Chinese Journal of General Practice, 2021, 19(4): 625-627, 683. doi: 10.16766/j.cnki.issn.1674-4152.001878 [17] 喻鹏. 透析饮食健康信念量表的汉化及应用[D]. 南昌: 南昌大学, 2023.YU P. Translation and application of the dialysis diet-related health belief questionnaire[D]. Nanchang: Nanchang University, 2023. -





 下载:
下载: