Application of uterine artery flow parameters combined with serum alpha-fetoprotein in predicting premature birth in twins
-
摘要:
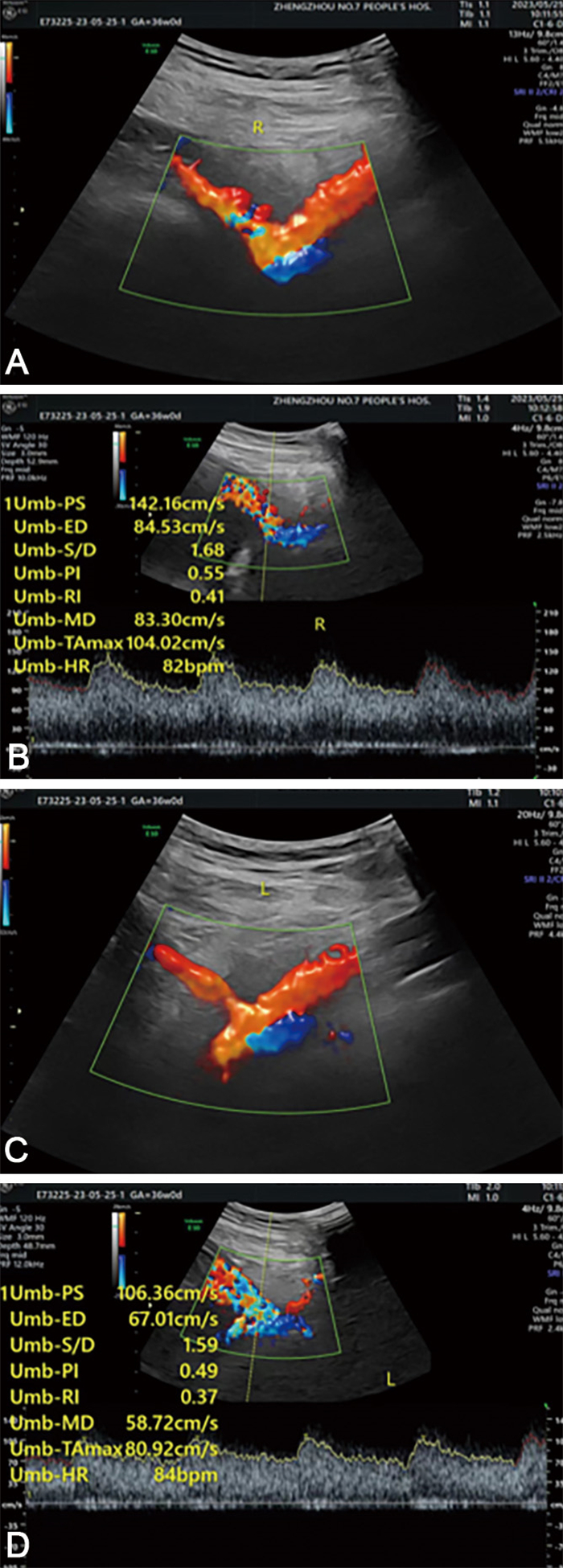
目的 早产(PTB)是新生儿死亡的主要原因,PTB风险较高的双胎孕妇胎盘屏障容易破裂,胎血流入母体,造成母体血清甲胎蛋白(AFP)水平升高。本研究探讨了子宫动脉血流参数联合AFP预测双胎早产的预测价值。 方法 选择2015年1月—2021年4月定期在郑州市第七人民医院产检的100例双胎妊娠孕妇进行回顾性分析,根据妊娠结局分为早产组(51例)和足月组(49例)。通过重复测量方差分析对比孕中期血清AFP水平和子宫动脉血流参数的差异,并且通过logistic回归分析研究二者对双胎妊娠早产结局的预测价值。 结果 随妊娠进展,早产组和足月组子宫动脉搏动指数(PI)、子宫动脉阻力指数(RI)、子宫动脉血流S/D值均逐渐下降,血清AFP水平均逐渐上升,早产组不同孕周子宫动脉血流动力学参数及血清AFP水平均高于同期足月组(P < 0.05)。血清AFP、PI、RI、S/D值及四者联合预测双胎早产的AUC分别为0.952、0.881、0.903、0.919和0.966。Logistic回归分析显示,血清AFP、PI、RI和S/D值是双胎孕妇早产的影响因素(OR值分别为2.746、1.262、1.509、2.158)。 结论 血清AFP水平、PI、RI和S/D值可以联合预测双胎早产,并且提高了单指标的灵敏度和特异度。 Abstract:Objective Preterm birth (PTB) is the main cause of neonatal death. Twins at high risk of PTB are susceptible to placental barrier rupture and fetal blood flow entering the mother, resulting in an increase in maternal serum alpha-fetoprotein (AFP) levels. The purpose of this study was to explore the predictive value of combining uterine artery blood flow parameters with AFP levels in predicting preterm delivery in twins. Methods A total of 100 pregnant women with twin pregnancy who underwent regular antenatal examination in the Seventh People' s Hospital of Zhengzhou from January 2015 to April 2021 were retrospectively analyzed. According to the pregnancy outcome, they were divided into a premature group (n=51) and a term group (n=49). Differences in mid-pregnancy serum AFP levels and uterine artery blood flow parameters were compared through repeated measurement analysis of variance. The predictive value of these factors for premature birth outcomes in twin pregnancies was assessed through logistic regression analysis. Results As progression of pregnancy, uterine artery pulsatility index (uterine artery pulsation index, PI), uterine artery resistance index (uterine artery resistance index, RI), and uterine artery blood flow Scarlett D value decreased, while serum AFP level increased gradually in both the preterm group and term group. The uterine artery hemodynamic parameters and serum AFP levels in the preterm group were higher than those in the term group at various gestational weeks. The AUC values of serum AFP, PI, RI, S/D and their combination were 0.952, 0.881, 0.903, 0.919 and 0.966, respectively. Logistic regression analysis showed that serum AFP, PI, RI and S/D were risk factors for preterm delivery in twin pregnant women (OR=2.746, 1.262, 1.509 and 2.158, respectively). Conclusion The combination of serum AFP levels, PI, RI, and S/D values can effectively predict premature delivery in twin birth, improving the sensitivity and specificity compared to single indicators. -
表 1 2组双胎妊娠孕妇不同孕周血清AFP水平、PI、RI和S/D值比较(x ±s)
Table 1. Comparison of serum AFP levels, PI, RI, and S/D values between two groups of patients at different gestational weeks (x ±s)
组别 例数 S/D 27~29周 30~32周 33~36周 早产组 51 9.42±1.24 9.12±0.47 8.78±0.29 足月组 49 5.43±0.53 5.21±0.58 5.03±0.37 F值 12.342 13.493 13.726 P值 < 0.001 < 0.001 < 0.001 组别 例数 PI 27~29周 30~32周 33~36周 早产组 51 2.62±0.07 2.38±0.36 2.13±0.45 足月组 49 1.95±0.35 1.84±0.27 1.80±0.16 F值 10.216 9.984 9.438 P值 < 0.001 < 0.001 < 0.001 组别 例数 RI 27~29周 30~32周 33~36周 早产组 51 0.78±0.09 0.73±0.05 0.69±0.18 足月组 49 0.55±0.11 0.56±0.15 0.53±0.03 F值 8.767 8.698 9.034 P值 < 0.001 < 0.001 < 0.001 组别 例数 AFP(μg/L) 27~29周 30~32周 33~36周 早产组 51 121.20±7.07 133.63±6.75 151.20±7.07 足月组 49 56.12±5.08 60.68±6.23 70.58±4.21 F值 24.325 29.549 26.839 P值 < 0.001 < 0.001 < 0.001 注:S/D,F时间=11.452,F组别=13.683,F交互=25.301,均P < 0.001;PI,F时间=12.654,F组别=10.935,F交互=15.368,均P < 0.001;RI,F时间=7.632,F组别=8.622,F交互=13.008,均P < 0.001;AFP,F时间=20.658,F组别=12.254,F交互=35.014,均P < 0.001。 表 2 各检测指标对于双胎早产的诊断效能
Table 2. Diagnostic accuracy of various detection indicators for premature twin birth
指标 AUC(95% CI) SE P值 灵敏度
(%)特异度
(%)AFP 0.952(0.927~0.976) 0.012 < 0.001 93.7 96.6 PI 0.881(0.863~0.916) 0.017 < 0.001 83.8 92.0 RI 0.903(0.870~0.937) 0.017 < 0.001 87.5 93.2 S/D 0.919(0.937~0.971) 0.012 < 0.001 94.7 95.2 AFP+PI+RI+S/D 0.966(0.956~0.977) 0.010 < 0.001 95.5 96.7 表 3 双胎妊娠孕妇早产影响因素的logistic回归分析
Table 3. Logistic regression analysis of the factors influencing preterm birth in twin pregnancy
变量 B SE Waldχ2 P值 OR值 95% CI AFP 1.010 0.887 1.297 0.003 2.746 1.968~3.535 PI 0.233 0.199 1.367 0.015 1.262 1.021~3.517 RI 0.411 0.363 1.285 0.011 1.509 1.117~2.941 S/D 0.769 0.712 1.167 0.009 2.158 1.469~3.998 -
[1] WALANI S R. Global burden of preterm birth[J]. Int J Gynaecol Obstet, 2020, 150(1): 31-33. doi: 10.1002/ijgo.13195 [2] CHOI S R, CHOI S J. Afterbirth oral fluid secretory leukocyte protease inhibitor decreased in acute histologic chorioamnionitis in preterm birth[J]. Am J Reprod Immunol, 2023, 90(1): e13733. DOI: 10.1111/aji.13733. [3] OHUMA E O, MOLLER A B, BRADLEY E, et al. National, regional, and global estimates of preterm birth in 2020, with trends from 2010: a systematic analysis[J]. Lancet, 2023, 402(10409): 1261-1271. doi: 10.1016/S0140-6736(23)00878-4 [4] 魏军, 刘彩霞, 崔红, 等. 双胎早产诊治及保健指南(2020年版)[J]. 中国实用妇科与产科杂志, 2020, 36(10): 949-956.WEI J, LIU C X, CUI H, et al. Twins of diagnosis and treatment of premature birth and care guide (2020 edition)[J]. Chinese Journal of Practical Gynecology and Obstetrics, 2020, 36(10): 949-956. [5] 王晓艳, 邵子瑜, 杭春梅, 等. 孕中期血清甲胎蛋白和游离β-人绒毛膜促性腺激素对瘢痕子宫孕妇发生胎盘植入性疾病的预测价值[J]. 中华实用诊断与治疗杂志, 2022, 36(5): 505-508.WANG X Y, SHAO Z Y, HANG C M, et al. The predictive value of serum alpha-fetoprotein and free human chorionic gonadotropin in the second trimester for placental accretion disease in pregnant women with cicatricidal uterus[J]. Journal of Chinese Practical Diagnosis and Therapy, 2022, 36(5): 505-508. [6] CELIK E, MELEKOG ˇ LU R, BAYGVL A, et al. The predictive value of maternal serum AFP to PAPP-A or b-hCG ratios in spontaneous preterm birth[J]. J Obstet Gynaecol, 2022, 42(6): 1956-1961. doi: 10.1080/01443615.2022.2055452 [7] 胡青铮, 姚艳红, 周丽娜. 孕中期血清AFP F-β-hCG联合uE3检测对双胎妊娠母婴不良妊娠结局的预测价值[J]. 中国妇幼保健, 2021, 36(15): 3484-3487.HU Q Z, YAO Y H, ZHOU L N. Value of serum AFP F-β-hCG combined with uE3 detection in predicting adverse pregnancy outcomes in twin pregnancy[J]. Maternal & Child Health Care of China, 2021, 36(15): 3484-3487. [8] 张军, 刘娟, 胡金绘, 等. 血浆少突胶质细胞髓鞘糖蛋白水平变化在诊断早产儿脑损伤中的价值[J]. 中华全科医学, 2021, 19(1): 69-72. doi: 10.16766/j.cnki.issn.1674-4152.001733ZHANG J, LIU J, HU J H, et al. The value of plasma oligodendrocyte myelin glycoprotein level in the diagnosis of brain injury in premature infants[J]. Chinese Journal of General Practice, 2021, 19(1): 69-72. doi: 10.16766/j.cnki.issn.1674-4152.001733 [9] STOYE D Q, BOARDMAN J P, OSMOND C, et al. Preterm birth and infant diurnal cortisol regulation[J]. Arch Dis Child Fetal Neonatal Ed, 2022, 107(5): 565-567. doi: 10.1136/archdischild-2021-323296 [10] 付杰, 魏广友, 郑爱华, 等. 经鼻间歇正压通气联合枸橼酸咖啡因治疗早产儿呼吸暂停疗效分析[J]. 中华全科医学, 2023, 21(4): 626-628, 645. doi: 10.16766/j.cnki.issn.1674-4152.002946FU J, WEI G Y, ZHENG A H, et al. Effect of nasal intermittent positive pressure ventilation combined with caffeine citrate on premature infants with apnea[J]. Chinese Journal of General Practice, 2023, 21(4): 626-628, 645. doi: 10.16766/j.cnki.issn.1674-4152.002946 [11] 武俊宝, 刘玉霞, 李超, 等. 产房内复苏质量改进对胎龄 < 32周早产儿近期临床结局的影响[J]. 新乡医学院学报, 2022, 39(8): 735-740.WU J B, LIU Y X, LI C, et al. Effect of improved resuscitation quality in delivery room on short-term clinical outcomes of preterm infants < 32 weeks gestational age[J]. Journal of Xinxiang Medical University, 2022, 39(8): 735-740. [12] 傅旭明, 黄烈平, 韩宜姚, 等. 不同维持剂量枸橼酸咖啡因在早产儿呼吸暂停中的应用对比观察[J]. 中华全科医学, 2021, 19(12): 2065-2067, 2076. doi: 10.16766/j.cnki.issn.1674-4152.002238FU X M, HUANG L P, HAN Y Y, et al. Comparative observation of different maintenance doses of caffeine citrate in premature infants with apnea[J]. Chinese Journal of General Practice, 2022, 19(12): 2065-2067, 2076. doi: 10.16766/j.cnki.issn.1674-4152.002238 [13] LI C J, CAO M S, ZHOU X. Role of epigenetics in parturition and preterm birth[J]. Biol Rev Camb Philos Soc, 2022, 97(3): 851-873. doi: 10.1111/brv.12825 [14] ROMAN A, RAMIREZ A, FOX N S. Screening for preterm birth in twin pregnancies[J]. Am J Obstet Gynecol MFM, 2022, 4(2S): 100531. DOI: 10.1016/j.ajogmf.2021.100531. [15] WANG Z Y, ZHAO S L, CUI X Y, et al. Effects of dietary patterns during pregnancy on preterm birth: a birth cohort study in Shanghai[J]. Nutrients, 2021, 13(7): 2367. DOI: 10.3390/nu13072367. [16] 刘小燕, 胡敏华, 刘春兰. 超声测量子宫颈管长度、子宫动脉血流动力学以及生化标志物预测早产的研究[J]. 中国医学创新, 2021, 18(10): 58-62.LIU X Y, HU M H, LIU C L. Study of ultrasound measurement of cervical canal length, uterine artery hemodynamics and biochemical markers for prediction of preterm birth[J]. Medical Innovation of China, 2021, 18(10): 58-62. -





 下载:
下载: