Risk prediction of placental abruption in singleton pregnancy with hypertensive disorders of pregnancy
-
摘要:
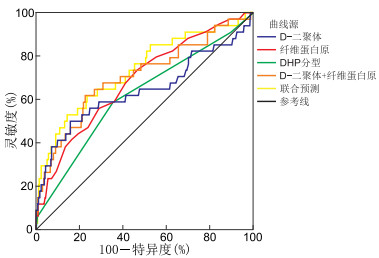
目的 探讨妊娠期高血压疾病(HDP)单胎妊娠患者并发胎盘早剥的危险因素以预测发生风险。 方法 回顾性分析2014年1月—2022年1月在安徽医科大学第二附属医院妇产科住院诊治且符合纳排标准的1 595例HDP患者临床资料,根据有无并发胎盘早剥分为研究组(发生胎盘早剥,34例)和对照组(未发生胎盘早剥,1 561例)。记录患者人口学特点、临床特点和实验室检测结果,采用单因素和多因素logistic回归模型分析HDP患者并发胎盘早剥的危险因素,并建立ROC曲线评价预测效能。 结果 1 595例HDP患者中,34例(2.13%)发生胎盘早剥。研究组血D-二聚体(P=0.005)、血肌酐(P=0.044)、血尿素氮(P=0.043)、谷草转氨酶(P=0.014)水平较高,血小板计数(P=0.012)、纤维蛋白原(P=0.011)水平较低,且发病与HDP分型相关。血D-二聚体水平(P=0.009)、纤维蛋白原水平(P < 0.01)及HDP分型[重度子痫前期(P=0.033)、子痫(P=0.001)]是HDP患者并发胎盘早剥的影响因素。其中,纤维蛋白原预测胎盘早剥的灵敏度最高(55.9%),D-二聚体特异度最高(84.2%),D-二聚体与纤维蛋白原联合预测灵敏度(61.8%)高于所有单项指标。HDP分型的AUC最低[0.617(95% CI: 0.515~0.720)],D-二聚体+纤维蛋白原+HDP分型联合预测的AUC最高[0.735(95% CI: 0.639~0.831)]。 结论 不同HDP表型对单胎妊娠患者并发胎盘早剥有显著影响,当纤维蛋白原降低、D-二聚体升高时,应高度警惕HDP单胎妊娠患者并发胎盘早剥。 Abstract:Objective To investigate the risk factors for placental abruption in singleton pregnancy with hypertensive disorders of pregnancy (HDP). Methods The clinical data of 1 595 HDP patients who met the inclusion criteria and were hospitalized in the Department of Obstetrics and Gynecology in the Second Affiliated Hospital of Anhui Medical University, from January 2014 to January 2022, were retrospectively analyzed. According to the occurrence of placental abruption, they were divided into study group (with placental abruption, 34 cases) and control group (without placental abruption, 1 561 cases). Demographic characteristics, clinical characteristics and laboratory test results were recorded. Univariate and multivariate logistic regression models were used to analyze the risk factors of HDP patients with placental abruption, and an ROC curve was constructed to evaluate the predictive efficacy. Results Among 1 595 HDP patients enrolled in this study, 34 were diagnosed with placental abruption (2.13%). Compared with the control group, the study group had higher levels of D-dimer (P=0.005), serum creatinine (P=0.044), blood urea nitrogen (P=0.043) and aspartate aminotransferase (P=0.014), and lower levels of platelet count (P=0.012) and fibrinogen (P=0.011). Serum D-dimer level (P=0.009), fibrinogen level (P < 0.01) and HDP types [severe preeclampsia (P=0.033), eclampsia (P=0.001)] were the influencing factors of placental abruption in HDP patients. Among them, fibrinogen had the highest predictive sensitivity (55.9%) and D-dimer had the highest specificity (84.2%). The sensitivity of the combination of D-dimer and fibrinogen was higher than that of the individual risk factors (61.8%). The AUC of HDP types was the lowest [0.617 (95% CI: 0.515-0.720)], and the AUC of D-dimer+fibrinogen+HDP types was the highest [0.735 (95% CI: 0.639-0.831)]. Conclusion Different types of HDP have a significant impact on placental abruption in singleton pregnancy. If fibrinogen is decreased and D-dimer is increased, placental abruption should be highly suspected in singleton pregnancy with HDP. -
Key words:
- Hypertensive disorders of pregnancy /
- Placental abruption /
- Risk factors /
- D-dimer /
- Fibrinogen
-
表 1 2组HDP单胎妊娠患者临床资料比较
Table 1. Comparison of clinical data of HDP single pregnancy patients in the two groups
项目 研究组(n=34) 对照组(n=1 561) 统计量 P值 年龄(x±s, 岁) 32.00±4.88 30.58±4.77 1.713a 0.087 孕前BMI(x±s) 21.94±3.69 23.16±3.95 1.787a 0.074 糖尿病或妊娠期糖尿病[例(%)] 8(23.53) 535(34.27) 1.710b 0.191 诊断HDP<32周[例(%)] 13(38.24) 439(28.12) 1.676b 0.196 自然流产病史[例(%)] 2(5.88) 56(3.59) 0.060b 0.807 收缩压(x±s, mmHg) 160.24±15.27 157.09±17.21 1.058a 0.290 舒张压(x±s, mmHg) 104.44±11.09 101.62±12.35 1.318a 0.188 血小板计数(x±s, ×109/L) 166.82±55.62 194.75±63.97 2.524a 0.012 血肌酐[M(P25, P75), μmol/L] 61(50, 75) 57(49, 66) -2.016c 0.044 血尿素氮[M(P25, P75), mmol/L] 4.48(3.45, 5.38) 4.00(3.16, 4.90) -2.023c 0.043 尿酸[M(P25, P75), μmol/L] 355.00(301.75, 440.00) 333.00(274.00, 404.00) -1.716c 0.086 白蛋白(x±s, g/L) 27.84±5.18 29.19±4.72 1.650a 0.099 D-二聚体[M(P25, P75), μg/mL] 3.14(1.24, 6.11) 1.74(1.13, 2.60) -2.820c 0.005 谷丙转氨酶[M(P25, P75), U/L] 20.00(13.75, 33.75) 19.00(13.00, 28.00) -0.723c 0.470 谷草转氨酶[M(P25, P75), U/L] 30.00(18.75, 39.50) 22.00(17.00, 31.00) -2.456c 0.014 纤维蛋白原(x±s, g/L) 3.48±1.06 4.25±1.76 2.533a 0.011 HDP分型[例(%)] 13.425b 0.008 慢性高血压合并妊娠 3(8.82) 159(10.19) 妊娠期高血压 4(11.76) 300(19.22) 轻度子痫前期 7(20.60) 548(35.10) 重度子痫前期 18(52.94) 546(34.98) 子痫 2(5.88) 8(0.51) 注:1 mmHg=0.133 kPa。a为t值,b为χ2值,c为Z值。 表 2 HDP单胎妊娠患者并发胎盘早剥的多因素分析
Table 2. Multifactor analysis of placental abruption in HDP single pregnancy patients
变量 B SE Waldχ2 P值 OR值 95% CI D-二聚体 0.048 0.018 6.905 0.009 1.049 1.012~1.087 纤维蛋白原 -0.707 0.194 13.250 < 0.001 0.493 0.337~0.722 重度子痫前期 0.790 0.370 4.559 0.033 2.204 1.067~4.552 子痫 2.759 0.857 10.356 0.001 15.777 2.940~84.659 注:HDP分型以慢性高血压合并妊娠为参照。 表 3 D-二聚体、纤维蛋白原、HDP分型预测HDP单胎妊娠患者并发胎盘早剥的效能分析
Table 3. Efficacy analysis of D-Dimer, fibrinogen, and HDP subtypes for predicting placental abruption in HDP single pregnancy patients
项目 AUC 95% CI SE P值 灵敏度(%) 特异度(%) D-二聚体 0.641 0.522~0.761 0.061 0.005 50.0 84.2 纤维蛋白原 0.685 0.592~0.777 0.047 < 0.001 55.9 71.1 HDP分型 0.617 0.515~0.720 0.052 0.019 35.5 76.7 D-二聚体+纤维蛋白原 0.705 0.604~0.806 0.052 < 0.001 61.8 77.3 D-二聚体+纤维蛋白原+HDP分型 0.735 0.639~0.831 0.049 < 0.001 14.4 61.5 -
[1] BRANDT J S, ANANTH C V. Placental abruption at near-term and term gestations: pathophysiology, epidemiology, diagnosis, and management[J]. Am J Obstet Gynecol, 2023, 228(5S): S1313-S1329. [2] 段涛, 谢幸, 孔北华. 妇产科学[M]. 9版. 北京: 人民卫生出版社, 2018: 150-153.DUAN T, XIE X, KONG B H. Obstetrics and Gynecology[M]. 9th edition. Beijing: People ' s Medical Publishing House, 2018: 150-153. [3] FOX R, KITT J, LEESON P, et al. Preeclampsia: risk factors, diagnosis, management, and the cardiovascular impact on the offspring[J]. J Clin Med, 2019, 8(10): 1625. DOI: 10.3390/jcm8101625. [4] NARUSE K, SHIGEMI D, HASHIGUCHI M, et al. Placental abruption in each hypertensive disorders of pregnancy phenotype: a retrospective cohort study using a national inpatient database in Japan[J]. Hypertens Res, 2021, 44(2): 232-238. doi: 10.1038/s41440-020-00537-6 [5] PARIENTE G, WAINSTOCK T, WALFISCH A, et al. Placental abruption and long-term neurological hospitalisations in the offspring[J]. Paediatr Perinat Epidemiol, 2019, 33(3): 215-222. doi: 10.1111/ppe.12553 [6] 张为远, 杨孜. 妊娠期高血压疾病诊治指南(2020)[J]. 中华妇产科杂志, 2020, 55(4): 227-238.ZHANG W Y, YANG Z. Guidelines for diagnosis and treatment of hypertensive disorders in pregnancy (2020)[J]. Chin J Obstet Gynecol, 2020, 55(4): 227-238. [7] 冯蜀欢, 林建华. 慢性高血压伴发子痫前期的临床管理[J]. 实用妇产科杂志, 2020, 36(12): 890-893.FENG S H, LIN J H. Clinical management of chronic hypertension complicated with preeclampsia[J]. J Prac Obste Gynecol, 2020, 36(12): 890-893. [8] 季燕雯, 陈先侠, 王海霞, 等. 早发型子痫前期不良妊娠结局的影响因素分析[J]. 实用医学杂志, 2020, 36(12): 1590-1594. doi: 10.3969/j.issn.1006-5725.2020.12.009JI Y W, CHEN X X, WANG H X, et al. Influencing factors of adverse pregnancy outcomes in early onset preeclampsia[J]. J Prac Med, 2020, 36(12): 1590-1594. doi: 10.3969/j.issn.1006-5725.2020.12.009 [9] 徐元元, 许健, 施卫平, 等. 子痫前期孕妇胎盘血流灌注指标预测胎盘早剥的价值及血流灌注指标与胎盘病理评分的相关性[J]. 中国现代医学杂志, 2023, 33(3): 76-82.XU Y Y, XU J, SHI W P, et al. The value of placental blood perfusion indexes in predicting placental abruption and the correlation between placental blood perfusion indexes and placental pathological score in preeclampsia[J]. Chin J Mod Med, 2023, 33(3): 76-82. [10] ROBERGE S, BUJOLD E, NICOLAIDES K H. Meta-analysis on the effect of aspirin use for prevention of preeclampsia on placental abruption and antepartum hemorrhage[J]. Am J Obstet Gynecol, 2018, 218(5): 483-489. doi: 10.1016/j.ajog.2017.12.238 [11] ADANE A A, SHEPHERD C C J, LIM F J, et al. The impact of pre-pregnancy body mass index and gestational weight gain on placental abruption risk: a systematic review and meta-analysis[J]. Arch Gynecol Obstet, 2019, 300(5): 1201-1210. doi: 10.1007/s00404-019-05320-8 [12] SCHUR E, BAUMFELD Y, ROTEM R, et al. Placental abruption: assessing trends in risk factors over time[J]. Arch Gynecol Obstet, 2022, 306(5): 1547-1554. doi: 10.1007/s00404-022-06638-6 [13] GUO Q, FENG P, YU Q, et al. Associations of systolic blood pressure trajectories during pregnancy and risk of adverse perinatal outcomes[J]. Hypertens Res, 2020, 43(3): 227-234. doi: 10.1038/s41440-019-0350-3 [14] FISHEL B M, SIBAI B M. Eclampsia in the 21st century[J]. Am J Obstet Gynecol, 2022, 226(2S): S1237-S1253. [15] BEDELL S, HUTSON J, DE VRIJER B, et al. Effects of maternal obesity and gestational diabetes mellitus on the placenta: current knowledge and targets for therapeutic interventions[J]. Curr Vasc Pharmacol, 2021, 19(2): 176-192. doi: 10.2174/18756212MTA3qNDApy [16] 杨子月. 血清D-二聚体、胎盘生长因子与重度子痫前期患者胎盘早剥的关系分析[J]. 现代诊断与治疗, 2022, 33(3): 425-427.YANG Z Y. Analysis of the relationship between serum D-Dimer, placental growth factor and placental abruption in patients with severe preeclampsia[J]. Modern Diagnosis & Therapy, 2022, 33(3): 425-427. [17] 吴兆晴, 徐金霞. D-二聚体、纤维蛋白原、心肌酶谱在妊娠期糖尿病中的临床意义[J]. 中国现代医学杂志, 2020, 30(3): 97-101.WU Z Q, XU J X. Clinical significance of D-Dimer, fibrinogen and myocardial enzymes in gestational diabetes mellitus[J]. Chin J Modern Med, 2020, 30(3): 97-101. [18] 刘娟, 杨丽珍, 侯凯文. 重度子痫前期患者血清纤维蛋白原、尿素氮、NEP、LRP-1表达水平预测胎盘早剥的临床价值分析[J]. 转化医学杂志, 2022, 11(3): 132-136.LIU J, YANG L Z, HOU K W. Clinical value of serum fibrinogen, urea nitrogen, NEP and LRP-1 expression levels in predicting placental abruption in patients with severe preeclampsia[J]. J Translational Med, 2022, 11(3): 133-136. [19] 朱虹, 宣荣荣, 刘莉萍, 等. 妊娠高血压综合征与妊娠期糖尿病患者凝血功能检测的价值探讨[J]. 中华全科医学, 2019, 17(10): 1711-1713. doi: 10.16766/j.cnki.issn.1674-4152.001037ZHU H, XUAN R R, LIU L P, et al. The value of coagulation function test in patients with pregnancy-induced hypertension syndrome and gestational diabetes mellitus[J]. Chinese Journal of General Practice, 2019, 17(10): 1711-1713. doi: 10.16766/j.cnki.issn.1674-4152.001037 [20] 王晓艳, 陶峰, 陈红波. 35例胎盘早剥患者临床特点及妊娠结局分析[J]. 安徽医学, 2019, 40(11): 1223-1225.WANG X Y, TAO F, CHEN H B. Clinical characteristics and pregnancy outcomes of 35 patients with placental abruption[J]. Anhui Med, 2019, 40(11): 1223-1225. -





 下载:
下载: