The effect of problem-solving therapy on depressive symptoms and cognitive flexibility in patients with primary moderate to severe depression
-
摘要:
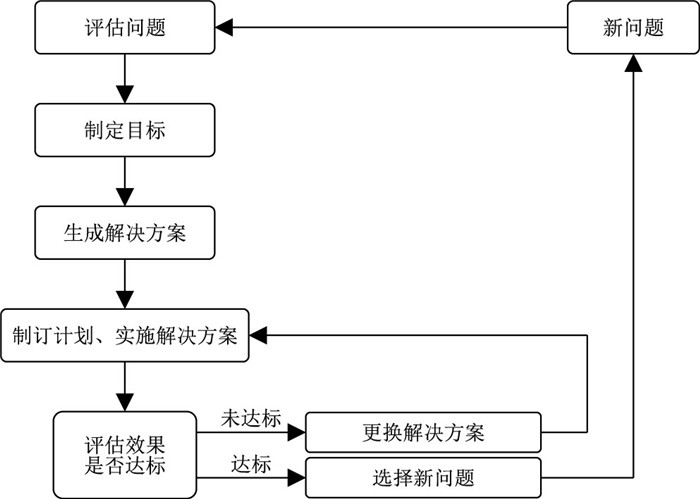
目的 分析在常规护理基础上应用问题解决疗法干预在首发抑郁症患者中的应用效果,及对患者抑郁症状和认知灵活性的影响。 方法 选取2021年2月—2023年10月绍兴市第七人民医院收治的126例首发中重度抑郁症患者作为研究对象,采用随机数字表法将其分为对照组(63例)和观察组(63例)。对照组应用常规护理,观察组在对照组基础上应用问题解决疗法。比较2组患者干预前后抑郁症状[汉密尔顿抑郁量表24项(HAMD-24)]及认知灵活性[认知灵活性问卷(CFI)]。 结果 干预后,2组患者HAMD-24量表评分中各维度及总分均较干预前有所降低,观察组总分为(17.84±2.73)分,明显低于对照组[(20.15±3.16)分],差异有统计学意义(P < 0.05);干预后,观察组患者CFI量表中可选择性、可控性及总分分别为(51.81±6.22)分、(18.91±2.74)分、(71.31±7.40)分,均高于对照组[(42.53±4.37)分、(15.72±2.83)分、(60.22±6.83)分],差异均有统计学意义(P < 0.05)。 结论 问题解决疗法能在常规治疗及护理的基础上改善首发中重度抑郁症患者抑郁症状,提高患者认知灵活性,具有一定的临床价值。 Abstract:Objective To analyze the application effect of problem-solving therapy intervention on the basis of routine nursing in patients with first-episode depression, and its impact on patients' depressive symptoms and cognitive flexibility. Methods A total of 126 patients with first-episode moderate to severe depression admitted to the Seventh People' s Hospital of Shaoxing City from February 2021 to October 2023 were selected as the study subjects, and they were divided into the control group (63 cases) and the observation group (63 cases) according to the method of randomized numerical table. The control group accepted routine nursing intervention, while the observation group accepted problem-solving therapy nursing on the basis of the control group. The depressive symptoms [Hamilton depression scale-24 items (HAMD-24)] and cognitive flexibility [cognitive flexibility inventory (CFI)] were compared between two groups of patients. Results After the intervention, the scores of each dimension and total score in the HAMD-24 scale of the two groups of patients decreased compared to before the intervention, and the total score of the observation group was (17.84±2.73) points, clearly less than that of the control group [(20.15±3.16) points], with statistical significance (P < 0.05). After intervention, the selectivity, controllability, and total score of the CFI scale in the observation group were (51.81±6.22) points, (18.91±2.74) points, and (71.31±7.40) points, respectively, which were higher than those in the control group [(42.53±4.37) points, (15.72±2.83) points, and (60.22±6.83) points], with statistical significance (P < 0.05). Conclusion Problem solving therapy nursing can improve the depressive symptoms and cognitive flexibility of first-onset moderate to severe depression patients on the basis of routine treatment and nursing, and has certain clinical value. -
表 1 2组抑郁症患者一般情况比较
Table 1. Comparison of the general information between two groups of depression patients
项目 对照组(n=63) 观察组(n=63) 统计量 P值 性别(例) 0.835a 0.361 男性 22 27 女性 41 36 年龄(x±s,岁) 38.42±8.16 37.91±7.49 0.365b 0.715 文化水平(例) 1.303c 0.521 初中及以下 7 5 中专/高中 22 28 大专及以上 34 30 经济水平(例) 0.493c 0.782 较好 22 25 一般 33 32 困难 8 6 病程时间(x±s,月) 10.76±3.58 11.01±4.12 0.364b 0.717 抑郁程度(例) 0.904a 0.342 中度 40 45 重度 23 18 艾司西酞普兰用量(x±s,mg) 15.63±3.11 15.70±2.24 0.145b 0.885 注:a为χ2值,b为t值,c为Z值。 表 2 2组抑郁症患者抑郁症状得分比较(x±s,分)
Table 2. Comparison of depression symptom scores between two groups of patients(x±s, points)
组别 例数 认知障碍 迟缓 绝望感 体重变化 干预前 干预后 干预前 干预后 干预前 干预后 干预前 干预后 对照组 63 9.87±1.14 6.05±1.04b 8.76±1.36 3.13±1.25b 6.95±1.52 2.44±0.51b 2.14±0.60 1.87±0.42 观察组 63 10.01±1.33 4.21±0.78b 8.88±1.41 2.72±0.77b 7.02±2.03 1.57±0.23b 2.20±0.55 1.86±0.38 统计量 0.634a 9.382c 0.486a 2.201c 0.219a 10.793c 1.268a 0.152c P值 0.527 < 0.001 0.628 0.032 0.827 < 0.001 0.207 0.834 组别 例数 焦虑/躯体化 日夜变化 睡眠障碍 总分 干预前 干预后 干预前 干预后 干预前 干预后 干预前 干预后 对照组 63 12.31±1.56 4.03±1.24b 1.75±0.39 0.94±0.35b 5.10±1.00 2.22±0.34b 29.83±4.55 20.15±3.16b 观察组 63 12.38±2.11 2.51±0.78b 1.81±0.46 0.76±0.22b 5.04±1.17 1.65±0.26b 30.13±3.81 17.84±2.73b 统计量 0.212a 6.966c 0.790a 3.156c 0.309a 9.873c 0.401a 4.247c P值 0.833 < 0.001 0.431 0.002 0.758 < 0.001 0.689 < 0.001 注:a为t值,c为F值;与同组干预前比较,bP < 0.05。 表 3 2组抑郁症患者认知灵活性得分对比(x±s,分)
Table 3. Comparison of cognitive flexibility scores between two groups of depressed patients (x±s, points)
组别 例数 可选择性 可控性 总分 干预前 干预后 干预前 干预后 干预前 干预后 对照组 63 34.18±5.70 42.53±4.37b 15.81±2.66 15.72±2.83 51.28±7.46 60.22±6.83b 观察组 63 34.52±5.22 51.81±6.22b 16.02±3.11 18.91±2.74b 51.42±8.15 71.31±7.40b 统计量 0.349a 8.793c 0.407a 5.922c 0.101a 8.031c P值 0.728 < 0.001 0.684 < 0.001 0.920 < 0.001 注:a为t值,c为F值;与同组干预前比较,bP < 0.05。 -
[1] 王媛媛, 甘建光, 陈晶, 等. 失效模式与效应分析风险管理在住院抑郁症患者自杀预防中的应用[J]. 中华全科医学, 2024, 22(4): 633-637. doi: 10.16766/j.cnki.issn.1674-4152.003468WANG Y Y, GAN J G, CHEN J, et al. The application of failure mode and effect analysis in risk management for suicide prevention in hospitalized patients with depression[J]. Chinese Journal of General Practice, 2024, 22(4): 633-637. doi: 10.16766/j.cnki.issn.1674-4152.003468 [2] 卢翔宇, 尚东旭, 郭玉芳, 等. 自助干预模式在成年抑郁症患者中应用效果的范围综述[J]. 中国实用护理杂志, 2023, 39(7): 555-561.LU X Y, SHANG D X, GUO Y F, et al. Scoping review of application effects of self-help intervention model in adult patients with depression[J]. Chinese Journal of Practical Nursing, 2023, 39(7): 555-561. [3] 胡洁琼, 季蕴辛, 戴霓, 等. 首发抑郁症住院患者低体质量率及其影响因素[J]. 浙江临床医学, 2022, 24(8): 1182-1183, 1186.HU J Q, JI Y X, DAI N, et al. Low body mass rate and its influencing factors in hospitalized patients with first episode depression[J]. Zhejiang Clinical Medical Journal, 2022, 24(8): 1182-1183, 1186. [4] 梅冬蕾, 吴艳坤, 陈超, 等. 青年女性进食障碍患者的认知灵活性[J]. 中国心理卫生杂志, 2023, 37(4): 273-278.MEI D L, WU Y K, CHEN C, et al. Cognitive flexibility in young female patients with eating disorders[J]. Chinese Mental Health Journal, 2023, 37(4): 273-278. [5] 高玉梅, 李瀛均, 耿文怡, 等. 问题解决疗法对慢性心力衰竭患者心理状态及自护能力的影响[J]. 海南医学, 2022, 33(3): 405-408.GAO Y M, LI Y J, GENG W Y, et al. Effects of problem solving therapy on psychological status and self-care ability of patients with chronic heart failure[J]. Hainan Medical Journal, 2022, 33(3): 405-408. [6] NIELSEN T L, HOLST-STENSBORG H W, NIELSEN L M, et al. Strengthening problem-solving skills through occupational therapy to improve older adults' occupational performance: a systematic review[J]. Scand J Occup Ther, 2023, 30(1): 1-13. doi: 10.1080/11038128.2022.2112281 [7] FIEGL S, LAHMANN C, O' ROURKE T, et al. Depression according to ICD-10 clinical interview vs. depression according to the epidemiologic studies depression scale to predict pain therapy outcomes[J]. Front Psychol, 2019, 10: 1862. DOI: 10.3389/fpsyg.2019.01862. [8] 杨树勤. 卫生统计学[M]. 3版. 北京: 人民卫生出版社, 1999: 148.YANG S Q. Health Statistics[M]. 3th edition. Beijing: People' s Medical Publishing House, 1999: 148. [9] BECH P. The responsiveness of the different versions of the Hamilton depression scale[J]. World Psychiatry, 2015, 14(3): 309-310. doi: 10.1002/wps.20248 [10] OSHIRO K, NAGAOKA S, SHINIZU E. Development and validation of the Japanese version of cognitive flexibility scale[J]. BMC Res Notes, 2016, 9: 275. DOI: 10.1186/s13104-016-2070-y. [11] BLUMBERGER D M, MULSANT B H, THORPE K E, et al. Effectiveness of standard sequential bilateral repetitive transcranial magnetic stimulation vs bilateral theta burst stimulation in older adults with depression: the FOUR-D randomized noninferiority clinical trial[J]. JAMA Psychiatry, 2022, 79(11): 1065-1073. doi: 10.1001/jamapsychiatry.2022.2862 [12] NIKOLAC PERKOVIC M, GREDICAK M, SAGUD M, et al. The association of brain-derived neurotrophic factor with the diagnosis and treatment response in depression[J]. Expert Rev Mol Diagn, 2023, 23(4): 283-296. doi: 10.1080/14737159.2023.2200937 [13] 吴孝琦, 孙倩, 段应龙, 等. 问题解决疗法对老年抑郁患者干预效果的Meta分析[J]. 中国实用护理杂志, 2022, 38(2): 154-161.WU X Q, SUN Q, DUAN Y L, et al. Meta-analysis for the effects of problem solving therapy on the elderly patients with depression[J]. Chinese Journal of Practical Nursing, 2022, 38(2): 154-161. [14] KRAUSE K R, COURTNEY D B, CHAN B W C, et al. Problem-solving training as an active ingredient of treatment for youth depression: a scoping review and exploratory meta-analysis[J]. BMC Psychiatry, 2021, 21(1): 397. DOI: 10.1186/s12888-021-03260-9. [15] 陈红, 王立钢, 陈娇, 等. 问题解决疗法对首发老年抑郁症患者临床疗效、认知及社会功能的影响[J]. 中华行为医学与脑科学杂志, 2024, 33(1): 45-50.CHEN H, WANG L G, CHEN J, et al. Effect of problem-solving therapy on clinical efficacy, cognitive and social function in senile patients with first episode depression[J]. Chinese Journal of Behavioral Medicine and Brain Science, 2024, 33(1): 45-50. [16] APOLINÁRIO-HAGEN J, DRÜGE M, FRITSCHE L. Cognitive behavioral therapy, mindfulness-based cognitive therapy and acceptance commitment therapy for anxiety disorders: integrating traditional with digital treatment approaches[J]. Adv Exp Med Biol, 2020: 1191: 291-329. [17] 谷宇昂, 贾淑蕾, 张淼, 等. 失眠障碍伴抑郁状态与失眠障碍患者的静息态脑镜像同伦连接分析[J]. 中华实用诊断与治疗杂志, 2024, 38(8): 768-772.GU Y A, JIA S L, ZHANG M, et al. Analysis of interhemispheric voxel-mirrored homotopic connectivity in resting-state functional magnetic resonance imaging in insomnia disorder patients complicated with or without depressive symptoms[J]. Journal of Chinese Practical Diagnosis and Therapy, 2024, 38(8): 768-772. [18] 赵丹丹, 刘梅红, 陆希. 积极心理干预对经内镜逆行胰胆管造影围术期胰腺炎患者情绪的影响[J]. 中国临床研究, 2024, 37(11): 1798-1802.ZHAO D D, LIU M H, LU X. Effect of positive psychological intervention on the emotions of perioperative pancreatitis patients undergoing endoscopic retrograde cholangiopancreatography[J]. Chinese Journal of Clinical Research, 2024, 37(11): 1798-1802. [19] VIEIRA W F, IOSIFESCU D V, MCEACHERN K M, et al. Photobiomodulation: an emerging treatment modality for depression[J]. Psychiatr Clin North Am, 2023, 46(2): 331-348. [20] 傅菊萍, 陈松, 支倩娜, 等. 认知行为健康教育模式对抑郁症患者自我效能感、应对方式和生活质量的干预效果[J]. 中国基层医药, 2022, 29(5): 777-780.FU J P, CHEN S, ZHI Q N, et al. Effects of a cognitive, behavioral, health education model on self-efficacy, coping style, and quality of life in patients with depression[J]. Chinese Journal of Primary Medicine and Pharmacy, 2022, 29(5): 777-780. -





 下载:
下载: