The effect of preoperative hand motor nerve conduction velocity and grip strength on prognosis in 85 patients with moderate to severe cubital tunnel syndrome
-
摘要:
目的 探讨85例中重度肘管综合征患者术前手部神经运动传导速度(MNCV)、握力对预后的影响,为其预后的评估提供指导。 方法 收集2021年7月—2023年7月于河北省沧州中西医结合医院治疗的85例中重度肘管综合征患者的病例资料,比较不同肘管综合征分级、不同预后患者的手部MNCV、握力水平,并评估上述指标预测预后不良的价值。 结果 (1) 手术前,重度组患者不同状态下的手部MNCV及握力均较中度组低(P < 0.05);手术后,2组患者上述指标均升高,且中度组较重度组高(P < 0.05);(2)手术后,手部MNCV及握力比较:功能恢复优组>功能恢复良组>功能恢复可组>功能恢复差组,差异有统计学意义(P < 0.05);(3)81例完整随访数据中功能恢复可及差的患者20例(预后不良组),余61例为预后良好组,预后不良组患者不同状态下的手部MNCV及握力均较预后良好组低(P < 0.05);(4)中重度肘管综合征患者不同状态下的手部MNCV及握力预测患者预后不良的效能较高;(5)预后不良组患者年龄≥50岁、病程≥10个月、长期屈肘工作及肌肉萎缩的占比较预后良好组高(P < 0.05);(6)长期屈肘工作及肌肉萎缩是中重度肘管综合征患者预后不良的危险因素(P=0.008、0.001)。 结论 接受治疗后的中重度肘管综合征患者,在不同状态下的手部MNCV及握力均提高,且中度肘管综合征患者上述指标提升更明显,均可作为预测中重度肘管综合征预后的有效指标。 -
关键词:
- 中重度肘管综合征 /
- 手部神经运动传导速度 /
- 握力 /
- 预后
Abstract:Objective To investigate the influence of hand motor nerve conduction velocity (MNCV) and grip strength on prognosis in 85 patients with moderate to severe cubital tunnel syndrome, and to provide guidance for prognosis evaluation. Methods Data of 85 patients with moderate to severe cubital tunnel syndrome treated in Cangzhou Hospital of Integrated Chinese and Western Medicine, Hebei Province from July 2021 to July 2023 were collected. Different cubital tunnel syndrome grades, different prognosis, and grip strength levels were compared, and the value of these indicators in predicting poor prognosis was evaluated. Results (1) Before the operation, the hand MNCV and grip strength in the severe group were lower than those in the moderate group (P < 0.05); After the operation, the above indexes increased in the two groups, and the moderate group was higher (P < 0.05); (2) After the surgery, comparison of hand MNCV and grip strength as follows: Excellent functional recovery group > good functional recovery group > fair functional recovery group > poor functional recovery group, with statistically significant difference (P < 0.05); (3) Among the 81 patients with complete follow-up data, 20 patients had poor functional recovery (poor prognosis group), and the remaining 61 patients were considered as the good prognosis group. The hand MNCV and grip strength in the poor prognosis group were lower under different conditions (P < 0.05); (4) Hand MNCV and grip strength under different conditions of moderate and severe cubital tunnel syndrome were more effective in predicting the poor prognosis of patients. (5) The proportion of patients aged ≥50 years, duration ≥10 months, long-term elbow bending and muscle atrophy in the poor prognosis group was higher than that in the good prognosis group (P < 0.05); (6) Long-term elbow bending and muscle atrophy were risk factors for poor prognosis in patients with moderate to severe cubital tunnel syndrome (P=0.008, 0.001). Conclusion After treatment, the cubital length hand MNCV and grip strength of patients with moderate and severe cubital tunnel syndrome are improved in different states, and the above indexes were improved more significantly in patients with moderate cubital tunnel syndrome, which could be used as effective indicators to predict the prognosis. -
表 1 不同肘管综合征分级患者手术前后不同状态下的手部MNCV及握力比较(x ±s)
Table 1. Comparison of hand MNCV and grip strength in patients with different grades of cubital tunnel syndrome before and after surgery(x±s)
组别 例数 V1(m/s) V2(m/s) V3(m/s) V4(m/s) 握力(N) 手术前 手术后 手术前 手术后 手术前 手术后 手术前 手术后 手术前 手术后 中度组 59 34.52±2.33 42.39±3.42b 33.27±2.16 41.44±2.61b 32.46±2.53 40.62±3.21b 31.76±2.85 40.89±2.82b 23.15±2.76 28.68±2.07b 重度组 26 32.08±2.47 39.76±3.54b 30.38±2.23 38.52±2.78b 29.71±2.64 37.81±3.43b 28.43±2.94 37.97±3.04b 20.08±2.83 24.33±2.34b 统计量 4.368a 3.232c 5.628a 4.659c 4.557a 3.642c 4.916a 4.295c 4.689a 8.576c P值 < 0.001 0.002 < 0.001 < 0.001 < 0.001 0.001 < 0.001 < 0.001 < 0.001 < 0.001 注:a为t值,c为F值;与同组手术前比较,bP < 0.05。 表 2 手术后不同功能恢复程度肘管综合征患者手部MNCV及握力比较(x±s)
Table 2. Comparison of hand MNCV and grip strength in patients with different functional recovery levels after surgery(x±s)
功能恢复情况 例数 V1(m/s) V2(m/s) V3(m/s) V4(m/s) 握力(N) 优 37 43.75±3.11ab 42.52±2.45abc 41.33±3.02ab 41.19±2.77ab 29.37±2.01abc 良 25 42.13±3.49 40.27±2.62 39.86±3.38 40.63±2.84 27.82±2.18 可 16 38.08±3.74 38.35±2.88 37.52±3.46 37.96±2.93 24.43±2.24 差 7 36.21±4.52 36.13±3.43 36.23±3.85 36.08±3.58 21.66±2.61 F值 16.090 16.870 8.027 9.452 37.340 P值 < 0.001 < 0.001 < 0.001 < 0.001 < 0.001 注:与功能恢复可组比较,aP < 0.05;与功能恢复差组比较,bP < 0.05;与功能恢复良组比较,cP < 0.05。 表 3 预后良好组及预后不良组患者不同状态下的手部MNCV及握力比较(x ±s)
Table 3. Comparison of hand MNCV and grip strength in patients with good prognosis and poor prognosis under different conditions(x±s)
组别 例数 V1(m/s) V2(m/s) V3(m/s) V4(m/s) 握力(N) 预后良好组 61 42.46±3.43 41.62±3.51 41.09±3.79 40.74±3.83 28.94±3.34 预后不良组 20 38.52±3.74 37.75±3.78 37.42±3.94 36.48±4.02 23.41±3.52 t值 3.360 4.199 3.722 4.265 6.342 P值 < 0.001 < 0.001 < 0.001 < 0.001 < 0.001 表 4 中重度肘管综合征患者不同状态下的手部MNCV及握力预测中重度肘管综合征预后不良的ROC曲线
Table 4. ROC curve for predicting poor prognosis in patients with moderate to severe cubital tunnel syndrome based on hand MNCV and grip strength in different states
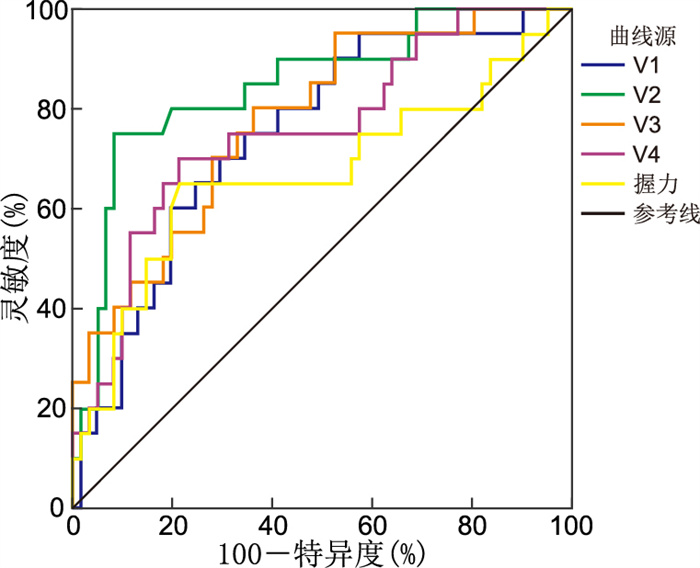
项目 AUC 95% CI P值 cut-off值 Youden指数 灵敏度(%) 特异度(%) V1 0.747 0.638~0.837 < 0.001 ≤40.78 m/s 0.406 75.00 65.57 V2 0.848 0.751~0.918 < 0.001 ≤37.25 m/s 0.668 75.00 91.80 V3 0.776 0.670~0.861 < 0.001 ≤39.97 m/s 0.439 80.00 63.93 V4 0.757 0.649~0.845 < 0.001 ≤37.40 m/s 0.487 70.00 78.69 握力 0.671 0.558~0.771 0.034 ≤25.78 N 0.437 65.00 78.69 表 5 预后良好组与预后不良组一般资料比较[例(%)]
Table 5. Comparison of general data between the good prognosis group and the poor prognosis group[cases (%)]
项目 例数 预后良好组(n=61) 预后不良组(n=20) χ2值 P值 年龄(岁) 5.139 0.023 ≥50 35 22(36.07) 13(65.00) <50 46 39(63.93) 7(35.00) 性别 0.200 0.655 男性 48 37(60.66) 11(55.00) 女性 33 24(39.34) 9(45.00) 病程(月) 11.148 0.001 ≥10 47 29(47.54) 18(90.00) <10 34 32(52.46) 2(10.00) BMI 0.105 0.745 ≤24 39 30(49.18) 9(45.00) >24 42 31(50.82) 11(55.00) 长期屈肘工作 6.972 0.008 是 40 25(40.98) 15(75.00) 否 41 36(59.02) 5(25.00) 肘部外伤史 0.218 0.641 有 15 12(19.67) 3(15.00) 无 66 49(80.33) 17(85.00) 肌肉萎缩 5.039 0.025 是 62 43(70.49) 19(95.00) 否 19 18(29.51) 1(5.00) 振幅(mV) 0.389 0.533 ≥5.0 52 38(62.30) 14(70.00) <5.0 29 23(37.70) 6(30.00) 潜伏期(ms) 0.033 0.855 ≥9.0 54 41(67.21) 13(65.00) <9.0 27 20(32.79) 7(35.00) 表 6 变量赋值情况
Table 6. Assignment of argument variables
变量 赋值方法 年龄 <50岁=0,≥50岁=1 病程 <10个月=0,≥10个月=1 长期屈肘工作 无=0,有=1 肌肉萎缩 否=0,是=1 表 7 中重度肘管综合征患者预后不良的多因素logistic回归分析
Table 7. Multivariate logistic regression analysis of poor prognosis in patients with moderate to severe cubital tunnel syndrome
变量 B SE Waldχ2 P值 OR值 95% CI 年龄 0.739 0.421 3.081 0.080 2.094 0.917~4.779 病程 0.812 0.518 2.457 0.118 2.252 0.816~6.217 长期屈肘工作 0.683 0.257 7.063 0.008 1.980 1.196~3.276 肌肉萎缩 0.727 0.223 10.628 0.001 2.069 1.336~3.203 -
[1] RHODES N G, HOWE B M, FRICK M A, et al. MR imaging of the postsurgical cubital tunnel: an imaging review of the cubital tunnel, cubital tunnel syndrome, and associated surgical techniques[J]. Skeletal Radiol, 2019, 48(10): 1541-1554. doi: 10.1007/s00256-019-03203-2 [2] 张光辉, 张志, 张清林, 等. 高分辨率超声检测尺神经直径在肘管综合征中的应用[J]. 中国骨伤, 2023, 36(6): 550-553.ZHANG G H, ZHANG Z, ZHANG Q L, et al. Application of ulnar nerve diameter changes examined by HRUS in patients with cubital tunnel syndrome[J]. China Journal of Orthopaedics and Traumatology, 2023, 36(6): 550-553. [3] ABOURISHA E, SRINIVASAN AS, BARAKAT A, et al. Surgical management of cubital tunnel syndrome: a systematic review and meta-analysis of randomised trials[J]. J Orthop, 2024, 53: 41-48. doi: 10.1016/j.jor.2024.02.041 [4] 张卫平, 陈莉, 谌芳群, 等. 剪切波弹性成像技术在肘管综合征诊断中的应用价值[J]. 重庆医学, 2021, 50(7): 1113-1116.ZHANG W P, CHEN L, SHEN F Q, et al. Application value of shear wave elastography in diagnosis of cubital tunnel syndrome[J]. Chongqing Medicine, 2021, 50(7): 1113-1116. [5] SHELKE S, AMBADE R, SHELKE A. From conservative measures to surgical interventions, treatment approaches for cubital tunnel syndrome: a comprehensive review[J]. Cureus, 2023, 15(12): e51262. DOI: 10.7759/cureus.51262. [6] 马嘉嘉, 杨晶, 郭金超, 等. 显微镜下微创松解治疗肘管综合征的疗效观察[J]. 中国骨与关节损伤杂志, 2019, 34(3): 317-318.MA J J, YANG J, GUO J C, et al. Observation of the curative effect of microinvasive release on cubital tunnel syndrome[J]. Chinese Journal of Bone and Joint Injury, 2019, 34(3): 317-318. [7] PAPADOPOULOS D V, KOSTAS-AGNANTIS I, KOSMAS D, et al. Ulnar intraneural cysts as a cause of cubital tunnel syndrome: presentation of a case and review of the literature[J]. Eur J Orthop Surg Traumatol, 2019, 29(7): 1559-1563. doi: 10.1007/s00590-019-02475-7 [8] KESSLER R B, THOMPSON R G, LOURIE G M. Cubital tunnel syndrome: a surgical modification to in situ decompression to improve results[J]. JSES Int, 2020, 4(1): 15-20. doi: 10.1016/j.jseint.2019.11.004 [9] 王萍, 张学磊, 余航, 等. 黄芪桂枝五物汤对肘管综合征患者肘管扩大成形术后尺神经运动传导速度和上肢功能的影响[J]. 陕西中医, 2023, 44(12): 1745-1748.WANG P, ZHANG X L, YU H, et al. Effects of Huangqi Guizhi Wuwu decoction on ulnar nerve motor conduction velocity, upper limb function in patients with cubital tunnel syndrome after extended cubital tunnel plasty[J]. Shaanxi Journal of Traditional Chinese Medicine, 2023, 44(12): 1745-1748. [10] 李志强, 江凌, 姚中强, 等. 超声引导下肘管综合征的介入治疗研究[J]. 中国超声医学杂志, 2023, 39(1): 86-89.LI Z Q, JIANG L, YAO Z Q, et al. Ultrasound-guided Interventional Treatment of Cubital Tunnel Syndrome[J]. Chinese Journal of Ultrasound in Medicine, 2023, 39(1): 86-89. [11] 顾玉东. 腕管综合征与肘管综合征诊治中的有关问题[J]. 中华手外科杂志, 2010, 26(6): 321-323.GU Y D. Issues in the diagnosis and treatment of carpal tunnel syndrome and cubital tunnel syndrome[J]. Chinese Journal of Hand Surgery, 2010, 26(6): 321-323. [12] 吴立东, 彭菁, 黄宗坚, 等. 肘管综合征的诊断和治疗[J]. 浙江医学, 2003, 25(1): 44-46.WU L D, PENG J, HUANG Z J, et al. Diagnosis and treatment of cubital tunnel syndrome[J]. Zhejiang Medical Journal, 2003, 25(1): 44-46. [13] PUGDAHL K, TANKISI H, FUGLSANG-FREDERIKSEN A. Electrodiagnostic testing of entrapment neuropathies: a review of existing guidelines[J]. J Clin Neurophysiol, 2020, 37(4): 299-305. doi: 10.1097/WNP.0000000000000668 [14] 顾玉东. 腕管综合征与肘管综合征功能评定标准的现状与建议[J]. 中华创伤骨科杂志, 2011, 13(1): 6-7.GU Y D. Current evaluation criteria for carpal tunnel syndrome and cubital tunnel syndrome[J]. Chinese Journal of Orthopaedic Trauma, 2011, 13(1): 6-7. [15] 户文耀, 李汶霖, 王洋, 等. WALANT麻醉联合小切口原位松解术治疗肘管综合征的疗效分析[J]. 中国骨与关节损伤杂志, 2021, 36(3): 294-296.HU W Y, LI W L, WANG Y, et al. Effect analysis of WALANT anesthesia combined with small incision in situ release in treatment of cubital tunnel syndrome[J]. Chinese Journal of Bone and Joint Injury, 2021, 36(3): 294-296. [16] 赵静, 李世英, 董汉青, 等. 尺神经松解前置术后联合中药治疗重度肘管综合征疗效及对尺神经功能、肘部尺神经运动传导速度的影响[J]. 现代中西医结合杂志, 2021, 30(31): 3501-3504.ZHAO J, LI S Y, DONG H Q, et al. Effect of ulnar nerve release and pretreatment combined with Chinese medicine on severe cubital tunnel syndrome and its influence on ulnar nerve function and ulnar nerve motor conduction velocity of elbow[J]. Journal of Modern Integrated Chinese and Western Medicine, 2021, 30(31): 3501-3504. [17] 高星, 孟玉凤, 王伟, 等. 显微镜下微创松解联合术后口服坚骨胶囊治疗肘管综合征的效果研究[J]. 中华全科医学, 2023, 21(12): 2057-2059, 2063. doi: 10.16766/j.cnki.issn.1674-4152.003289GAO X, MENG Y F, WANG W, et al. Study on the therapeutic effect of minimally invasive release under microscope combined with postoperative oral administration of Jiangu capsules on cubital tunnel syndrome[J]. Chinese Journal of General Practice, 2023, 21(12): 2057-2059, 2063. doi: 10.16766/j.cnki.issn.1674-4152.003289 [18] 肖锋, 劳杰, 赵新. 影响重度肘管综合征术后疗效的相关因素分析[J]. 中华手外科杂志, 2019, 35(3): 206-208.XIAO F, LAO J, ZHAO X. Relevant factors influencing the outcome of severe cubital tunnel syndrome after operation[J]. Chinese Journal of Hand Surgery, 2019, 35(3): 206-208. [19] 齐江明, 宫可同, 李东升, 等. 肘管综合征患者伸肘与屈肘状态下尺神经运动神经传导速度对比研究[J]. 中华手外科杂志, 2019, 35(5): 377-379.QI J M, GONG K T, LI D S, et al. A comparative study of motor nerve conduction velocity of ulnar nerve between elbow extension and elbow flexion in patients with cubital tunnel syndrome[J]. Chinese Journal of Hand Surgery, 2019, 35(5): 377-379. [20] 张磊, 王海林, 刘旋, 等. 尺神经松解前置术治疗肘管综合征的临床疗效及预后的影响因素分析[J]. 局解手术学杂志, 2021, 30(6): 520-524.ZHANG L, WANG H L, LIU X, et al. Clinical efficacy of ulnar nerve release anterior transposition on cubital tunnel syndrome and its influencing factors for prognosis[J]. Journal of Regional Anatomy and Operative Surgery, 2021, 30(6): 520-524. -





 下载:
下载: