Causal relationship between fasting plasma glucose and coronary heart disease based on two-sample mendelian randomization
-
摘要:
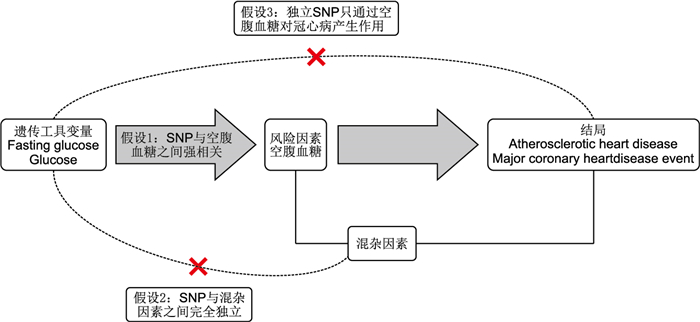
目的 使用两样本孟德尔随机化分析探讨空腹血糖与冠心病之间是否存在因果关系,为冠心病临床防治提供依据。 方法 运用两样本孟德尔随机化分析,以P < 5×10-8,距离10 000 kb,r2 < 0.001为筛选标准,从欧洲血统全基因组关联研究(GWAS)的数据集中提取与冠心病和空腹血糖密切相关的单核苷酸多态性(SNP)作为工具变量,分析空腹血糖(n=200 622)与冠心病(12 171例病例和450 839例对照)的因果关系。使用来自其他数据集的GWAS数据(空腹血糖:n=24 679;冠心病:43 518例病例和333 759例对照)进行重复孟德尔随机化分析,以验证结果的可靠性。使用逆方差加权法(IVW)作为主要分析方法,并进行敏感性分析以评估结果的稳健性。 结果 IVW结果证明较高的空腹血糖水平增加冠心病的发生风险(OR=1.007,95% CI:1.002~1.013,P=0.010)。重复分析也发现了类似的趋势(OR=1.202,95% CI:1.086~1.329,P < 0.001)。敏感性分析显示孟德尔随机化估计是稳健的。 结论 对欧洲人群的孟德尔随机化分析表明,空腹血糖与冠心病的发生之间存在因果关联,在临床实践中合理控制空腹血糖有利于预防冠心病和相关并发症。 Abstract:Objective Using two-sample mendelian randomization analysis to investigate the causal relationship between fasting plasma glucose and coronary heart disease, and to provide a basis for clinical prevention and treatment of coronary heart disease. Methods The causal relationship between fasting plasma glucose and coronary heart disease was analyzed using a two-sample Mendelian randomization approach with stringent selection criteria (P < 5×10-8, a distance of 10 000 kb, and r2 < 0.001). To identify instrumental variables closely associated with coronary heart disease and fasting plasma glucose in a European ancestry genome-wide association studies (GWAS) dataset, we extracted SNPs. This analysis included 200 622 fasting plasma glucose samples and 12 171 coronary heart disease cases with 450 839 controls. To validate the results, a repeated Mendelian randomization analysis was conducted using GWAS data from other datasets (fasting plasma glucose: n=24 679; coronary heart disease: 43 518 cases, and 333 759 controls). The primary analytical method used was the inverse variance-weighted method (IVW), and sensitivity analyses were performed to assess the robustness of the Mendelian randomization results. Results The IVW analysis strongly supports that higher fasting plasma glucose levels increase the risk of coronary heart disease (OR=1.007, 95% CI: 1.002-1.013, P=0.010). Similar trends were observed in the repeated analyses (OR=1.202, 95% CI: 1.086-1.329, P < 0.001). Sensitivity analyses further reinforce the robustness of the Mendelian randomization estimates. Conclusion Mendelian randomization analysis in the European population indicates a causal relationship between fasting plasma glucose and increased coronary heart disease risk. Clinically managing fasting plasma glucose levels within reason may be beneficial in preventing coronary heart disease and its related complications. -
表 1 纳入研究的SNP敏感性分析
Table 1. Sensitive analysis of the SNPs in this study
通过MR-PRESSO剔除异常SNP 异质性检验MR-Egger 异质性检验IVW 多效性检验MR-Egger 多效性检验
PRESSO(P值)Q Q-df Q-pval Q Q-df Q-pval 截距 SE P值 剔除异常SNP前 91.44 55 0.001 93.31 56 0.001 -0.000 1 0.000 1 0.294 0.001 剔除异常SNP后 61.00 52 0.184 61.34 53 0.202 -5.48×10-5 0.000 1 0.595 0.180 表 2 重复验证的MR分析结果
Table 2. MR analysis results of the repeated validation analysis Table 2 MR analysis results of the repeated validation
MR方法 OR值 95% CI P值 Cochran’s Q
检验P值MR-Egger
截距P值IVW 1.202 1.086~1.329 < 0.001 0.539 MR-Egger 1.232 0.846~1.793 0.390 0.342 0.905 Weighted median 1.220 1.078~1.380 0.002 Weighted mode 1.232 1.071~1.418 0.062 Simple mode 1.229 1.048~1.440 0.085 -
[1] SHAYA G E, LEUCKER T M, JONES S R, et al. Coronary heart disease risk: low-density lipoprotein and beyond[J]. Trends Cardiovasc Med, 2022, 32(4): 181-194. doi: 10.1016/j.tcm.2021.04.002 [2] GUTIÉRREZ-CUEVAS J, SANTOS A, ARMENDARIZ-BORUNDA J. Pathophysiological molecular mechanisms of obesity: a link between MAFLD and NASH with cardiovascular diseases[J]. Int J Mol Sci, 2021, 22(21): 11629. DOI: 10.3390/ijms222111629. [3] KASE N G, GRETZ FRIEDMAN E, BRODMAN M, et al. The midlife transition and the risk of cardiovascular disease and cancer part Ⅰ: magnitude and mechanisms[J]. Am J Obstet Gynecol, 2020, 223(6): 820-833. doi: 10.1016/j.ajog.2020.05.051 [4] 杨玲, 杜雪平. 社区规范管理的稳定性冠心病患者生活质量研究[J]. 中华全科医学, 2023, 21(11): 1898-1902.YANG L, DU X P. Research on the quality of life in patients with stable coronary artery disease under standardized management in community[J]. Chinese Journal of General Practice, 2023, 21(11): 1898-1902. [5] HASBANI N R, LIGTHART S, BROWN M R, et al. American heart association ' s life ' s simple 7: lifestyle recommendations, polygenic risk, and lifetime risk of coronary heart disease[J]. Circulation, 2022, 145(11): 808-818. doi: 10.1161/CIRCULATIONAHA.121.053730 [6] CAI X, XUE Z, ZENG F F, et al. Population serum proteomics uncovers a prognostic protein classifier for metabolic syndrome[J]. Cell Rep Med, 2023, 4(9): 101172. DOI: 10.1016/j.xcrm.2023.101172. [7] SU W Y, CHEN S C, HUANG Y T, et al. Comparison of the effects of fasting glucose, hemoglobin A(1c), and triglyceride-glucose index on cardiovascular events in type 2 diabetes mellitus[J]. Nutrients, 2019, 11(11): 2838. DOI: 10.3390/nu11112838. [8] LIU X, WU S, SONG Q, et al. Reversion from pre-diabetes mellitus to normoglycemia and risk of cardiovascular disease and all-cause mortality in a chinese population: a prospective cohort study[J]. J Am Heart Assoc, 2021, 10(3): e019045. DOI: 10.1161/JAHA.120.019045. [9] JIN Y, XU Z, ZHANG Y, et al. Serum/plasma biomarkers and the progression of cardiometabolic multimorbidity: a systematic review and meta-analysis[J]. Front Public Health, 2023, 11: 1280185. DOI: 10.3389/fpubh.2023.1280185. [10] BOWDEN J, HOLMES M V. Meta-analysis and mendelian randomization: a review[J]. Res Synth Methods, 2019, 10(4): 486-496. doi: 10.1002/jrsm.1346 [11] BIRNEY E. Mendelian randomization[J]. Cold Spring Harb Perspect Med, 2022, 12(4): a041302. DOI: 10.1101/cshperspect.a041302. [12] WU Y, ZHANG C Y, LIU X, et al. Shared genetic architecture and causal relationship between sleep behaviors and lifespan[J]. Transl Psychiatry, 2024, 14(1): 108. DOI: 10.1038/s41398-024-02826-x. [13] HEMANI G, ZHENG J, ELSWORTH B, et al. The MR-Base platform supports systematic causal inference across the human phenome[J]. Elife, 2018, 7: e34408. DOI: 10.7554/eLife.34408. [14] CHEN J, SPRACKLEN C N, MARENNE G, et al. The trans-ancestral genomic architecture of glycemic traits[J]. Nat Genet, 2021, 53(6): 840-860. doi: 10.1038/s41588-021-00852-9 [15] KETTUNEN J, DEMIRKAN A, WVRTZ P, et al. Genome-wide study for circulating metabolites identifies 62 loci and reveals novel systemic effects of LPA[J]. Nat Commun, 2016, 7: 11122. DOI: 10.1038/ncomms11122. [16] KURKI M I, KARJALAINEN J, PALTA P, et al. FinnGen provides genetic insights from a well-phenotyped isolated population[J]. Nature, 2023, 613(7944): 508-518. doi: 10.1038/s41586-022-05473-8 [17] LUO J, LE CESSIE S, VAN HEEMST D, et al. Diet-derived circulating antioxidants and risk of coronary heart disease: a mendelian randomization study[J]. J Am Coll Cardiol, 2021, 77(1): 45-54. doi: 10.1016/j.jacc.2020.10.048 [18] MENG L, WANG Z, MING Y C, et al. Are micronutrient levels and supplements causally associated with the risk of Alzheimer ' s disease? A two-sample Mendelian randomization analysis[J]. Food Funct, 2022, 13(12): 6665-6673. doi: 10.1039/D1FO03574F [19] HE S, PENG Y, CHEN X, et al. Causality between inflammatory bowel disease and the cerebral cortex: insights from Mendelian randomization and integrated bioinformatics analysis[J]. Front Immunol, 2023, 14: 1175873. DOI: 10.3389/fimmu.2023.1175873. [20] WU Y, KONG X J, JI Y Y, et al. Serum electrolyte concentrations and risk of atrial fibrillation: an observational and mendelian randomization study[J]. BMC Genomics, 2024, 25(1): 280. DOI: 10.1186/s12864-024-10197-2. [21] QIN P, QIN T, LIANG L, et al. The role of mitochondrial DNA copy number in cardiometabolic disease: a bidirectional two-sample mendelian randomization study[J]. Cardiovasc Diabetol, 2024, 23(1): 45. DOI: 10.1186/s12933-023-02074-1. [22] WENZL F A, AMBROSINI S, MOHAMMED S A, et al. Inflammation in metabolic cardiomyopathy[J]. Front Cardiovasc Med, 2021, 8: 742178. DOI: 10.3389/fcvm.2021.742178. [23] 王凯阳, 刘凤双, 刘永国, 等. 代谢综合征及各组分与急性心肌梗死患者冠状动脉病变程度及临床结局的相关性研究[J]. 中华全科医学, 2024, 22(2): 212-216, 239.WANG K Y, LIU F S, LIU Y G, et al. The correlation between metabolic syndrome and its components with the degree of coronary artery stenosis and clinical outcomes in patients with acute myocardial infarction[J]. Chinese Journal of General Practice, 2024, 22(2): 212-216, 239. [24] 林小梅, 祖姆热提·阿布都克依木, 马春晖, 等. 血清白介素6、空腹血糖水平与冠心病及不良心血管事件关系的研究[J]. 中国全科医学, 2024, 27(3): 286-292.LIN X M, ZUMURETI A B D K Y M, MA C H, et al. Study on the correlation of serum interleukin-6 and fasting blood glucose with coronary heart disease and adverse cardiovascular events[J]. Chinese General Practice, 2024, 27(3): 286-292. [25] HOU X Z, LV Y F, LI Y S, et al. Association between different insulin resistance surrogates and all-cause mortality in patients with coronary heart disease and hypertension: NHANES longitudinal cohort study[J]. Cardiovasc Diabetol, 2024, 23(1): 86. DOI: 10.1186/s12933-024-02173-7. [26] MARZIANO C, GENET G, HIRSCHI K K. Vascular endothelial cell specification in health and disease[J]. Angiogenesis, 2021, 24(2): 213-236. doi: 10.1007/s10456-021-09785-7 [27] BAI B, YANG Y, WANG Q, et al. NLRP3 inflammasome in endothelial dysfunction[J]. Cell Death Dis, 2020, 11(9): 776. DOI: 10.1038/s41419-020-02985-x. [28] 蔡宇豪, 惠波, 宋小龙, 等. 血管内皮生长因子基因多态性与冠心病患者冠状动脉多支病变的相关性研究[J]. 实用心脑肺血管病杂志, 2024, 32(2): 43-47.CAI Y H, HUI B, SONG X L, et al. Correlation between Vascular Endothelial Growth Factor Gene Polymorphism and Coronary Multi-vessel Disease in Patients with Coronary Heart Disease[J]. Practical Journal of Cardiac Cerebral Pneumal and Vascular Disease, 2024, 32(2): 43-47. [29] KLEIN K R, FRANEK E, MARSO S, et al. Hemoglobin glycation index, calculated from a single fasting glucose value, as a prediction tool for severe hypoglycemia and major adverse cardiovascular events in DEVOTE[J]. BMJ Open Diabetes Res Care, 2021, 9(2): e002339. DOI: 10.1136/bmjdrc-2021-002339. [30] HE Y, LI Z, YU L, et al. Association between the atherogenic index of plasma and carotid artery plaques in patients with coronary heart disease in different glucose metabolism states: an RCSCD-TCM study in Tianjin, China[J]. Endocrine, 2023, 81(2): 252-261. doi: 10.1007/s12020-023-03389-5 [31] VERHEUGT F W A, TEN BERG J M, STOREY R F, et al. Antithrombotics: from aspirin to DOACs in coronary artery disease and atrial fibrillation (Part 3/5)[J]. J Am Coll Cardiol, 2019, 74(5): 699-711. doi: 10.1016/j.jacc.2019.02.080 [32] RAI A K, LEE B, GOMEZ R, et al. Current status and potential therapeutic strategies for using non-coding rna to treat diabetic cardiomyopathy[J]. Front Physiol, 2020, 11: 612722. DOI: 10.3389/fphys.2020.612722. -





 下载:
下载: